Korean J Neurotrauma.
2019 Oct;15(2):143-149. 10.13004/kjnt.2019.15.e19.
Changes of Biomarkers before and after Antibiotic Treatment in Spinal Infection
- Affiliations
-
- 1Department of Neurosurgery, Chungnam National University Hospital, Daejeon, Korea. Jeongwook.lim@gmail.com
- KMID: 2461119
- DOI: http://doi.org/10.13004/kjnt.2019.15.e19
Abstract
OBJECTIVE
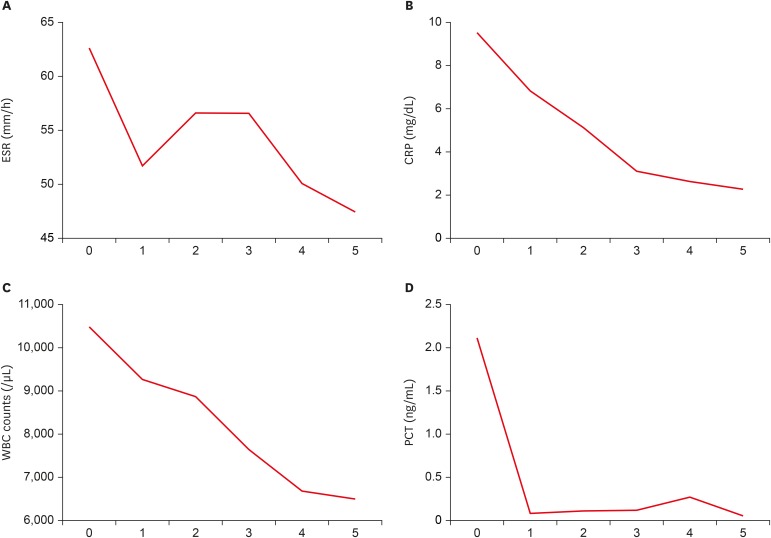
The laboratory biomarkers used to diagnose spinal infection include white blood cell (WBC) counts, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). Recently, procalcitonin (PCT) has been used as a biomarker to distinguish between bacterial infection and non-bacterial infection. We aimed to compare the changes of conventional biomarker and PCT in patients with spinal infection before and after antibiotic treatment.
METHODS
ESR, CRP, WBC counts, and PCT were measured in 29 patients diagnosed with pyogenic spinal infection at our hospital between May 2016 and December 2018 prior to antibiotic administration. After antibiotic administration, the values were followed up for 4 weeks at 1-week intervals.
RESULTS
A total of 29 patients were enrolled, with a mean age of 67.8 years, consisting of 16 men and 13 women. Twenty-five patients had lumbar infections, and 2 each had cervical and thoracic infections. The mean ESR, CRP, PCT, and WBCs decreased at week 4 of antibiotic treatment compared to their baseline values. CRP and WBCs were significantly decreased after 4 weeks of treatment compared to before treatment. The mean ESR and PCT was not statistically significant compared to pretreatment and after antibiotic treatment (p-value>0.05).
CONCLUSION
Among several biomarker, CRP and WBCs are biomarkers that can aid early evaluation of the effects of antibiotic treatment in pyogenic spondylitis. Although PCT did not have statistical significance, it can be used as a biomarker that reflects the effect of antibiotic and severity of infection.
Keyword
MeSH Terms
Figure
Reference
-
1. Becker KL, Snider R, Nylen ES. Procalcitonin in sepsis and systemic inflammation: a harmful biomarker and a therapeutic target. Br J Pharmacol. 2010; 159:253–264. PMID: 20002097.
Article2. Branche A, Neeser O, Mueller B, Schuetz P. Procalcitonin to guide antibiotic decision making. Curr Opin Infect Dis. 2019; 32:130–135. PMID: 30648993.
Article3. Bustamante A, Vilar-Bergua A, Guettier S, Sánchez-Poblet J, García-Berrocoso T, Giralt D, et al. C-reactive protein in the detection of post-stroke infections: systematic review and individual participant data analysis. J Neurochem. 2017; 141:305–314. PMID: 28171699.
Article4. Choi MK, Kim SB, Kim KD, Ament JD. Sequential changes of plasma C-reactive protein, erythrocyte sedimentation rate and white blood cell count in spine surgery: comparison between lumbar open discectomy and posterior lumbar interbody fusion. J Korean Neurosurg Soc. 2014; 56:218–223. PMID: 25368764.5. Chung YG, Won YS, Kwon YJ, Shin HC, Choi CS, Yeom JS. Comparison of serum CRP and procalcitonin in patients after spine surgery. J Korean Neurosurg Soc. 2011; 49:43–48. PMID: 21494362.
Article6. Dapunt U, Bürkle C, Günther F, Pepke W, Hemmer S, Akbar M. Surgical site infections following instrumented stabilization of the spine. Ther Clin Risk Manag. 2017; 13:1239–1245. PMID: 29033574.
Article7. De Santis V, Corona A. Procalcitonin to guide antibiotic stewardship in intensive care. Lancet Infect Dis. 2016; 16:887–888. PMID: 27477972.
Article8. Dubost JJ, Lopez J, Pereira B, Couderc M, Tournadre A, Soubrier M. Serum procalcitonin measurement is not a useful biomarker in the detection of primary infectious spondylodiscitis. Joint Bone Spine. 2017; 84:503–504. PMID: 27659402.
Article9. Gilbert DN. Use of plasma procalcitonin levels as an adjunct to clinical microbiology. J Clin Microbiol. 2010; 48:2325–2329. PMID: 20421436.
Article10. Heim N, Wiedemeyer V, Reich RH, Martini M. The role of C-reactive protein and white blood cell count in the prediction of length of stay in hospital and severity of odontogenic abscess. J Craniomaxillofac Surg. 2018; 46:2220–2226. PMID: 30416035.
Article11. Jenkins TC, Haukoos JS, Cotton E, Weitzenkamp D, Frank DN, Burman WJ. Time course of C-reactive protein and procalcitonin levels during the treatment of acute bacterial skin infections. Open Forum Infect Dis. 2018; 5:ofy029. PMID: 29516022.
Article12. Jeong DK, Lee HW, Kwon YM. Clinical value of procalcitonin in patients with spinal infection. J Korean Neurosurg Soc. 2015; 58:271–275. PMID: 26539272.
Article13. Jeong SJ, Choi SW, Youm JY, Kim HW, Ha HG, Yi JS. Microbiology and epidemiology of infectious spinal disease. J Korean Neurosurg Soc. 2014; 56:21–27. PMID: 25289121.
Article14. Kang KT, Son DW, Lee SH, Song GS, Sung SK, Lee SW. Variation of C-reactive protein and white blood cell counts in spinal operation: primary fusion surgery versus revision fusion surgery. Korean J Spine. 2017; 14:66–70. PMID: 29017299.
Article15. Kunakornsawat S, Tungsiripat R, Putthiwara D, Piyakulkaew C, Pluemvitayaporn T, Pruttikul P, et al. Postoperative kinetics of C-reactive protein and erythrocyte sediment rate in one-, two-, and multilevel posterior spinal decompressions and instrumentations. Global Spine J. 2017; 7:448–451. PMID: 28811989.
Article16. Lener S, Hartmann S, Barbagallo GM, Certo F, Thomé C, Tschugg A. Management of spinal infection: a review of the literature. Acta Neurochir (Wien). 2018; 160:487–496. PMID: 29356895.
Article17. Maus U, Andereya S, Gravius S, Ohnsorge JA, Miltner O, Niedhart C. Procalcitonin (PCT) as diagnostic tool for the monitoring of spondylodiscitis. Z Orthop Unfall. 2009; 147:59–64. PMID: 19263315.18. Mun JH, Kim DH, Ryu KS, Park CK, Kim MC. Diagnostic value of early inflammatory reaction in postoperative infection of the lumbar spine. J Korean Neurosurg Soc. 2005; 38:206–210.19. Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine. 2009; 34:1422–1428. PMID: 19478664.
Article20. Samsudin I, Vasikaran SD. Clinical Utility and Measurement of Procalcitonin. Clin Biochem Rev. 2017; 38:59–68. PMID: 29332972.21. Schuetz P, Beishuizen A, Broyles M, Ferrer R, Gavazzi G, Gluck EH, et al. Procalcitonin (PCT)-guided antibiotic stewardship: an international experts consensus on optimized clinical use. Clin Chem Lab Med. 2019; 57:1308–1318. PMID: 30721141.
Article22. Shehabi Y, Seppelt I. Pro/Con debate: is procalcitonin useful for guiding antibiotic decision making in critically ill patients? Crit Care. 2008; 12:211. PMID: 18466649.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antibiotic Use in Pediatric Dentistry
- Current Status of Antibiotic Stewardship and the Role of Biomarkers in Antibiotic Stewardship Programs
- Infectious diseases and biomarker use
- Role of biomarkers in antimicrobial stewardship: physicians’ perspectives
- Clinical Utility of Procalcitonin on Antibiotic Stewardship: A Narrative Review