Korean Circ J.
2019 Nov;49(11):1052-1061. 10.4070/kcj.2019.0098.
Temporal Variability of Platelet Reactivity in Patients Treated with Clopidogrel or Ticagrelor
- Affiliations
-
- 1Department of Cardiovascular Medicine, Regional Cardiocerebrovascular Center, Wonkwang University Hospital, Iksan, Korea. shururuka73@gmail.com
- KMID: 2460531
- DOI: http://doi.org/10.4070/kcj.2019.0098
Abstract
- BACKGROUND AND OBJECTIVES
The degree of antiplatelet response to P2Y12 inhibitors has been associated with clinical outcomes. The aim of this study was to test the variability of platelet reactivity over time among patients treated with clopidogrel or ticagrelor.
METHODS
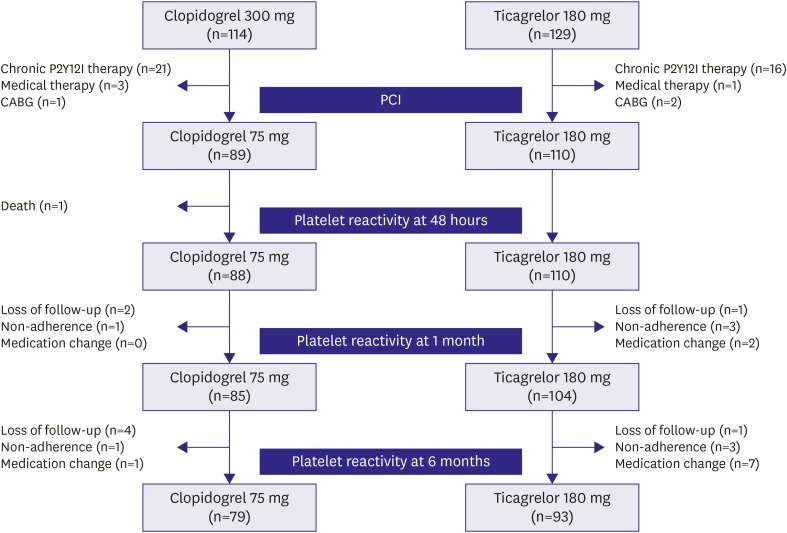
A single-center cohort of acute coronary syndrome patients that underwent percutaneous coronary intervention (PCI) was analyzed. Platelet reactivity was measured at baseline, 48 hours after PCI, 1 month, and 6 months after clopidogrel (n=79) or ticagrelor (n=93) treatment. High on-treatment platelet reactivity (HPR) was defined as ≥47 U, assessed by multiple electrode platelet aggregometry.
RESULTS
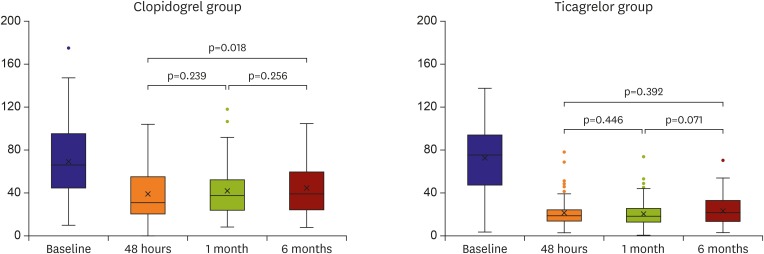
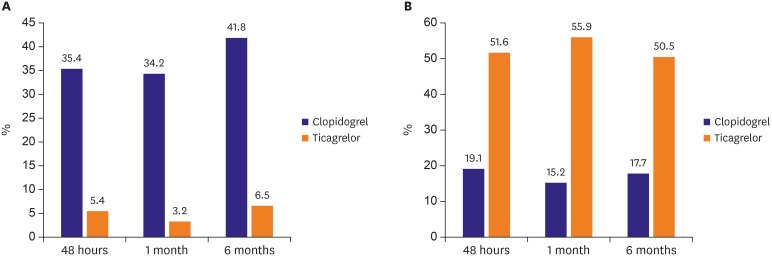
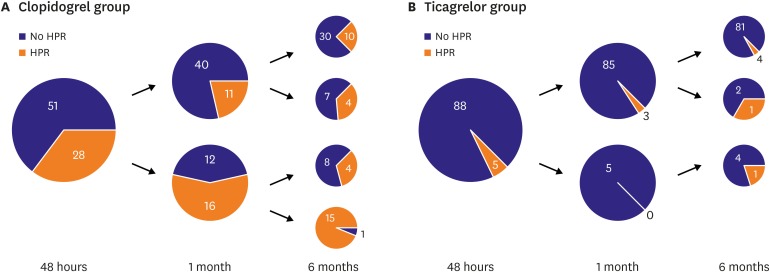
Platelet reactivity in the clopidogrel group increased over time, 38.2±21.7 U at 48 hours, 41.4±22.3 U at 1 month, and 44.7±25.5 U at 6 months (p=0.018, 48 hours to 6 months). However, platelet reactivity in the ticagrelor group was not significantly changed, 21.4±12.6 U at 48 hours, 20.0±12.2 U at 1 month, and 22.8±13.8 U at 6 months (p=0.392). A platelet reactivity change over time of more than 20U was found in 67.1% of the patients with clopidogrel group and 34.4% of ticagrelor group (p<0.001). Between 48 hours and 6 months, 43% of patients changed their responder status in the clopidogrel group, and 13% in the ticagrelor group (p<0.001).
CONCLUSIONS
Although ticagrelor treatment resulted in less temporal variability of platelet reactivity than clopidogrel treatment in terms of HPR, platelet reactivity varied over time in a significant proportion of patients.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Temporal Variability of Platelet Reactivity Phenotype: Another Barrier to Personalized Antiplatelet Strategy Guided by Platelet Function Testing
Young-Hoon Jeong, Udaya S. Tantry, Paul A. Gurbel
Korean Circ J. 2019;49(11):1062-1065. doi: 10.4070/kcj.2019.0260.
Reference
-
1. Park DW, Lee SW, Yun SC, et al. A point-of-care platelet function assay and C-reactive protein for prediction of major cardiovascular events after drug-eluting stent implantation. J Am Coll Cardiol. 2011; 58:2630–2639. PMID: 22152948.2. Stone GW, Witzenbichler B, Weisz G, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013; 382:614–623. PMID: 23890998.3. Trenk D, Hochholzer W, Fromm MF, et al. Cytochrome P450 2C19 681G>A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J Am Coll Cardiol. 2008; 51:1925–1934. PMID: 18482659.4. Sibbing D, Braun S, Morath T, et al. Platelet reactivity after clopidogrel treatment assessed with point-of-care analysis and early drug-eluting stent thrombosis. J Am Coll Cardiol. 2009; 53:849–856. PMID: 19264241.5. Breet NJ, van Werkum JW, Bouman HJ, et al. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. JAMA. 2010; 303:754–762. PMID: 20179285.6. Price MJ, Berger PB, Teirstein PS, et al. Standard- vs high-dose clopidogrel based on platelet function testing after percutaneous coronary intervention: the GRAVITAS randomized trial. JAMA. 2011; 305:1097–1105. PMID: 21406646.7. Trenk D, Stone GW, Gawaz M, et al. A randomized trial of prasugrel versus clopidogrel in patients with high platelet reactivity on clopidogrel after elective percutaneous coronary intervention with implantation of drug-eluting stents: results of the TRIGGER-PCI (Testing Platelet Reactivity In Patients Undergoing Elective Stent Placement on Clopidogrel to Guide Alternative Therapy With Prasugrel) study. J Am Coll Cardiol. 2012; 59:2159–2164. PMID: 22520250.8. Suh JW, Lee SP, Park KW, et al. Multicenter randomized trial evaluating the efficacy of cilostazol on ischemic vascular complications after drug-eluting stent implantation for coronary heart disease: results of the CILON-T (influence of CILostazol-based triple antiplatelet therapy ON ischemic complication after drug-eluting stenT implantation) trial. J Am Coll Cardiol. 2011; 57:280–289. PMID: 21232664.9. Hochholzer W, Ruff CT, Mesa RA, et al. Variability of individual platelet reactivity over time in patients treated with clopidogrel: insights from the ELEVATE-TIMI 56 trial. J Am Coll Cardiol. 2014; 64:361–368. PMID: 25060370.10. Gurbel PA, Bliden KP, Butler K, et al. Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET study. Circulation. 2009; 120:2577–2585. PMID: 19923168.11. Tantry US, Bonello L, Aradi D, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013; 62:2261–2273. PMID: 24076493.12. Nührenberg TG, Stratz C, Leggewie S, et al. Temporal variability in the antiplatelet effects of clopidogrel and aspirin after elective drug-eluting stent implantation. An ADAPT-DES substudy. Thromb Haemost. 2015; 114:1020–1027. PMID: 26305340.13. Campo G, Parrinello G, Ferraresi P, et al. Prospective evaluation of on-clopidogrel platelet reactivity over time in patients treated with percutaneous coronary intervention relationship with gene polymorphisms and clinical outcome. J Am Coll Cardiol. 2011; 57:2474–2483. PMID: 21679849.14. Dorsam RT, Kunapuli SP. Central role of the P2Y12 receptor in platelet activation. J Clin Invest. 2004; 113:340–345. PMID: 14755328.15. Patrono C, Coller B, FitzGerald GA, Hirsh J, Roth G. Platelet-active drugs: the relationships among dose, effectiveness, and side effects: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126:234S–264S. PMID: 15383474.16. Yun KH, Rhee SJ, Park HY, et al. Effects of omeprazole on the antiplatelet activity of clopidogrel. Int Heart J. 2010; 51:13–16. PMID: 20145345.17. Deharo P, Quilici J, Bonnet G, et al. Is platelet inhibition correlated with time from last intake on P2Y12 blockers after an acute coronary syndrome? A pilot study. Platelets. 2016; 27:791–795. PMID: 27275528.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Platelet Number and Platelet Indices on Platelet Reactivity in Patients Treated with Clopidogrel or Ticagrelor
- Ticagrelor Use in Indian Patients Undergoing Neuroendovascular Procedures: A Single Center Experience
- Hypersensitivity to ticagrelor and low response to clopidogrel: a case report
- The effect of antiplatelet drug on coronary endothelial and microvascular function: comparison with ticagrelor and clopidogrel
- An Intra-procedural Stent Thrombosis in a Prasugrel Resistant Patient Treated with Ticagrelor