J Korean Ophthalmol Soc.
2019 Oct;60(10):929-934. 10.3341/jkos.2019.60.10.929.
Repeatability and Reproducibility of Tear Meniscus Evaluations Using Two Different Spectral Domain-optical Coherence Tomography
- Affiliations
-
- 1Department of Ophthalmology, Ewha Womans University College of Medicine, Seoul, Korea. hkeoph@gmail.com
- KMID: 2460510
- DOI: http://doi.org/10.3341/jkos.2019.60.10.929
Abstract
- PURPOSE
To evaluate the repeatability and reproducibility of inferior tear meniscus measurements using two different spectral domain-optical coherence tomography (OCT), and to compare the inter-device agreements between these devices.
METHODS
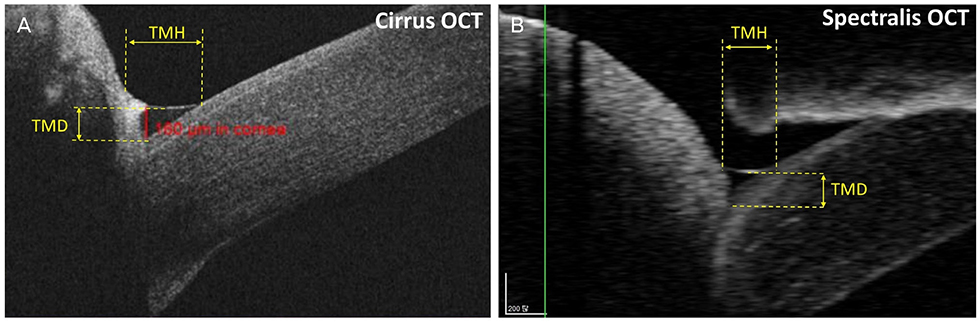
Two examiners evaluated the tear meniscus depth (TMD) and tear meniscus height (TMH) of 20 eyes in 20 normal subjects using Cirrus OCT and Spectralis OCT with the examiners calculating the TMD and TMH. We analyzed intra-examiner repeatability, inter-examiner reproducibility, and inter-device agreement.
RESULTS
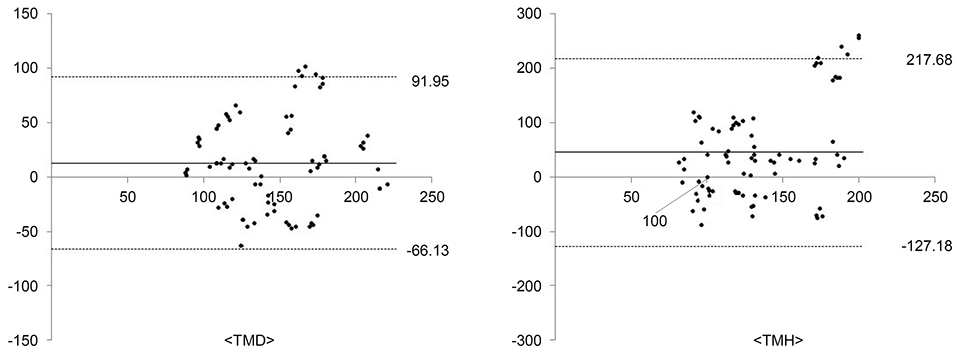
The average TMD measurements using the Cirrus OCT and Spectralis OCT devices were 151.25 ± 41.53 µm and 139.10 ± 40.56 µm by examiner 1, respectively, and 152.03 ± 42.77 µm and 138.35 ± 39.70 µm by examiner 2, respectively. The TMHs were 291.90 ± 100.19 µm and 245.43 ± 66.44 µm by examiner 1, respectively, and 288.25 ± 98.72 µm and 244.23 ± 60.69 µm by examiner 2, respectively. The TMDs and TMHs measured using these OCT devices were not statistically significant for intra-examiner and inter-examiner measurements (all, p > 0.05). These devices showed high repeatability (intraclass correlation coefficient ≥ 0.991) for intra-examiner TMD and TMH measurements and the inter-examiner coefficient of variation ranged from 2.04% to 4.32%. The 95% limits of agreement between the two devices were −66.13 to 91.95 µm for TMD and −127.18 to 217.68 µm for TMH.
CONCLUSIONS
Both OCT devices are useful for conducting inferior tear meniscus measurements. The inter-device agreement was poor, and the devices were not interchangeable.
Keyword
MeSH Terms
Figure
Reference
-
1. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.2. Lin PY, Tsai SY, Cheng CY, et al. Prevalence of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology. 2003; 110:1096–1101.3. McCarty CA, Bansal AK, Livingston PM, et al. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology. 1998; 105:1114–1119.4. Kallarackal GU, Ansari EA, Amos N, et al. A comparative study to assess the clinical use of fluorescein meniscus time (FMT) with tear break up time (TBUT) and Schirmer's tests (ST) in the diagnosis of dry eyes. Eye. 2002; 16:594–600.
Article5. Senchyna M, Wax MB. Quantitative assessment of tear production: a review of methods and utility in dry eye drug discovery. J Ocul Biol Dis Infor. 2008; 1:1–6.
Article6. Mishima S, Gasset A, Klyce SD Jr, Baum JL. Determination of tear volume and tear flow. Invest Ophthalmol. 1966; 5:264–276.7. Yokoi N, Bron AJ, Tiffany JM, et al. Relationship between tear volume and tear meniscus curvature. Arch Ophthalmol. 2004; 122:1265–1269.
Article8. Mainstone JC, Bruce AS, Golding TR. Tear meniscus measurement in the diagnosis of dry eye. Curr Eye Res. 1996; 15:653–661.
Article9. Lim KJ, Lee JH. Measurement of the tear meniscus height using 0.25% fluorescein sodium. Korean J Ophthalmol. 1991; 5:34–36.
Article10. Ibrahim OM, Dogru M, Ward SK, et al. The efficacy, sensitivity, and specificity of strip meniscometry in conjunction with tear function tests in the assessment of tear meniscus. Invest Ophthalmol Vis Sci. 2011; 52:2194–2198.
Article11. Raj A, Dhasmana R, Nagpal RC. Anterior segment optical coherence tomography for tear meniscus evaluation and its correlation with other tear variables in healthy individuals. J Clin Diagn Res. 2016; 10:NC01-4.
Article12. Chan HH, Zhao Y, Tun TA, Tong L. Repeatability of tear meniscus evaluation using spectral-domain Cirrus(R) HD-OCT and time-domain Visante(R) OCT. Cont Lens Anterior Eye. 2015; 38:368–372.13. Arriola-Villalobos P, Fernández-Vigo JI, Díaz-Valle D, et al. Assessment of lower tear meniscus measurements obtained with keratograph and agreement with fourier-domain optical-coherence tomography. Br J Ophthalmol. 2015; 99:1120–1125.
Article14. Vaz S, Falkmer T, Passmore AE, et al. The case for using the repeatability coefficient when calculating test-retest reliability. PLoS One. 2013; 8:e73990.
Article15. Kong KA. Statistical methods: reliability assessment and method comparison. Ewha Med J. 2017; 40:9–16.
Article16. Jones LW, Rahman S, Leech R, et al. Determination of inferior tear meniscus height and inferior tear meniscus volume using optical coherence tomography. Invest Ophthalmol Vis Sci. 2004; 45:144.
Article17. Bitton E, Keech A, Simpson T, Jones L. Variability of the analysis of the tear meniscus height by optical coherence tomography. Optom Vis Sci. 2007; 84:903–908.
Article18. Arriola-Villalobos P, Fernández-Vigo JI, Díaz-Valle D, et al. Lower tear meniscus measurements using a new anterior segment swept-source optical coherence tomography and agreement with fourier-domain optical coherence tomography. Cornea. 2016; 36:183–188.
Article19. Zhou S, Li Y, Lu AT, et al. Reproducibility of tear meniscus measurement by Fourier-domain optical coherence tomography: a pilot study. Ophthalmic Surg Lasers Imaging. 2009; 40:442–447.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repeatability of Spectral Domain OCT (3D-OCT 1000) in Normal Subjects and Various Macular Diseases
- Changes in Tear Volume after 3% Diquafosol Treatment in Patients with Dry Eye Syndrome: An Anterior Segment Spectral-domain Optical Coherence Tomography Study
- The Repeatability of Retinal Layer Thickness Measurements with Spectral-Domain Optical Coherence Tomography in Normal Eyes
- Tear Meniscus Evaluation Using Optical Coherence Tomography in Dry Eye Patients
- Changes in Area of Conjunctiva and Tear Meniscus Measured Using Anterior Segment Optical Coherence Tomography after Conjunctivochalasis Surgery