Yonsei Med J.
2019 Oct;60(10):890-897. 10.3349/ymj.2019.60.10.890.
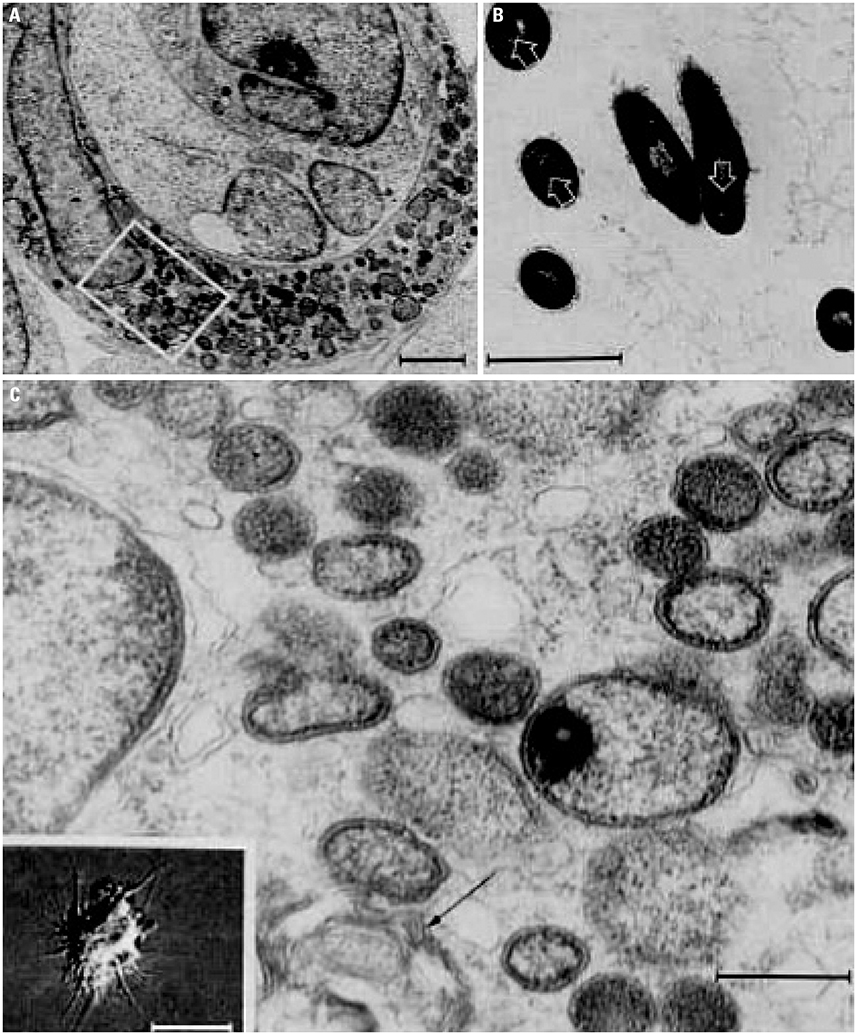
“Hairiness†is a Facsimile of Reorganized Cytoskeletons: A Cytopathic Effect of Coxiella burnetii
- Affiliations
-
- 1Emeritus Professor, Yonsei University College of Medicine, Seoul, Korea. wyleegkl@naver.com
- KMID: 2459141
- DOI: http://doi.org/10.3349/ymj.2019.60.10.890
Abstract
- In 1993, I reported that Coxiella burnetii transforms human B cells into hairy cells (cbHCs), the first hairy cell reported outside of hairy cell leukemia (HCL). Over last few decades, advances in molecular biology have provided evidence supporting that C. burnetii induces hairiness and inhibits the apoptosis of host cells. The present review summarizes new information in support of cbHC. C. burnetii was shown to induce reorganization of the cytoskeleton and to inhibit apoptosis in host cells. Peritoneal B1a cells were found to be permissive for virulent C. burnetii Nine Mile phase I (NMI) strains in mice. C. burnetii severely impaired E-cad expression in circulating cells of Q fever patients. B-cell non-Hodgkin lymphoma was linked to C. burnetii. Mutation of BRAF V600E was pronounced in HCL, but "hairiness" was not linked to the mutation. Risk factors shared among coxiellosis and HCL in humans and animals were reported in patients with Q-fever. Accordingly, I propose that C. burnetii induces reorganization of the cytoskeleton and inhibits apoptosis as cytopathic effects that are not target cell specific. The observed hairiness in cbHC appears to be a fixed image of dynamic nature, and hairy cells in HCL are distinct among lymphoid cells in circulation. As the cytoskeleton plays key roles in maintaining cell structural integrity in health and disease, the pathophysiology of similar cytopathic effects should be addressed in other diseases, such as myopathies, B-cell dyscrasias, and autoimmune syndromes.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee WY. Hairy cell transformation of human peripheral blood lymphocytes by Coxiella burnetii. Yonsei Med J. 1993; 34:11–21.
Article2. Lee WY, Lee JM, Park KH, Park C, Chang M, Hong WP, et al. Coxiella burnetii in polymorphic lymphocytes in tissue and blood of patients with polymorphic reticulosis. Acta Virol. 1995; 39:269–274.3. Angelakis E, Raoult D. Q fever. Vet Microbiol. 2010; 140:297–309.
Article4. Melenotte C, Million M, Audoly G, Gorse A, Dutronc H, Roland G, et al. B-cell non-Hodgkin lymphoma linked to Coxiella burnetii. Blood. 2016; 127:113–121.
Article5. Ammatuna E, Iannitto E, Tick LW, Arents NL, Kuijper PH, Nijziel MR. Two cases of q-Fever in hairy cell leukemia. Case Rep Hematol. 2014; 2014:863932.
Article6. Achten-Weiler M, Veldhuis Kroeze EJ, Boerma S, van der. Hairy cell-like leukemia in a 9-year-old Friesian mare. Vet Q. 2016; 36:105–108.
Article7. Al-Bagdadi FK, Seger CL, Henry RW, Neal Maulden G. Acute lymphoblast leukemia in sheep induced by inoculation of bovine leukemia virus: diagnostic electron microscopic morphological study. Ultrastruct Pathol. 2006; 30:85–94.
Article8. Schrek R, Donnelly WJ. “Hairy” cells in blood in lymphoreticular neoplastic disease and “flagellated” cells of normal lymph nodes. Blood. 1966; 27:199–211.
Article9. Shao H, Calvo KR, Grönborg M, Tembhare PR, Kreitman RJ, Stetler-Stevenson M, et al. Distinguishing hairy cell leukemia variant from hairy cell leukemia: development and validation of diagnostic criteria. Leuk Res. 2013; 37:401–409.
Article10. Braylan RC, Jaffee ES, Triche TJ, Nanba K, Fowlkes Bi, Metzger H, et al. Structural and functional properties of the “hairy” cells of leukemic reticuloendotheliosis. Cancer. 1978; 41:210–227.
Article11. Golomb HM, Mintz U, Vardiman J, Wilson C, Rosner MC. Surface immunoglobulins, lectin-induced cap formation, and phagocytic function in five patients with the leukemic phase of hairy cell leukemia. Cancer. 1980; 46:50–55.
Article12. Caligaris-Cappio F, Janossy G, Campana D, Chilosi M, Bergui L, Foà R, et al. Lineage relationship of chronic lymphocytic leukemia and hairy cell leukemia: studies with TPA. Leuk Res. 1984; 8:567–578.
Article13. Braun J, Unanue ER. The lymphocyte cytoskeleton and its control of surface receptor functions. Semin Hematol. 1983; 20:322–333.14. Cohen HJ. Human lymphocyte surface immunoglobulin capping. Normal characteristics and anomalous behavior of chronic lymphocytic leukemic lymphocytes. J Clin Invest. 1975; 55:84–93.
Article15. Caligaris-Cappio F, Bergui L, Tesio L, Corbascio G, Tousco F, Marchisio PC. Cytoskeleton organization is aberrantly rearranged in the cells of B chronic lymphocytic leukemia and hairy cell leukemia. Blood. 1986; 67:233–239.
Article16. Schrek R, Messmore HL, Knospe WH, Stefani SS. A colchicine-sensitivity test for leukaemic lymphocytes. Scand J Haematol. 1976; 16:357–364.
Article17. Tiacci E, Trifonov V, Schiavoni G, Holmes A, Kern W, Martelli MP, et al. BRAF mutations in hairy-cell leukemia. N Engl J Med. 2011; 364:2305–2315.18. Boyd EM, Bench AJ, van't Veer MB, Wright P, Bloxham DM, Follows GA, et al. High resolution melting analysis for detection of BRAF exon 15 mutations in hairy cell leukaemia and other lymphoid malignancies. Br J Haematol. 2011; 155:609–612.
Article19. Arcaini L, Zibellini S, Boveri E, Riboni R, Rattotti S, Varettoni M, et al. The BRAF V600E mutation in hairy cell leukemia and other mature B-cell neoplasms. Blood. 2012; 119:188–191.
Article20. Schnittger S, Bacher U, Haferlach T, Wendland N, Ulke M, Dicker F, et al. Development and validation of a real-time quantification assay to detect and monitor BRAFV600E mutations in hairy cell leukemia. Blood. 2012; 119:3151–3154.
Article21. Thompson PA, Ravandi F. How I manage patients with hairy cell leukaemia. Br J Haematol. 2017; 177:543–556.
Article22. Xi L, Arons E, Navarro W, Calvo KR, Stetler-Stevenson M, Raffeld M, et al. Both variant and IGHV4-34-expressing hairy cell leukemia lack the BRAF V600E mutation. Blood. 2012; 119:3330–3332.
Article23. Weston-Bell NJ, Hendriks D, Sugiyarto G, Bos NA, Kluin-Nelemans HC, Forconi F, et al. Hairy cell leukemia cell lines expressing annexin A1 and displaying B-cell receptor signals characteristic of primary tumor cells lack the signature BRAF mutation to reveal unrepresentative origins. Leukemia. 2013; 27:241–245.
Article24. Tiacci E, Pucciarini A, Bigerna B, Pettirossi V, Strozzini F, Martelli MP, et al. Absence of BRAF-V600E in the human cell lines BONNA-12, ESKOL, HAIR-M, and HC-1 questions their origin from hairy cell leukemia. Blood. 2012; 119:5332–5333.
Article25. Chung SS, Kim E, Park JH, Chung YR, Lito P, Teruya-Feldstein J, et al. Hematopoietic stem cell origin of BRAFV600E mutations in hairy cell leukemia. Sci Transl Med. 2014; 6:238ra71.
Article26. Bang FB. History of tissue culture at Johns Hopkins. Bull Hist Med. 1977; 51:516–537.27. Lee WY. Effect of different substrates on chromosomes in rat cell line [dissertation]. Baltimore (MD): Johns Hopkins University;1977.28. Curtin JA, Fridlyand J, Kageshita T, Patel HN, Busam KJ, Kutzner H, et al. Distinct sets of genetic alterations in melanoma. N Engl J Med. 2005; 353:2135–2147.
Article29. Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999; 12:518–553.
Article30. Tissot-Dupont H, Raoult D. Q fever. Infect Dis Clin North Am. 2008; 22:505–514.
Article31. Parker NR, Barralet JH, Bell AM. Q fever. Lancet. 2006; 367:679–688.
Article32. Robyn MP, Newman AP, Amato M, Walawander M, Kothe C, Nerone JD, et al. Q fever outbreak among travelers to Germany who received live cell therapy--United States and Canada, 2014. MMWR Morb Mortal Wkly Rep. 2015; 64:1071–1073.
Article33. Dupont HT, Brouqui P, Faugere B, Raoult D. Prevalence of antibodies to Coxiella burnetii, Rickettsia conorii, and Rickettsia typhi in seven African countries. Clin Infect Dis. 1995; 21:1126–1133.
Article34. Mancini F, Di Luca M, Toma L, Vescio F, Bianchi R, Khoury C, et al. Prevalence of tick-borne pathogens in an urban park in Rome, Italy. Ann Agric Environ Med. 2014; 21:723–727.
Article35. Tissot-Dupont H, Amadei MA, Nezri M, Raoult D. Wind in November, Q fever in December. Emerg Infect Dis. 2004; 10:1264–1269.
Article36. Racult D, Stein A. Q fever during pregnancy--a risk for women, fetuses, and obstetricians. N Engl J Med. 1994; 330:371.37. Amit S, Shinar S, Halutz O, Atiya-Nasagi Y, Giladi M. Suspected person-to-person transmission of Q fever among hospitalized pregnant women. Clin Infect Dis. 2014; 58:e146–e147.
Article38. Kersh GJ, Priestley R, Massung RF. Stability of Coxiella burnetii in stored human blood. Transfusion. 2013; 53:1493–1496.39. Rottner K, Stradal TE, Wehland J. Bacteria-host-cell interactions at the plasma membrane: stories on actin cytoskeleton subversion. Dev Cell. 2005; 9:3–17.
Article40. Popoff MR. Bacterial factors exploit eukaryotic Rho GTPase signaling cascades to promote invasion and proliferation within their host. Small GTPases. 2014; 5:e28209.
Article41. Dellacasagrande J, Ghigo E, Hammami SME, Toman R, Raoult D, Capo C, et al. alpha(v)beta(3) integrin and bacterial lipopolysaccharide are involved in Coxiella burnetii-stimulated production of tumor necrosis factor by human monocytes. Infect Immun. 2000; 68:5673–5678.
Article42. Meconi S, Jacomo V, Boquet P, Raoult D, Mege JL, Capo C. Coxiella burnetii induces reorganization of the actin cytoskeleton in human monocytes. Infect Immun. 1998; 66:5527–5533.
Article43. Ghigo E, Capo C, Tung CH, Raoult D, Gorvel JP, Mege JL. Coxiella burnetii survival in THP-1 monocytes involves the impairment of phagosome maturation: IFN-gamma mediates its restoration and bacterial killing. J Immunol. 2002; 169:4488–4495.
Article44. Ramaekers FC, Bosman FT. The cytoskeleton and disease. J Pathol. 2004; 204:351–354.
Article45. Meconi S, Capo C, Remacle-Bonnet M, Pommier G, Raoult D, Mege JL. Activation of protein tyrosine kinases by Coxiella burnetii: role in actin cytoskeleton reorganization and bacterial phagocytosis. Infect Immun. 2001; 69:2520–2526.
Article46. Conti F, Boucherit N, Baldassarre V, Trouplin V, Toman R, Mottola G, et al. Coxiella burnetii lipopolysaccharide blocks p38α-MAPK activation through the disruption of TLR-2 and TLR-4 association. Front Cell Infect Microbiol. 2015; 4:182.
Article47. Honstettre A, Ghigo E, Moynault A, Capo C, Toman R, Akira S, et al. Lipopolysaccharide from Coxiella burnetii is involved in bacterial phagocytosis, filamentous actin reorganization, and inflammatory responses through toll-like receptor 4. J Immunol. 2004; 172:3695–3703.
Article48. Baca OG, Klassen DA, Aragon AS. Entry of Coxiella burnetii into host cells. Acta Virol. 1993; 37:143–155.49. Seshadri R, Paulsen IT, Eisen JA, Read TD, Nelson KE, Nelson WC, et al. Complete genome sequence of the Q-fever pathogen Coxiella burnetii. Proc Natl Acad Sci U S A. 2003; 100:5455–5460.
Article50. Beare PA, Gilk SD, Larson CL, Hill J, Stead CM, Omsland A, et al. Dot/Icm type IVB secretion system requirements for Coxiella burnetii growth in human macrophages. MBio. 2011; 2:e00175–e00111.
Article51. Carey KL, Newton HJ, Lührmann A, Roy CR. The Coxiella burnetii Dot/Icm system delivers a unique repertoire of type IV effectors into host cells and is required for intracellular replication. PLoS Pathog. 2011; 7:e1002056.
Article52. McDonough JA, Newton HJ, Roy CR. Coxiella burnetii secretion systems. In : Toman R, Heinzen RA, Samuel JE, Mege JL, editors. Coxiella burnetii: recent advances and new perspectives in research of the Q fever bacterium. Dordrecht: Springer;2012. p. 171–197.53. Mezouar S, Omar Osman I, Melenotte C, Slimani C, Chartier C, Raoult D, et al. High concentrations of serum soluble E-cadherin in patients with Q fever. Front Cell Infect Microbiol. 2019; 9:219.
Article54. Schoenlaub L, Elliott A, Freches D, Mitchell WJ, Zhang G. Role of B cells in host defense against primary Coxiella burnetii infection. Infect Immun. 2015; 83:4826–4836.
Article55. Lamkanfi M, Dixit VM. Manipulation of host cell death pathways during microbial infections. Cell Host Microbe. 2010; 8:44–54.
Article56. Hotchkiss RS, Strasser A, McDunn JE, Swanson PE. Cell death. N Engl J Med. 2009; 361:1570–1583.
Article57. Gallucci S, Lolkema M, Matzinger P. Natural adjuvants: endogenous activators of dendritic cells. Nat Med. 1999; 5:1249–1255.
Article58. Elliott MR, Ravichandran KS. Clearance of apoptotic cells: implications in health and disease. J Cell Biol. 2010; 189:1059–1070.
Article59. Faherty CS, Maurelli AT. Staying alive: bacterial inhibition of apoptosis during infection. Trends Microbiol. 2008; 16:173–180.
Article60. Omsland A, Cockrell DC, Howe D, Fischer ER, Virtaneva K, Sturdevant DE, et al. Host cell-free growth of the Q fever bacterium Coxiella burnetii. Proc Natl Acad Sci U S A. 2009; 106:4430–4434.
Article61. Lührmann A, Roy CR. Coxiella burnetii inhibits activation of host cell apoptosis through a mechanism that involves preventing cytochrome c release from mitochondria. Infect Immun. 2007; 75:5282–5289.
Article62. Voth DE, Heinzen RA. Lounging in a lysosome: the intracellular lifestyle of Coxiella burnetii. Cell Microbiol. 2007; 9:829–840.
Article63. Voth DE, Heinzen RA. Sustained activation of Akt and Erk1/2 is required for Coxiella burnetii antiapoptotic activity. Infect Immun. 2009; 77:205–213.
Article64. Pan X, Lührmann A, Satoh A, Laskowski-Arce MA, Roy CR. Ankyrin repeat proteins comprise a diverse family of bacterial type IV effectors. Science. 2008; 320:1651–1654.
Article65. Lührmann A, Nogueira CV, Carey KL, Roy CR. Inhibition of pathogen-induced apoptosis by a Coxiella burnetii type IV effector protein. Proc Natl Acad Sci U S A. 2010; 107:18997–19001.
Article66. Eckart RA, Bisle S, Schulze-Luehrmann J, Wittmann I, Jantsch J, Schmid B, et al. Antiapoptotic activity of Coxiella burnetii effector protein AnkG is controlled by p32-dependent trafficking. Infect Immun. 2014; 82:2763–2771.
Article67. Klingenbeck L, Eckart RA, Berens C, Lührmann A. The Coxiella burnetii type IV secretion system substrate CaeB inhibits intrinsic apoptosis at the mitochondrial level. Cell Microbiol. 2013; 15:675–687.
Article68. Melenotte C, Mezouar S, Ben Amara A, Benatti S, Chiaroni J, Devaux C, et al. A transcriptional signature associated with non-Hodgkin lymphoma in the blood of patients with Q fever. PLoS One. 2019; 14:e0217542.
Article69. Monnereau A, Slager SL, Hughes AM, Smith A, Glimelius B, Habermann TM, et al. Medical history, lifestyle, and occupational risk factors for hairy cell leukemia: the InterLymph Non-Hodgkin Lymphoma Subtypes Project. J Natl Cancer Inst Monogr. 2014; 2014:115–124.
Article70. Tadmor T, Polliack A. Epidemiology and environmental risk in hairy cell leukemia. Best Pract Res Clin Haematol. 2015; 28:175–179.
Article71. Morton LM, Slager SL, Cerhan JR, Wang SS, Vajdic CM, Skibola CF, et al. Etiologic heterogeneity among non-Hodgkin lymphoma subtypes: the InterLymph Non-Hodgkin Lymphoma Subtypes Project. J Natl Cancer Inst Monogr. 2014; 2014:130–144.72. Meadows S, Jones-Bitton A, McEwen SA, Jansen J, Patel SN, Filejski C, et al. Coxiella burnetii (Q Fever) seropositivity and associated risk factors in sheep and goat farm workers in Ontario, Canada. Vector Borne Zoonotic Dis. 2016; 16:643–649.
Article73. Somasundaram V, Ahuja A, Manivannan P, Chandra D, Purohit A, Saxena R. Unusual hairy projections in a case of T-acute lymphoblastic leukemia, a cause for diagnostic dilemma: a case report. J Hematol Thrombo Dis. 2015; 3:223.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Association of Kawasaki Disease and Coxiella burnetii
- Prevalence of antibodies to the coxiella burnetii phase II antigen among residents in korea
- Prevalence of antibodies to coxiella burnetii phase I antigen among Korean
- Prevalence of antibodies to the phase I antigen of coxiella burnetii , the Q fever agent, among residents in Korea
- Isolation and cultivation of a coxiella burnetii strain from raw milk of dairy cows in korea