J Korean Acad Psychiatr Ment Health Nurs.
2019 Sep;28(3):271-285. 10.12934/jkpmhn.2019.28.3.271.
Effectiveness of Acceptance and Commitment Therapy for Chronic Pain Patients: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Assistant professor, Department of Nursing, Sunlin University, Pohang, Korea.
- 2Professor, College of Social Sciences, Kyungpook National University, Daegu, Korea.
- 3Associate Professor, College of Nursing, Keimyung University, Daegu, Korea. sejun2@gw.kmu.ac.kr
- KMID: 2459090
- DOI: http://doi.org/10.12934/jkpmhn.2019.28.3.271
Abstract
- PURPOSE
The aims of this study was to evaluate the effects of acceptance and commitment therapy (ACT) for chronic pain patients.
METHODS
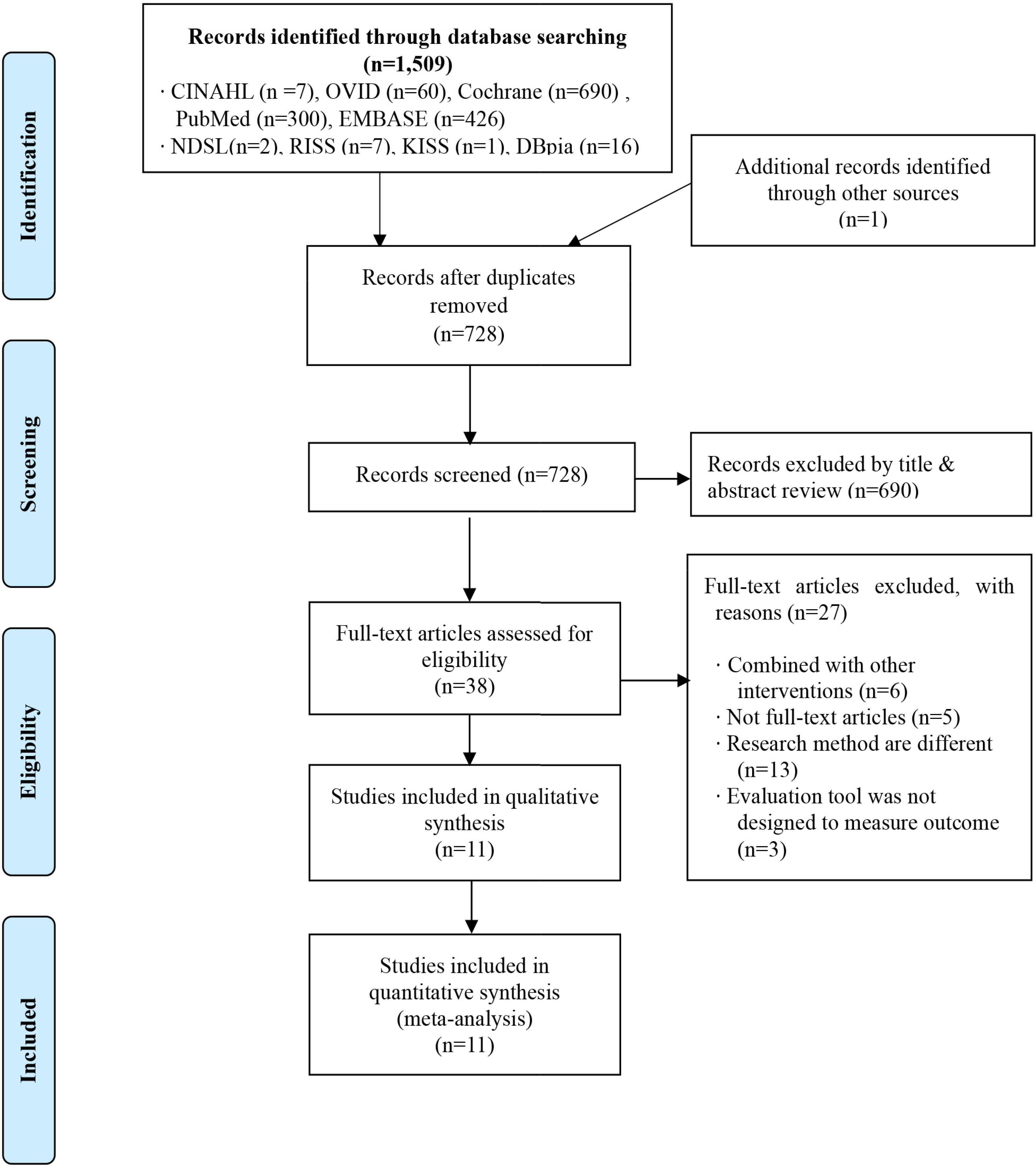
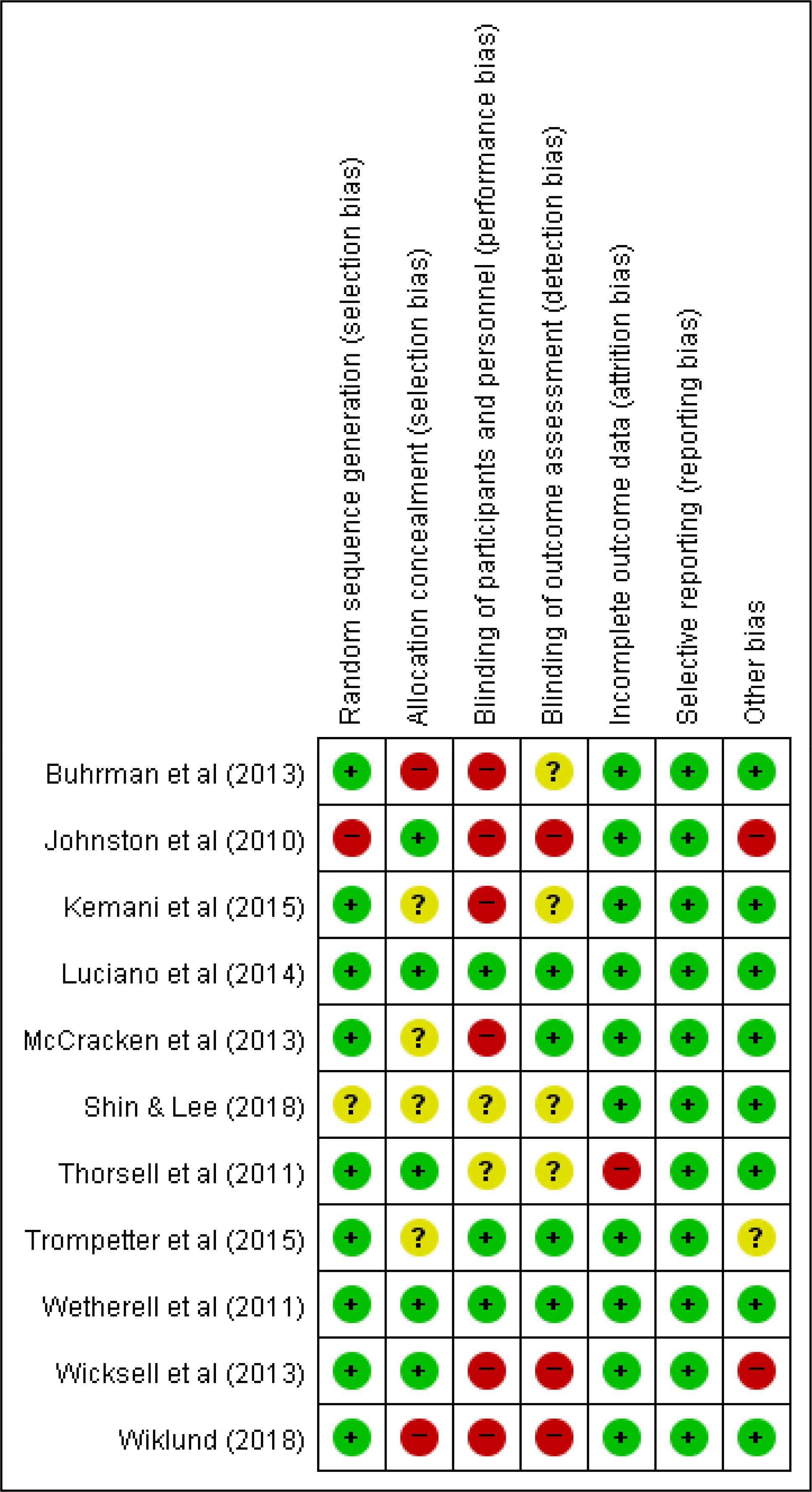
Based on the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses, we searched the Cochrane Library, CINAHL, EMBASE, OVID, PubMed and Korean databases to identify randomized controlled trials published through May 2019. To estimate the effect size, a meta-analysis of the studies was performed using the R program, and the risk of bias was assessed using the Cochrane's Risk of Bias tool for randomized studies.
RESULTS
A total of 11 studies were included in this study. Studies were heterogeneous, and random effects models were used in the analyses. ACT was effective for improving pain (g=−0.40, 95%CI:−0.69~−1.12, p<.001, I2=80%), pain acceptance (g=1.24, 95% CI:0.41~2.05, p<.001, I²=95%), anxiety (g=−0.47, 95% CI:−0.81~−0.13, p<.001, I²=84%), depression (g=−0.52, 95% CI:−0.85~−0.19, p<.001, I²=85%), and quality of life (g=1.14, 95% CI:0.11~2.17, p<.001, I²=95%).
CONCLUSION
Our study findings of the ACT seems to be effective for improving pain, pain acceptance, anxiety, depression, and quality of life in patients with chronic pain. Additionally, ACT may be useful for reducing barriers to therapy, and various studies should be attempted.
Keyword
MeSH Terms
Figure
Reference
-
1. Merskey HE. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. 2nd ed.Seattle: IASP Press;1994. p. 222.2. Jeong CKH, Park JY, Kim NS, Park HY. Status of chronic pain prevalence in the Korean adults [Internet]. 2015. [cited 2015 Aug 10]. Available from:. https://www.bioin.or.kr/board.do?num=254082&cmd=view&bid=policy.3. Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. The Journal of Pain: Official Journal of the American Pain Society. 2006; 7(11):779–793. https://doi.org/10.1016/j.jpain.2006.08.005.
Article4. Institute of Medicine Committee on Advancing Pain Research, Care, and Education. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington (DC): National Academies Press;2011. p. 364.5. Jeong EK, Kwak YH, Song JS. Influences of chronic pain on the use of medical services in South Korea. The Journal of the Korea Contents Assosciation. 2015; 15(2):363–369. https://doi.org/10.5392/JKCA.2015.15.02.363.
Article6. Breivik H, Eisenberg E, O' Brien T. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013; 13:1229. https://doi.org/10.1186/1471-2458-13-1229.
Article7. Zale EL, Ditre JW. Pain-related fear, disability, and the fear-avoidance model of chronic pain. Current Opinion Psychology. 2015; 5:24–30. https://doi.org/10.1016/j.copsyc.2015.03.014.
Article8. Azevedo LF, Costa-Pereira A, Mendonca L, Dias CC, Castro-Lopes JM. Epidemiology of chronic pain: a population-based nationwide study on its prevalence, characteristics and associated disability in Portugal. The Journal of Pain: Official Journal of the American Pain Society. 2012; 13(8):773–783. https://doi.org/10.1016/j.jpain.2012.05.012.9. Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. The Cochrane Database of Systematic Reviews. 2012; 11:1–112. https://doi.org/10.1002/14651858.CD007407.pub3.10. American Psychological Association. Pain. Psychology Topic [Internet]. 2000. [cited 2019 Jun 1]. Available from:. https://www.apa.org/topics/pain.11. McCracken LM, Turk DC. Behavioral and cognitive-behavioral treatment for chronic pain: outcome, predictors of outcome, and treatment process. Spine. 2002; 27(22):2564–2573. https://doi.org/10.1097/00007632-200211150-00033.12. Graham CD, Gouick J, Krahe C, Gillanders D. A systematic review of the use of acceptance and commitment therapy (ACT) in chronic disease and longterm conditions. Clinical Psychology Review. 2016; 46:46–58. https://doi.org/10.1016/j.cpr.2016.04.009.
Article13. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy. 2006; 44(1):1–25. https://doi.org/10.1016/j.brat.2005.06.006.
Article14. Kim KH, Kwon JH. Testing models of relation to academic & career stress, acceptance behavior, and the psychological wellbeing of college students. The Korean Association of Human Development. 2014; 21(4):43–46. https://doi.org/10.15284/kjhd.2014.21.4.43.15. Hayes SC, Strosahl KD, Wilson KG, Bissett RT, Pistorello J, Toarmino D, et al. Measuring experiential avoidance: a preliminary test of a working model. The Psychological Record. 2004; 54(4):553–578. https://doi.org/10.1007/BF03395492.
Article16. Hughes LS, Clark J, Colclough JA, Dale E, McMillan D. Acceptance and commitment therapy (ACT) for chronic pain: a systematic review and metaanalyses. The Clinical Journal of Pain. 2017; 33(6):552–568. https://doi.org/10.1097/AJP.0000000000000425.17. Ost LG. The efficacy of acceptance and commitment therapy: an updated systematic review and metaanalysis. Behaviour Research & Therapy. 2014; 61:105–121. https://doi.org/10.1016/j.brat.2014.07.018.18. Ong CW, Lee EB, Twohig MP. A metaanalysis of dropout rates in acceptance and commitment therapy. Behaviour Research and Therapy. 2018; 104:14–33. https://doi.org/10.1016/j.brat.2018.02.004.
Article19. Hacker T, Stone P, MacBeth A. Acceptance and commitment therapy - do we know enough? Cumulative and sequential metaanalyses of randomized controlled trials. Journal of Affective Disorders. 2016; 190:551–565. https://doi.org/10.1016/j.jad.2015.10.053.
Article20. Schutze R, Rees C, Smith A, Slater H, Campbell JM, O'Sullivan P. How can we best reduce pain catastrophizing in adults with chronic noncancer pain? A systematic review and metaanalysis. The Journal of Pain: Official Journal of the American Pain Society. 2018; 19(3):233–256. https://doi.org/10.1016/j.jpain.2017.09.010.21. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. BMJ: British Medical Journal. 2009; 339:b2535. https://doi.org/10.1136/bmj.b2535.
Article22. Higgins JPT, Green S. editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [Internet]. London, UK: The Cochrane Collaboration;2011. [cited 2016 Nov 29]. Available from:. http://handbook.cochrane.org.23. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to metaanalysis. West Sussex, UK: John Wiley & Sons, Ltd.;2009. p. 452.24. Thorsell J, Finnes S, Dahl JA, Lundgren T, Gybrant M, Gordh T, et al. A comparative study of 2 manual-based self-help interventions, acceptance and commitment therapy and applied relaxation, for persons with chronic pain. Clinical Journal of Pain. 2011; 27(8):716–723. https://doi.org/10.1097/AJP.0b013e318219a933.
Article25. Hayes SC, Strosahi KD. A practical guide to acceptance and commitment therapy. New York: Springer;2004. p. 396.26. Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KM. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cognitive Behavior Therapy. 2016; 45(1):5–31. https://doi.org/10.1080/16506073.2015.1098724.
Article27. Bach P, Hayes SC. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2002; 70(5):1129–1139. https://doi.org/10.1037/0022-006X.70.5.1129.
Article28. Twohig MP, Levin ME. Acceptance and commitment therapy as a treatment for anxiety and depression: a review. The Psychiatric Clinics of North America. 2017; 40(4):751–770. https://doi.org/10.1016/j.psc.2017.08.009.29. A-Tjak JGL, Davis ML, Morina N, Powers MB, Smits JA, Em-melkamp PM. A metaanalysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychotherapy and Psychosomatics. 2015; 84(1):30–36. https://doi.org/10.1159/000365764.
Article30. Park JH, Hyoung S. Effects of psychoeducational intervention for cancer survivors: a systematic review and metaanalysis. Journal of Korean Academy of Nursing. 2017; 47(2):143–163. https://doi.org/10.4040/jkan.2017.47.2.143.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improving Diabetes Self-Mangement and Mental Health through Acceptance and Commitment Therapy
- An Introduction of the Systematic Review and Meta-Analysis
- Acceptance and Commitment Therapy for Psychosis
- Introduction to systematic review and meta-analysis
- Effect of intracanal cryotherapy on postendodontic pain: a systematic review and meta-analysis of randomized controlled trials