J Gastric Cancer.
2019 Mar;19(1):49-61. 10.5230/jgc.2019.19.e2.
Intraoperative Neurophysiologic Testing of the Perigastric Vagus Nerve Branches to Evaluate Viability and Signals along Nerve Pathways during Gastrectomy
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul, Korea. seongho.kong@snu.ac.kr
- 2Department of Neurology, Seoul National University Hospital, Seoul, Korea. sueh916@gmail.com
- 3Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea.
- 4Cancer Research Institute, Seoul National University, Seoul, Korea.
- KMID: 2458817
- DOI: http://doi.org/10.5230/jgc.2019.19.e2
Abstract
- PURPOSE
The perigastric vagus nerve may play an important role in preserving function after gastrectomy, and intraoperative neurophysiologic tests might represent a feasible method of evaluating the vagus nerve. The purpose of this study is to assess the feasibility of neurophysiologic evaluations of the function and viability of perigastric vagus nerve branches during gastrectomy.
MATERIALS AND METHODS
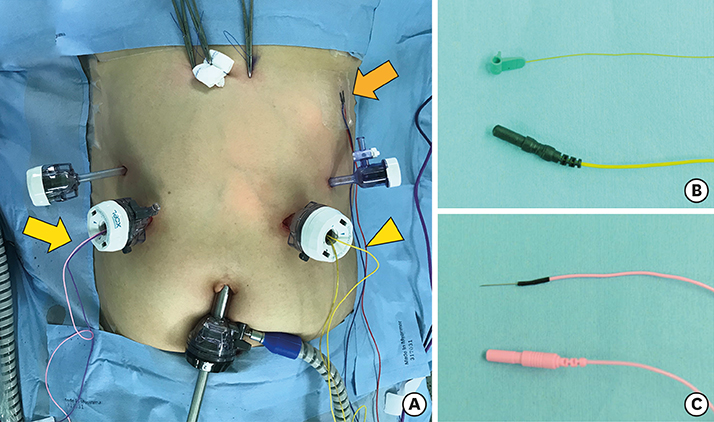
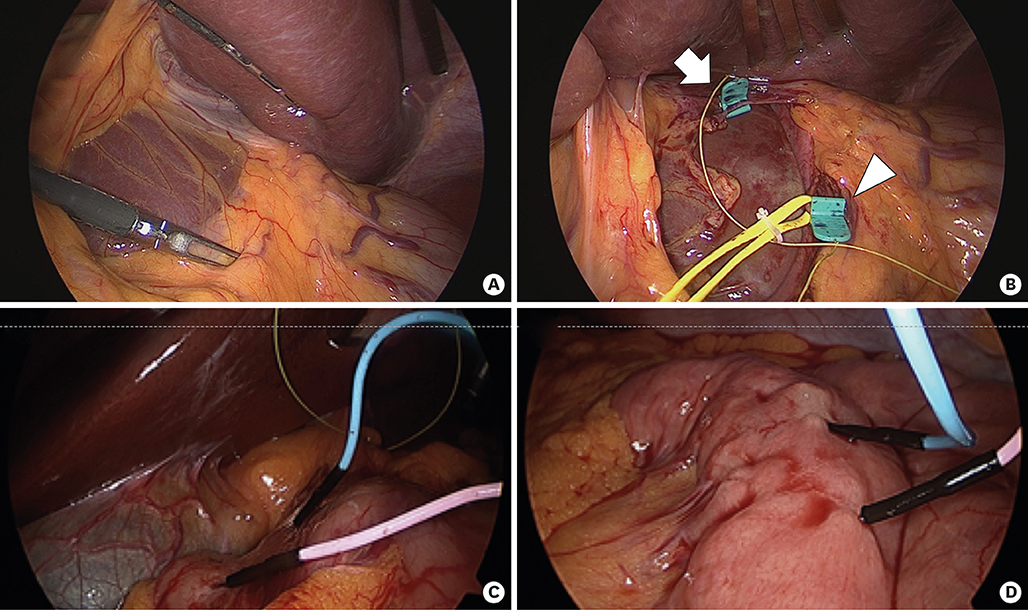
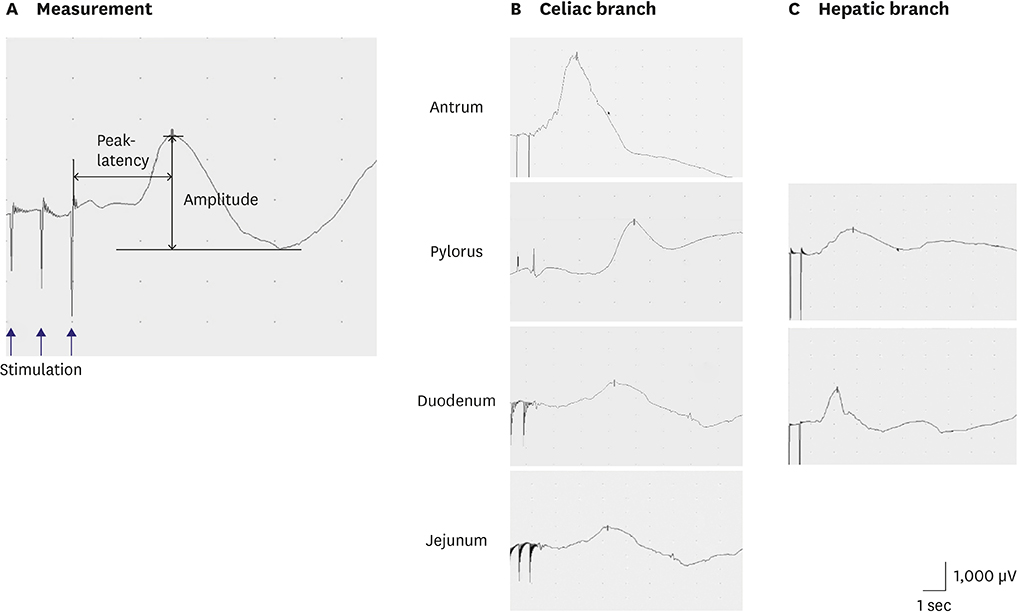
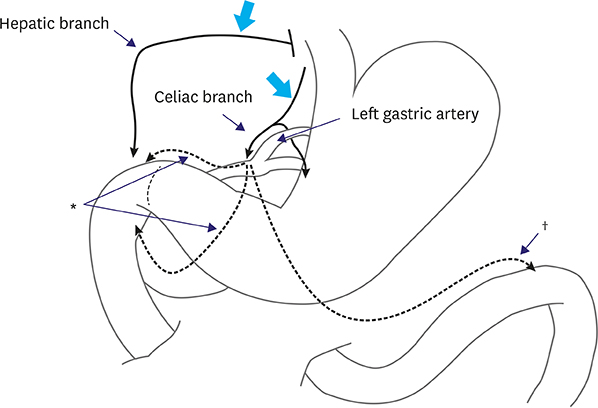
Thirteen patients (1 open total gastrectomy, 1 laparoscopic total gastrectomy, and 11 laparoscopic distal gastrectomy) were prospectively enrolled. The hepatic and celiac branches of the vagus nerve were exposed, and grabbing type stimulation electrodes were applied as follows: 10-30 mA intensity, 4 trains, 1,000 µs/train, and 5× frequency. Visible myocontractile movement and electrical signals were monitored via needle probes before and after gastrectomy. Gastrointestinal symptoms were evaluated preoperatively and postoperatively at 3 weeks and 3 months, respectively.
RESULTS
Responses were observed after stimulating the celiac branch in 10, 9, 10, and 6 patients in the antrum, pylorus, duodenum, and proximal jejunum, respectively. Ten patients responded to hepatic branch stimulation at the duodenum. After vagus-preserving distal gastrectomy, 2 patients lost responses to the celiac branch at the duodenum and jejunum (1 each), and 1 patient lost response to the hepatic branch at the duodenum. Significant procedure-related complications and meaningful postoperative diarrhea were not observed.
CONCLUSIONS
Intraoperative neurophysiologic testing seems to be a feasible methodology for monitoring the perigastric vagus nerves. Innervation of the duodenum via the celiac branch and postoperative preservation of the function of the vagus nerves were confirmed in most patients. TRIAL REGISTRATION: Clinical Research Information Service Identifier: KCT0000823
MeSH Terms
Figure
Reference
-
1. Bolton JS, Conway WC 2nd. Postgastrectomy syndromes. Surg Clin North Am. 2011; 91:1105–1122.
Article2. Nunobe S, Hiki N, Fukunaga T, Tokunaga M, Ohyama S, Seto Y, et al. Laparoscopy-assisted pylorus-preserving gastrectomy: preservation of vagus nerve and infrapyloric blood flow induces less stasis. World J Surg. 2007; 31:2335–2340.
Article3. Suh YS, Han DS, Kong SH, Kwon S, Shin CI, Kim WH, et al. Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg. 2014; 259:485–493.
Article4. Kim YG, Kong SH, Oh SY, Lee KG, Suh YS, Yang JY, et al. Effects of screening on gastric cancer management: comparative analysis of the results in 2006 and in 2011. J Gastric Cancer. 2014; 14:129–134.
Article5. Berthoud HR, Carlson NR, Powley TL. Topography of efferent vagal innervation of the rat gastrointestinal tract. Am J Physiol. 1991; 260:R200–R207.
Article6. Ruckley CV. A study of the variations of the abdominal vagi. Br J Surg. 1964; 51:569–573.
Article7. Ihasz M, Griffith CA. Gallstones after vagotomy. Am J Surg. 1981; 141:48–50.
Article8. Kojima K, Yamada H, Inokuchi M, Kawano T, Sugihara K. Functional evaluation after vagus-nerve-sparing laparoscopically assisted distal gastrectomy. Surg Endosc. 2008; 22:2003–2008.9. Shahidullah M, Kennedy TL, Parks TG. The vagus, the duodenal brake, and gastric emptying. Gut. 1975; 16:331–336.
Article10. Ando H, Mochiki E, Ohno T, Kogure N, Tanaka N, Tabe Y, et al. Effect of distal subtotal gastrectomy with preservation of the celiac branch of the vagus nerve to gastrointestinal function: an experimental study in conscious dogs. Ann Surg. 2008; 247:976–986.11. Tokunaga M, Hiki N, Fukunaga T, Ohyama S, Nunobe S, Yamada K, et al. Is preservation of the celiac branch of the vagal nerve effective in preventing stasis following pylorus-preserving gastrectomy? Hepatogastroenterology. 2011; 58:1046–1050.12. Sakuramoto S, Kikuchi S, Kuroyama S, Futawatari N, Katada N, Kobayashi N, et al. Laparoscopy-assisted distal gastrectomy for early gastric cancer: experience with 111 consecutive patients. Surg Endosc. 2006; 20:55–60.13. Uyama I, Sakurai Y, Komori Y, Nakamura Y, Syoji M, Tonomura S, et al. Laparoscopic gastrectomy with preservation of the vagus nerve accompanied by lymph node dissection for early gastric carcinoma. J Am Coll Surg. 2005; 200:140–145.
Article14. Yamada H, Kojima K, Inokuchi M, Kawano T, Sugihara K. Efficacy of celiac branch preservation in Roux-en-y reconstruction after laparoscopy-assisted distal gastrectomy. Surgery. 2011; 149:22–28.
Article15. Miyato H, Kitayama J, Hidemura A, Ishigami H, Kaisaki S, Nagawa H. Vagus nerve preservation selectively restores visceral fat volume in patients with early gastric cancer who underwent gastrectomy. J Surg Res. 2012; 173:60–67.
Article16. Furukawa H, Ohashi M, Honda M, Kumagai K, Nunobe S, Sano T, et al. Preservation of the celiac branch of the vagal nerve for pylorus-preserving gastrectomy: is it meaningful? Gastric Cancer. 2018; 21:516–523.
Article17. Kim SM, Cho J, Kang D, Oh SJ, Kim AR, Sohn TS, et al. A randomized controlled trial of vagus nerve-preserving distal gastrectomy versus conventional distal gastrectomy for postoperative quality of life in early stage gastric cancer patients. Ann Surg. 2016; 263:1079–1084.
Article18. Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011; 121:Suppl 1. S1–S16.
Article19. Slimp JC. Electrophysiologic intraoperative monitoring for spine procedures. Phys Med Rehabil Clin N Am. 2004; 15:85–105.
Article20. Evans MS, Verma-Ahuja S, Naritoku DK, Espinosa JA. Intraoperative human vagus nerve compound action potentials. Acta Neurol Scand. 2004; 110:232–238.
Article21. Ordelman SCMA, Kornet L, Cornelussen R, Buschman HPJ, Veltink PH. Average reference recording from the vagal nerve reveals an evoked indirect response. In : 2009 4th International IEEE/EMBS Conference on Neural Engineering; 2009 Apr 29–May 2; Antalya: IEEE;2009. p. 574–576.22. Koo B, Ham SD, Sood S, Tarver B. Human vagus nerve electrophysiology: a guide to vagus nerve stimulation parameters. J Clin Neurophysiol. 2001; 18:429–433.23. Familoni BO, Abell TL, Voeller G. Measurement of gastric and small bowel electrical activity at laparoscopy. J Laparoendosc Surg. 1994; 4:325–332.
Article24. Svedlund J, Sjödin I, Dotevall G. GSRS--a clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig Dis Sci. 1988; 33:129–134.
Article25. Kulich KR, Madisch A, Pacini F, Piqué JM, Regula J, Van Rensburg CJ, et al. Reliability and validity of the gastrointestinal symptom rating scale (GSRS) and quality of life in reflux and dyspepsia (QOLRAD) questionnaire in dyspepsia: a six-country study. Health Qual Life Outcomes. 2008; 6:12.
Article26. Sigstad H. A clinical diagnostic index in the diagnosis of the dumping syndrome. Changes in plasma volume and blood sugar after a test meal. Acta Med Scand. 1970; 188:479–486.27. De Neef KJ, Jansen JR, Versprille A. Developmental morphometry and physiology of the rabbit vagus nerve. Brain Res. 1982; 256:265–274.
Article28. Tosato M, Yoshida K, Toft E, Nekrasas V, Struijk JJ. Closed-loop control of the heart rate by electrical stimulation of the vagus nerve. Med Biol Eng Comput. 2006; 44:161–169.
Article29. Bortolotti M. Gastric electrical stimulation for gastroparesis: a goal greatly pursued, but not yet attained. World J Gastroenterol. 2011; 17:273–282.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A rare variation of the glossopharyngeal nerve
- Complete Atrioventricular Nodal Block in Patient Undergoing Left Vagus Nerve Stimulation: A case report
- Neurogenic pathways in remote ischemic preconditioning induced cardioprotection: Evidences and possible mechanisms
- Concurrent Ipsilateral Recurrent and Nonrecurrent Laryngeal Nerve During Thyroidectomy: A Case Report
- Neurilemmomas of the Cervicla Vagus Nerve: A Case Report