J Lipid Atheroscler.
2019 Sep;8(2):242-251. 10.12997/jla.2019.8.2.242.
Dyslipidemia and Rate of Under-Target Low-Density Lipoprotein-Cholesterol in Patients with Coronary Artery Disease in Korea
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. jangys1212@yuhs.ac
- 2Cardiovascular Division, Department of Internal Medicine, Korea University Ansan Hospital, Ansan, Korea.
- 3Department of Cardiovascular Medicine, Chonnam National University Hospital, Gwangju, Korea.
- 4Department of Cardiology, Keimyung University Hospital, Daegu, Korea.
- 5Division of Cardiology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 6Merck Sharp & Dohme (MSD), Seoul, Korea.
- 7Stiftung Institut für Herzinfarktforschung, Ludwigshafen, Germany.
- 8Klinikum der Stadt Ludwigshafen, Medizinische Klinik B, Ludwigshafen, Germany.
- 9Department of Epidemiology, School of Public Health, Rutgers University, Piscataway, NJ, USA.
- 10Merck & Co., Inc., Kenilworth, NJ, USA.
- KMID: 2458389
- DOI: http://doi.org/10.12997/jla.2019.8.2.242
Abstract
OBJECTIVE
The aim of this study was to evaluate under target rates of low-density lipoprotein-cholesterol (LDL-C) in Korean patients with stable coronary artery disease (CAD) or an acute coronary syndrome (ACS) in real world practice.
METHODS
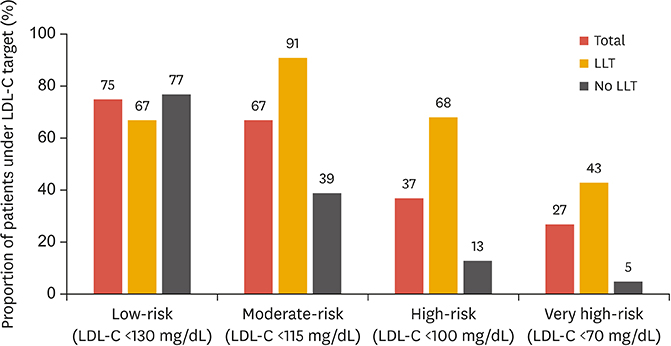
Dyslipidemia International Study II was an international observational study of patients with stable CAD or an ACS. Lipid profiles and use of lipid-lowering therapy (LLT) were documented at enrollment, and for the ACS cohort, 4 months follow-up was recommended. Rates of under target LDL-C as per European guidelines, were evaluated, and multivariate regression was performed to identify predictive factors of patients presenting under the target.
RESULTS
A total of 808 patients were enrolled in Korea, 500 with stable CAD and 308 with ACS. Of these, 90.6% and 52.6% were being treated with LLT, respectively. In the stable CAD group, 40.0% were under target LDL-C, while in ACS group, the rate was 23.7%. A higher statin dose was independently associated with under target LDL-C in both groups (OR, 1.03; p=0.046 [stable CAD] and OR, 1.05; p=0.01 [ACS]). The mean statin dosage (atorvastatin equivalent) was 17 mg/day. In the 79 ACS patients who underwent the follow-up examination, the LDL-C under target rate rose to 59.5%.
CONCLUSION
Only a minority of patients with stable CAD or ACS were under their target LDL-C level at enrollment. The statin dose was not sufficient in the majority of patients. These results indicate a considerable LLT gap in Korean patients with established CAD.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sungrae Kim
Diabetes Metab J. 2022;46(3):464-475. doi: 10.4093/dmj.2021.0088.
Reference
-
1. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005; 366:1267–1278.
Article2. Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016; 37:2999–3058.
Article3. Waters DD, Brotons C, Chiang CW, Ferrières J, Foody J, Jukema JW, et al. Lipid treatment assessment project 2: a multinational survey to evaluate the proportion of patients achieving low-density lipoprotein cholesterol goals. Circulation. 2009; 120:28–34.
Article4. Gitt AK, Drexel H, Feely J, Ferrières J, Gonzalez-Juanatey JR, Thomsen KK, et al. Persistent lipid abnormalities in statin-treated patients and predictors of LDL-cholesterol goal achievement in clinical practice in Europe and Canada. Eur J Prev Cardiol. 2012; 19:221–230.
Article5. Sung J, Kim SH, Song HR, Chi MH, Park JE. Lipid-lowering treatment practice patterns in Korea: comparison with the data obtained from the CEPHEUS Pan-Asian study. J Atheroscler Thromb. 2014; 21:1219–1227.
Article6. Chiang CE, Ferrières J, Gotcheva NN, Raal FJ, Shehab A, Sung J, et al. Suboptimal control of lipid levels: results from 29 countries participating in the Centralized Pan-Regional Surveys on the Undertreatment of Hypercholesterolaemia (CEPHEUS). J Atheroscler Thromb. 2016; 23:567–587.
Article7. American Diabetes Association. Standards of medical care in diabetes--2013. Diabetes Care. 2013; 36:Suppl 1. S11–S66.8. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003; 289:2560–2572.
Article9. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013; 34:2159–2219.10. Gitt AK, Lautsch D, Ferrières J, De Ferrari GM, Vyas A, Baxter CA, et al. Cholesterol target value attainment and lipid-lowering therapy in patients with stable or acute coronary heart disease: results from the Dyslipidemia International Study II. Atherosclerosis. 2017; 266:158–166.
Article11. Poh KK, Ambegaonkar B, Baxter CA, Brudi P, Buddhari W, Chiang FT, et al. Low-density lipoprotein cholesterol target attainment in patients with stable or acute coronary heart disease in the Asia-Pacific region: results from the Dyslipidemia International Study II. Eur J Prev Cardiol. 2018; 25:1950–1963.
Article12. Levin A, Stevens PE, Bilous RW, Coresh J, De Francisco ALM, De Jong PE, et al. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013; 3:1–150.13. European Association for Cardiovascular Prevention & Rehabilitation, Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, et al. ESC/EAS guidelines for the management of dyslipidaemias: the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011; 32:1769–1818.14. Weng TC, Yang YH, Lin SJ, Tai SH. A systematic review and meta-analysis on the therapeutic equivalence of statins. J Clin Pharm Ther. 2010; 35:139–151.
Article15. Lee JA, Sunwoo S, Kim YS, Oh HJ, Kang HC, Park KC, et al. Achieving recommended low density lipoprotein cholesterol goals and the factors associated with target achievement of hypercholesterolemia patients with rosuvastatin in primary care. Curr Med Res Opin. 2013; 29:751–760.
Article16. Hwang JY, Jung CH, Lee WJ, Park CY, Kim SR, Yoon KH, et al. Low density lipoprotein cholesterol target goal attainment rate and physician perceptions about target goal achievement in Korean patients with diabetes. Diabetes Metab J. 2011; 35:628–636.
Article17. Yu SH, Kang JG, Hwang YC, Ahn KJ, Yoo HJ, Ahn HY, et al. Increasing achievement of the target goals for glycemic, blood pressure and lipid control for adults with diagnosed diabetes in Korea. J Diabetes Investig. 2013; 4:460–465.
Article18. Kim HS, Wu Y, Lin SJ, Deerochanawong C, Zambahari R, Zhao L, et al. Current status of cholesterol goal attainment after statin therapy among patients with hypercholesterolemia in Asian countries and region: the Return on Expenditure Achieved for Lipid Therapy in Asia (REALITY-Asia) study. Curr Med Res Opin. 2008; 24:1951–1963.
Article19. Ho LT, Yin WH, Chuang SY, Tseng WK, Wu YW, Hsieh IC, et al. Determinants for achieving the LDL-C target of lipid control for secondary prevention of cardiovascular events in Taiwan. PLoS One. 2015; 10:e0116513.
Article20. Park JE, Chiang CE, Munawar M, Pham GK, Sukonthasarn A, Aquino AR, et al. Lipid-lowering treatment in hypercholesterolaemic patients: the CEPHEUS Pan-Asian survey. Eur J Prev Cardiol. 2012; 19:781–794.
Article21. Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med. 2000; 160:459–467.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug treatment of dyslipidemia
- Residual Cardiovascular Risk Remains Despite of Statin Treatment: Importance of High-Density Lipoprotein Cholesterol
- Mechanism, clinical consequences, and management of dyslipidemia in children with nephrotic syndrome
- Association between Coronary Artery Calcification and Carotid Plaque Using Health Check-Up Data
- Progression of Coronary Artery Disease after Percutaneous Transluminal Coronary Angioplasty