J Dent Anesth Pain Med.
2019 Aug;19(4):201-208. 10.17245/jdapm.2019.19.4.201.
Post-extraction pain in the adjacent tooth after surgical extraction of the mandibular third molar
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Wonkwang University, Iksan, Korea. cejoms@wku.ac.kr
- 2Wonkwang Research Institute, College of Dentistry, Wonkwang University, Iksan, Korea.
- 3Sanbon L Dental Clinic, Gunpo, Korea.
- 4Artificial Intelligence Research Institute of Society, Wonkwang University, Iksan, Korea.
- KMID: 2456011
- DOI: http://doi.org/10.17245/jdapm.2019.19.4.201
Abstract
- BACKGROUND
After tooth extraction, pain due to dry socket and pain in the adjacent tooth are common. The aim of this study was to retrospectively analyze pain in the adjacent tooth after surgical extraction of the mandibular third molar.
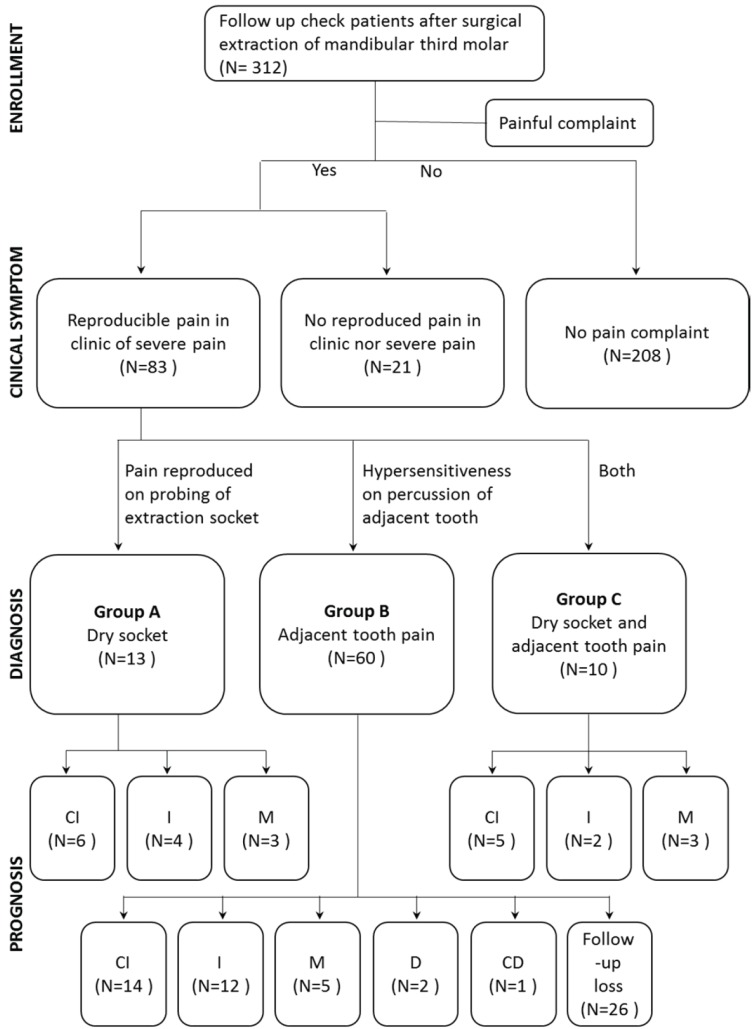
METHODS
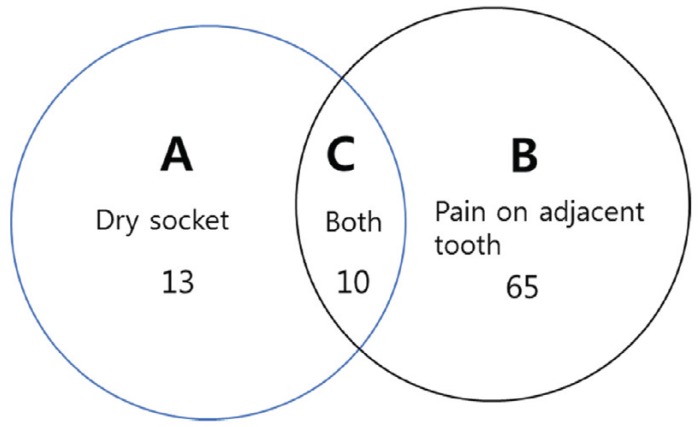
Postoperative pain due to dry socket, pain in the adjacent tooth, and pain from other causes were present. Group A included patents with dry socket alone; group B included patients with pain in the adjacent tooth alone; and group C included patients with both. The duration of symptoms was recorded. In addition, the prognosis of pain was divided into the complete improvement, improvement, maintenance, deterioration, and complete deterioration groups.
RESULTS
A total of 312 mandibular third molars were extracted from 13, 60, and 10 patients in groups A, B, and C, respectively. The mean duration of symptoms was 5 days in group A and B and 15.2 days in group C. There were statistically significant differences in the duration of symptoms between groups A and C and groups B and C.
CONCLUSION
Pain in the adjacent tooth after third molar extraction can be caused by inflammatory reactions and pressure on this tooth. The pain caused by pressure on the periodontal ligament and alveolar bone results from the cytokines released by osteoclasts, which are responsible for bone destruction. However, pain from periodontal ligament damage caused by excessive pressure may be misunderstood as pulpal pain. Unconscious parafunctional habits, such as clenching and bruxism, could also be associated with post-extraction pain.
Keyword
MeSH Terms
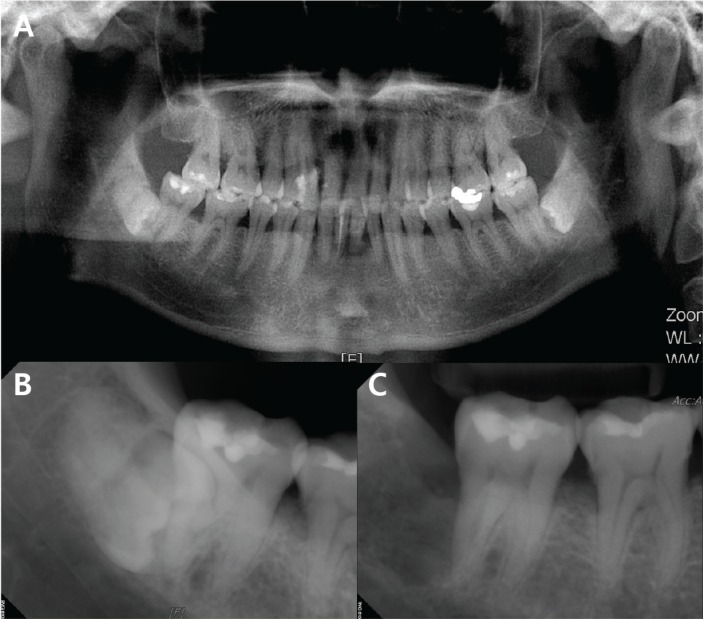
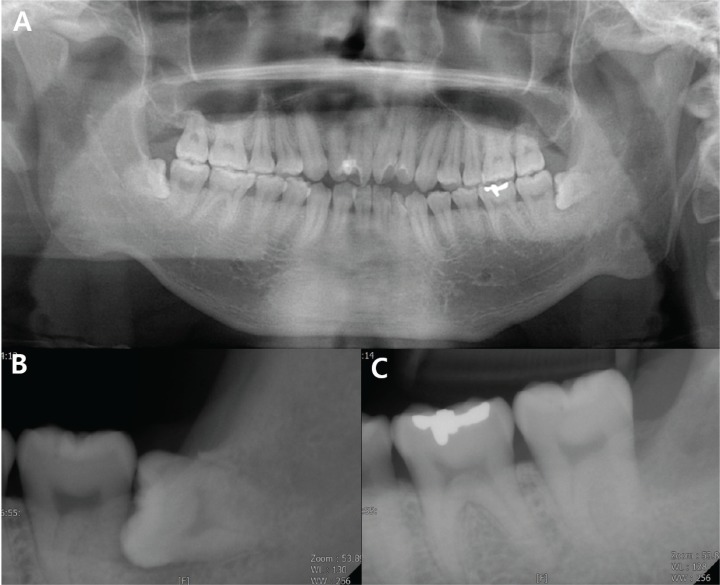
Figure
Reference
-
1. Jüri K. Alling CC, Helfrick JF, Alling RD, editors. Impacted Teeth. 1st ed. Philadelphia: Saunders Co;1993. p. 371.2. Haug RH, Perrott DH, Gonzalez ML, Talwar RM. The American Association of Oral and Maxillofacial Surgeons age-related third molar study. J Oral Maxillofac Surg. 2005; 63:1106–1114. PMID: 16094577.
Article3. Osborn TP, Frederickson G Jr, Small IA, Torgerson TS. A prospective study of complications related to mandibular third molar surgery. J Oral Maxillofac Surg. 1985; 43:767–769. PMID: 2995624.
Article4. Bouloux GF, Steed MB, Perciaccante VJ. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am. 2007; 19:117–128. PMID: 18088870.
Article5. Bui CH, Seldin EB, Dodson TD. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003; 61:1379–1389. PMID: 14663801.
Article6. Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain. 1997; 69:1–18. PMID: 9060007.
Article7. Miki K, Honma S, Ebara S, Kumamoto K, Murakami S, Wakisaka S. Changes in the distribution of periodontal nerve fibers during dentition transition in the cat. PLoS One. 2015; 10:e0129826. PMID: 26083023.
Article8. Cho TJ, Gerstenfeld LC, Einhorn TA. Differential temporal expression of members of the transforming growth factor beta superfamily during murine fracture healing. J Bone Miner Res. 2002; 17:513–520. PMID: 11874242.9. Gerstenfeld LC, Cullinane DM, Barnes GL, Graves DT, Einhorn TA. Fracture healing as a post-natal developmental process: molecular, spatial, and temporal aspects of its regulation. J Cell Biochem. 2003; 88:873–884. PMID: 12616527.
Article10. De Jongh RF, Vissers KC, Meert TF, Booij LH, De Deyne CS, Heylen RJ. The role of interleukin-6 in nociception and pain. Anesth Analg. 2003; 96:1096–1103. PMID: 12651667.
Article11. Ikeda T, Nakano M, Brando E, Suzuki A. The effect of traumatic occlusal contact on tooth pain threshold in humans. J Oral Rehabil. 1998; 25:589–595. PMID: 9781861.12. Gulabivala K, Ng YL. Tooth organogenesis, morphology and physiology. Endodontics. 4th ed. St. Louis: Mosby;2014. p. 2–32.13. Polson AM, Zander HA. Effect of periodontal trauma upon intrabony pockets. J Periodontol. 1983; 54:586–591. PMID: 6580411.
Article14. Lindhe J, Ericsson I. The influence of trauma from occlusion on reduced but healthy periodontal tissues in dogs. J Clin Periodontol. 1976; 3:110–122. PMID: 1064595.
Article15. Feller L, Khammissa RA, Schechter I, Thomadakis G, Fourie J, Lemmer J. Biological events in periodontal ligament and alveolar bone associated with application of orthodontic forces. ScientificWorldJournal. 2015; 2015:876509. PMID: 26421314.
Article16. Ramfjord SP, Ash MM Jr. Significance of occlusion in the etiology and treatment of early, moderate and advanced periodontitis. J Periodontol. 1981; 52:511–517. PMID: 6793705.
Article17. Bjorndahl O. Periodontal traumatism. J Periodontol. 1958; 29:223–231.
Article18. Glover ME. Occlusal therapy and its role in the etiology and treatment of periodontal diseases. Tex Dent J. 1988; 105:18–22.19. Wank GS, Kroll YJ. Occlusal trauma. An evaluation of its relationship to periodontal prostheses. Dent Clin North Am. 1981; 25:511–532. PMID: 7021239.20. Burgett FG. Trauma from occlusion. Periodontal concerns. Dent Clin North Am. 1995; 39:301–311. PMID: 7781828.21. Hattner R, Epker BN, Frost HM. Suggested sequential mode of control of changes in cell behaviour in adult bone remodelling. Nature. 1965; 206:489–490. PMID: 5319106.
Article22. Hughes JM, Petit MA. Biological underpinning of Frost's mechanostat thresholds: The important role of osteocytes. J Musculoskelet Neuronal Interact. 2010; 10:128–135. PMID: 20516629.23. Verborgt O, Gibson GJ, Schaffler MB. Loss of osteocyte integrity in association with microdamage and bone remodeling after fatigue in vivo. J Bone Miner Res. 2000; 15:60–67. PMID: 10646115.
Article24. Bentolila V, Boyce TM, Fyhrie DP, Drumb R, Skerry TM, Schaffler MB. Intracortical remodeling in adult rat long bones after fatigue loading. Bone. 1998; 23:275–281. PMID: 9737350.
Article25. Benemei S, Nicoletti P, Capone JG, Geppetti P. CGRP receptors in the control of pain and inflammation. Curr Opin Pharmacol. 2009; 9:9–14. PMID: 19157980.
Article26. Roqué M, Martinez MJ, Alonso P, Català E, Garcia JL, Ferrandiz M. Radioisotopes for metastatic bone pain. Cochrane Database Syst Rev. 2003; (4):CD003347. PMID: 14583970.
Article27. Kvinnsland I, Heyeraas KJ. Effect of traumatic occlusion on CGRP and SP immunoreactive nerve fibre morphology in rat molar pulp and periodontium. Histochemistry. 1992; 97:111–120. PMID: 1373126.
Article28. Waerhaug J. Pathogenesis of pocket formation in traumatic occlusion. J Periodontol. 1955; 26:107–118.
Article29. Roberts WE. Bone physiology, metabolism, and biomechanics in orthodontic practice. In : Graber TM, Vanarsdall RL, editors. Orthodontics: Current Principles and Techniques. 2nd ed. St Louis: Mosby;1994. p. 193–234.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on the second molar which was malpositioned after orthodontic treatment
- Management of the Third Molar Tooth in Mandibular Angle Fracture
- The anxiety in patients undergoing third molar extraction
- Pressure Root Resorption of the Second Molar Caused by Third Molar Impaction: A Case Report of Severely Resorbed Root with Vital Pulp
- The influence of mandibular third molar on mandibular angle fracture