Korean J Radiol.
2019 Sep;20(9):1368-1380. 10.3348/kjr.2019.0057.
A Stepwise Diagnostic Approach to Cystic Lung Diseases for Radiologists
- Affiliations
-
- 1Department of Radiology, Korea University Guro Hospital, College of Medicine, Korea University, Seoul, Korea. keyrad@korea.ac.kr
- 2Department of Radiology, Korea University Ansan Hospital, College of Medicine, Korea University, Ansan, Korea.
- 3Department of Radiology, Korea University Anam Hospital, College of Medicine, Korea University, Seoul, Korea.
- KMID: 2455765
- DOI: http://doi.org/10.3348/kjr.2019.0057
Abstract
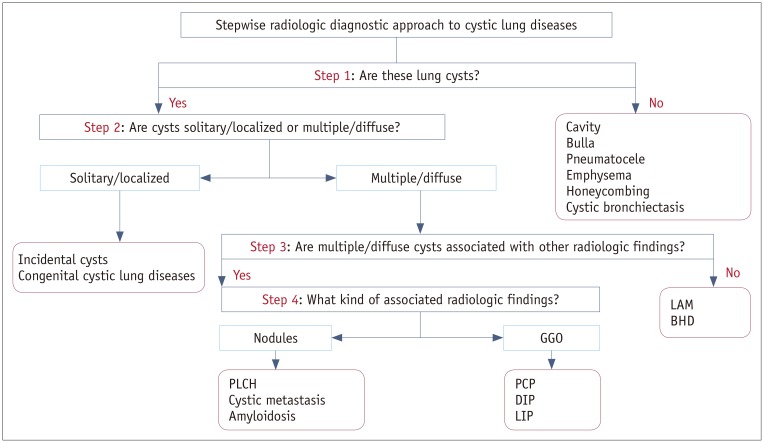
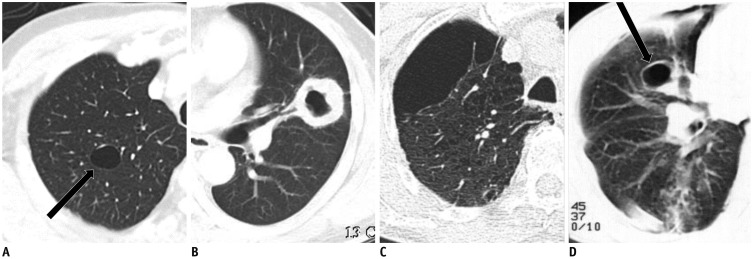
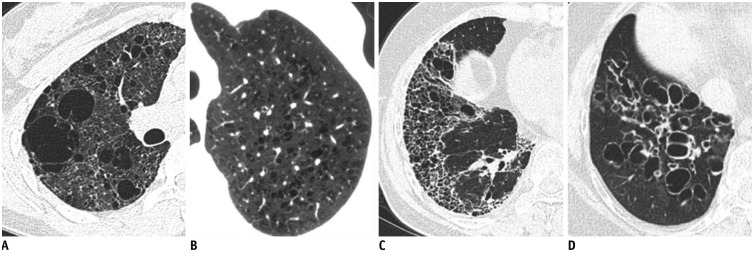
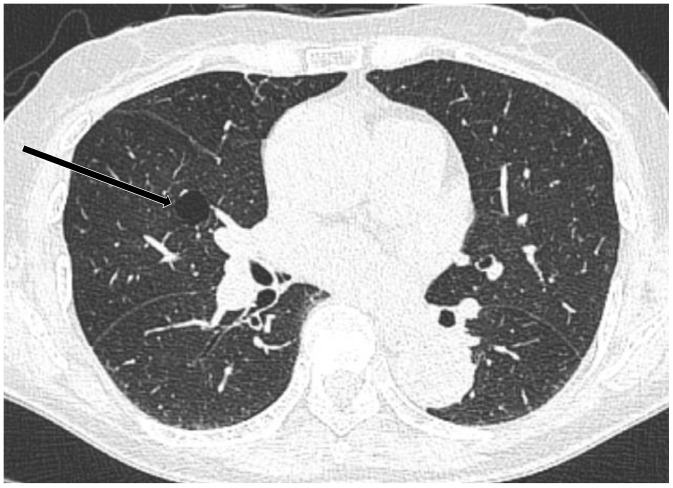
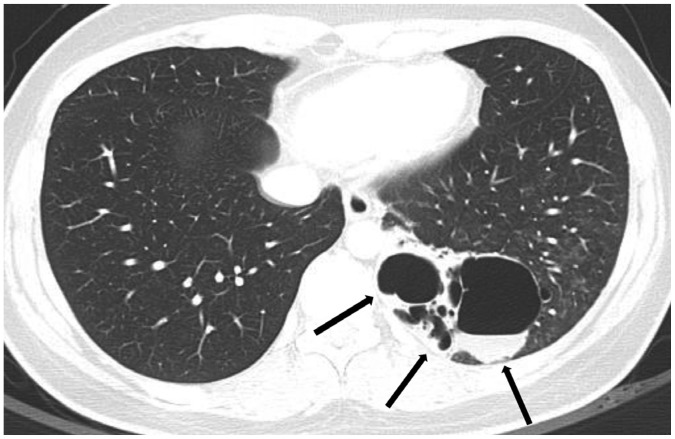
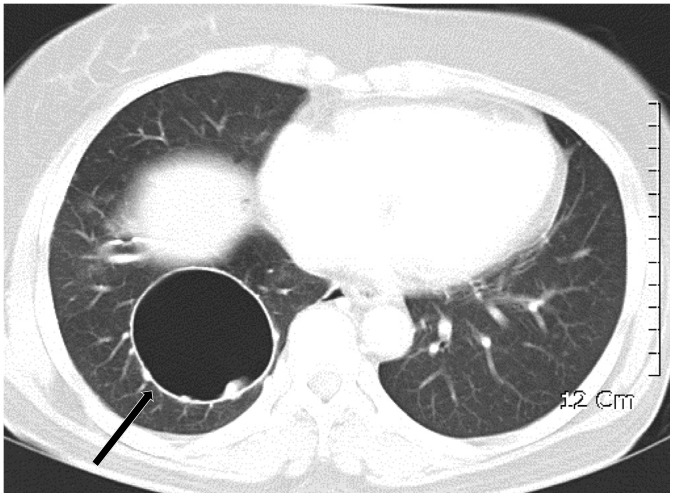
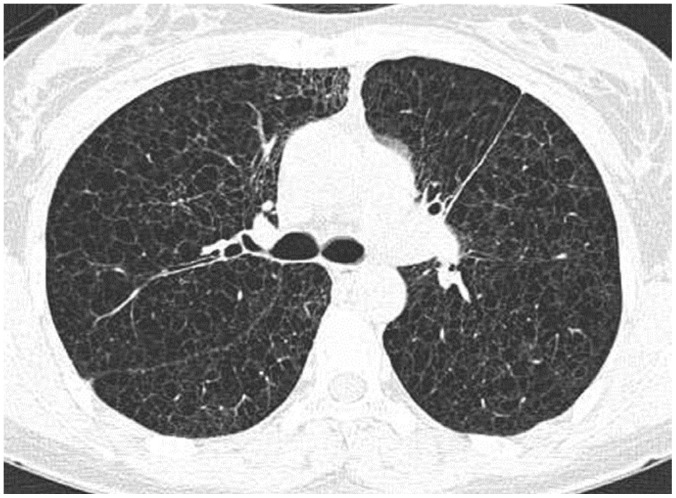
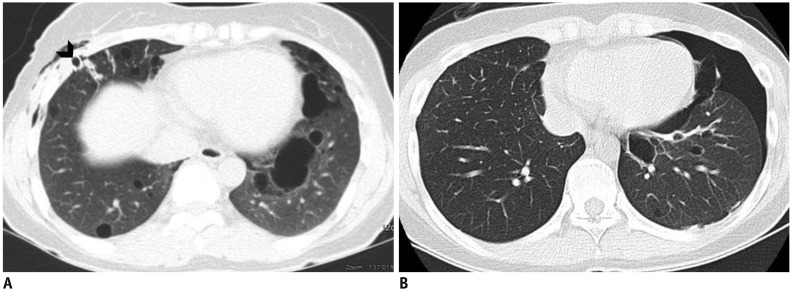
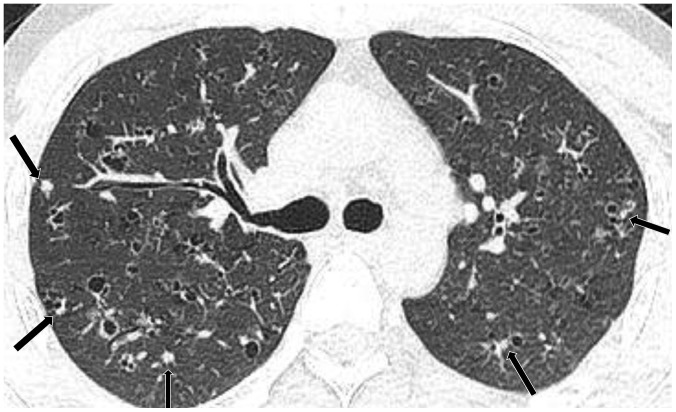
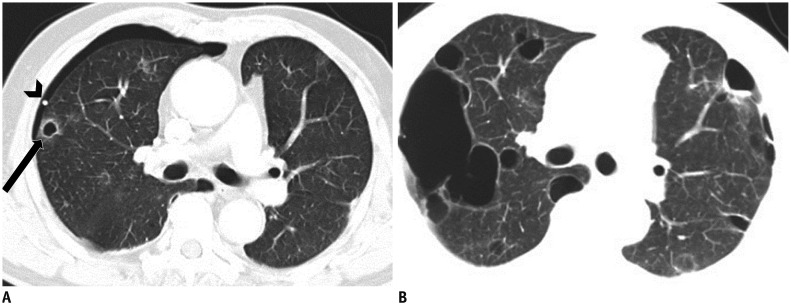
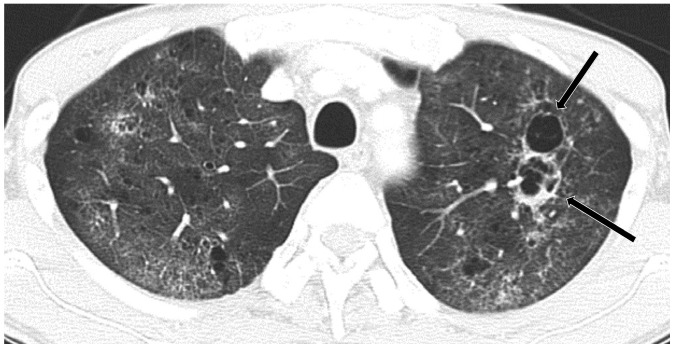
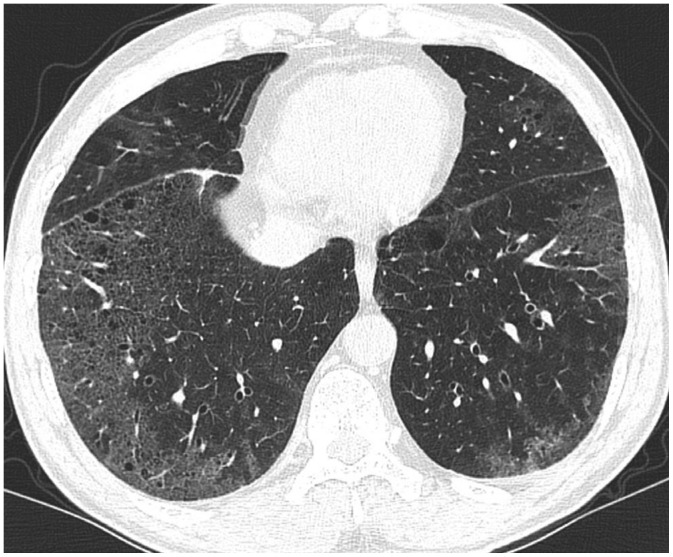
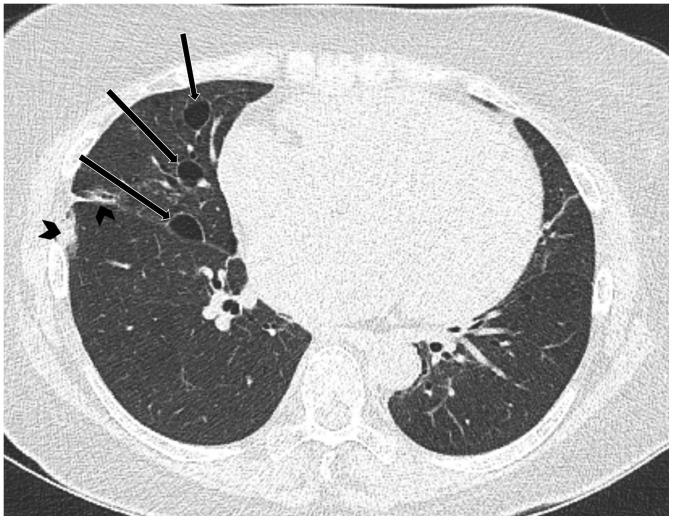
- Lung cysts are commonly seen on computed tomography (CT), and cystic lung diseases show a wide disease spectrum. Thus, correct diagnosis of cystic lung diseases is a challenge for radiologists. As the first diagnostic step, cysts should be distinguished from cavities, bullae, pneumatocele, emphysema, honeycombing, and cystic bronchiectasis. Second, cysts can be categorized as single/localized versus multiple/diffuse. Solitary/localized cysts include incidental cysts and congenital cystic diseases. Multiple/diffuse cysts can be further categorized according to the presence or absence of associated radiologic findings. Multiple/diffuse cysts without associated findings include lymphangioleiomyomatosis and Birt-Hogg-Dubé syndrome. Multiple/diffuse cysts may be associated with ground-glass opacity or small nodules. Multiple/diffuse cysts with nodules include Langerhans cell histiocytosis, cystic metastasis, and amyloidosis. Multiple/diffuse cysts with ground-glass opacity include pneumocystis pneumonia, desquamative interstitial pneumonia, and lymphocytic interstitial pneumonia. This stepwise radiologic diagnostic approach can be helpful in reaching a correct diagnosis for various cystic lung diseases.
Keyword
MeSH Terms
Figure
Reference
-
1. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008; 246:697–722. PMID: 18195376.
Article2. Gupta N, Vassallo R, Wikenheiser-Brokamp KA, McCormack FX. Diffuse cystic lung disease. Part II. Am J Respir Crit Care Med. 2015; 192:17–29. PMID: 25906201.
Article3. Ryu JH, Swensen SJ. Cystic and cavitary lung diseases: focal and diffuse. Mayo Clin Proc. 2003; 78:744–752. PMID: 12934786.
Article4. Gafoor K, Patel S, Girvin F, Gupta N, Naidich D, Machnicki S, et al. Cavitary lung diseases: a clinical-radiologic algorithmic approach. Chest. 2018; 153:1443–1465. PMID: 29518379.5. Parkar AP, Kandiah P. Differential diagnosis of cavitary lung lesions. J Belg Soc Radiol. 2016; 100:100. PMID: 30151493.
Article6. Beigelman-Aubry C, Godet C, Caumes E. Lung infections: the radiologist's perspective. Diagn Interv Imaging. 2012; 93:431–440. PMID: 22658280.
Article7. Lynch DA, Austin JH, Hogg JC, Grenier PA, Kauczor HU, Bankier AA, et al. CT-definable subtypes of chronic obstructive pulmonary disease: a statement of the Fleischner Society. Radiology. 2015; 277:192–205. PMID: 25961632.
Article8. Takahashi M, Fukuoka J, Nitta N, Takazakura R, Nagatani Y, Murakami Y, et al. Imaging of pulmonary emphysema: a pictorial review. Int J Chron Obstruct Pulmon Dis. 2008; 3:193–204. PMID: 18686729.9. Ha D, Yadav R, Mazzone PJ. Cystic lung disease: systematic, stepwise diagnosis. Cleve Clin J Med. 2015; 82:115–127. PMID: 25897602.
Article10. Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. American Thoracic Society. European Respiratory Society. Japanese Respiratory Society. Latin American Thoracic Society. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018; 198:e44–e68. PMID: 30168753.
Article11. Copley SJ, Wells AU, Hawtin KE, Gibson DJ, Hodson JM, Jacques AE, et al. Lung morphology in the elderly: comparative CT study of subjects over 75 years old versus those under 55 years old. Radiology. 2009; 251:566–573. PMID: 19401580.
Article12. Araki T, Nishino M, Gao W, Dupuis J, Putman RK, Washko GR, et al. Pulmonary cysts identified on chest CT: are they part of aging change or of clinical significance? Thorax. 2015; 70:1156–1162. PMID: 26514407.
Article13. Raoof S, Bondalapati P, Vydyula R, Ryu JH, Gupta N, Raoof S, et al. Cystic lung diseases: algorithmic approach. Chest. 2016; 150:945–965. PMID: 27180915.14. Biyyam DR, Chapman T, Ferguson MR, Deutsch G, Dighe MK. Congenital lung abnormalities: embryologic features, prenatal diagnosis, and postnatal radiologic-pathologic correlation. Radiographics. 2010; 30:1721–1738. PMID: 21071385.
Article15. Odev K, Guler I, Altinok T, Pekcan S, Batur A, Ozbiner H. Cystic and cavitary lung lesions in children: radiologic findings with pathologic correlation. J Clin Imaging Sci. 2013; 3:60. PMID: 24605255.
Article16. Zylak CJ, Eyler WR, Spizarny DL, Stone CH. Developmental lung anomalies in the adult: radiologic-pathologic correlation. Radiographics. 2002; 22 Spec No:S25–S43. PMID: 12376599.
Article17. Yoon YC, Lee KS, Kim TS, Kim J, Shim YM, Han J. Intrapulmonary bronchogenic cyst: CT and pathologic findings in five adult patients. AJR Am J Roentgenol. 2002; 179:167–170. PMID: 12076928.
Article18. Kalassian KG, Doyle R, Kao P, Ruoss S, Raffin TA. Lymphangioleiomyomatosis: new insights. Am J Respir Crit Care Med. 1997; 155:1183–1186. PMID: 9105053.
Article19. Pallisa E, Sanz P, Roman A, Majó J, Andreu J, Cáceres J. Lymphangioleiomyomatosis: pulmonary and abdominal findings with pathologic correlation. Radiographics. 2002; 22 Spec No:S185–S198. PMID: 12376610.
Article20. Baldi BG, Carvalho CRR, Dias OM, Marchiori E, Hochhegger B. Diffuse cystic lung diseases: differential diagnosis. J Bras Pneumol. 2017; 43:140–149. PMID: 28538782.
Article21. Umeoka S, Koyama T, Miki Y, Akai M, Tsutsui K, Togashi K. Pictorial review of tuberous sclerosis in various organs. Radiographics. 2008; 28:e32. PMID: 18772274.
Article22. Seaman DM, Meyer CA, Gilman MD, McCormack FX. Diffuse cystic lung disease at high-resolution CT. AJR Am J Roentgenol. 2011; 196:1305–1311. PMID: 21606293.
Article23. Kitaichi M, Nishimura K, Itoh H, Izumi T. Pulmonary lymphangioleiomyomatosis: a report of 46 patients including a clinicopathologic study of prognostic factors. Am J Respir Crit Care Med. 1995; 151(2 Pt 1):527–533. PMID: 7842216.
Article24. Menko FH, van Steensel MA, Giraud S, Friis-Hansen L, Richard S, Ungari S, et al. European BHD Consortium. Birt-Hogg-Dubé syndrome: diagnosis and management. Lancet Oncol. 2009; 10:1199–1206. PMID: 19959076.
Article25. Tobino K, Hirai T, Johkoh T, Kurihara M, Fujimoto K, Tomiyama N, et al. Differentiation between Birt-Hogg-Dubé syndrome and lymphangioleiomyomatosis: quantitative analysis of pulmonary cysts on computed tomography of the chest in 66 females. Eur J Radiol. 2012; 81:1340–1346. PMID: 21550193.
Article26. Agarwal PP, Gross BH, Holloway BJ, Seely J, Stark P, Kazerooni EA. Thoracic CT findings in Birt-Hogg-Dubé syndrome. AJR Am J Roentgenol. 2011; 196:349–352. PMID: 21257886.
Article27. Toro JR, Pautler SE, Stewart L, Glenn GM, Weinreich M, Toure O, et al. Lung cysts, spontaneous pneumothorax, and genetic associations in 89 families with Birt-Hogg-Dubé syndrome. Am J Respir Crit Care Med. 2007; 175:1044–1053. PMID: 17322109.
Article28. Tobino K, Gunji Y, Kurihara M, Kunogi M, Koike K, Tomiyama N, et al. Characteristics of pulmonary cysts in Birt-Hogg-Dubé syndrome: thin-section CT findings of the chest in 12 patients. Eur J Radiol. 2011; 77:403–409. PMID: 19782489.
Article29. Abbott GF, Rosado-de-Christenson ML, Franks TJ, Frazier AA, Galvin JR. From the archives of the AFIP: pulmonary Langerhans cell histiocytosis. Radiographics. 2004; 24:821–841. PMID: 15143231.30. Yogi A, Miyara T, Ogawa K, Iraha S, Matori S, Haranaga S, et al. Pulmonary metastases from angiosarcoma: a spectrum of CT findings. Acta Radiol. 2016; 57:41–46. PMID: 25711232.
Article31. Tateishi U, Hasegawa T, Kusumoto M, Yamazaki N, Iinuma G, Muramatsu Y, et al. Metastatic angiosarcoma of the lung: spectrum of CT findings. AJR Am J Roentgenol. 2003; 180:1671–1674. PMID: 12760941.
Article32. Cantin L, Bankier AA, Eisenberg RL. Multiple cystlike lung lesions in the adult. AJR Am J Roentgenol. 2010; 194:W1–W11. PMID: 20028879.
Article33. Czeyda-Pommersheim F, Hwang M, Chen SS, Strollo D, Fuhrman C, Bhalla S. Amyloidosis: modern cross-sectional imaging. Radiographics. 2015; 35:1381–1392. PMID: 26230754.
Article34. Zamora AC, White DB, Sykes AM, Hoskote SS, Moua T, Yi ES, et al. Amyloid-associated cystic lung disease. Chest. 2016; 149:1223–1233. PMID: 26513525.
Article35. Georgiades CS, Neyman EG, Barish MA, Fishman EK. Amyloidosis: review and CT manifestations. Radiographics. 2004; 24:405–416. PMID: 15026589.
Article36. Kanne JP, Yandow DR, Meyer CA. Pneumocystis jiroveci pneumonia: high-resolution CT findings in patients with and without HIV infection. AJR Am J Roentgenol. 2012; 198:W555–W561. PMID: 22623570.
Article37. Boiselle PM, Crans CA Jr, Kaplan MA. The changing face of pneumocystis carinii pneumonia in AIDS patients. AJR Am J Roentgenol. 1999; 172:1301–1309. PMID: 10227507.
Article38. Godbert B, Wissler MP, Vignaud JM. Desquamative interstitial pneumonia: an analytic review with an emphasis on aetiology. Eur Respir Rev. 2013; 22:117–123. PMID: 23728865.
Article39. Travis WD, Costabel U, Hansell DM, King TE Jr, Lynch DA, Nicholson AG, ATS/ERS Committee on Idiopathic Interstitial Pneumonias, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013; 188:733–748. PMID: 24032382.
Article40. Gupta N, Vassallo R, Wikenheiser-Brokamp KA, McCormack FX. Diffuse cystic lung disease. Part I. Am J Respir Crit Care Med. 2015; 191:1354–1366. PMID: 25906089.
Article41. Gupta N, Colby TV, Meyer CA, McCormack FX, Wikenheiser-Brokamp KA. Smoking-related diffuse cystic lung disease. Chest. 2018; 154:e31–e35. PMID: 30080520.42. Attili AK, Kazerooni EA, Gross BH, Flaherty KR, Myers JL, Martinez FJ. Smoking-related interstitial lung disease: radiologic-clinical-pathologic correlation. Radiographics. 2008; 28:1383–1396. discussion 1396–1398. PMID: 18794314.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- DILD (diffuse infiltrative lung disease); Radiologic Diagnostic Approach According to High-Resolution CT Pattern
- Cystic Lung Disease: a Comparison of C ystic Size, as Seen on Expira tory and Inspiratory HRCT Scans
- Congenital cystic diseases of the lung
- Pathologic Review of Cystic and Cavitary Lung Diseases
- Future Supply of and Demand for Diagnostic Radiologists in Korea