J Korean Orthop Assoc.
2019 Aug;54(4):327-335. 10.4055/jkoa.2019.54.4.327.
Surgical Treatment of Osteoporotic Vertebral Compression Fractures at Thoraco-Lumbar Levels: Only Pedicle Screw Constructs with Polymethylmethacrylate Augmentation
- Affiliations
-
- 1Department of Orthopedic Surgery, Gachon University Gil Medical Center, Incheon, Korea. bbaik@hanmail.net
- KMID: 2455501
- DOI: http://doi.org/10.4055/jkoa.2019.54.4.327
Abstract
- PURPOSE
To investigate the radiological efficacy of polymethylmethacrylate (PMMA) augmentation of pedicle screw operation in osteoporotic vertebral compression fractures (OVCF) patients.
MATERIALS AND METHODS
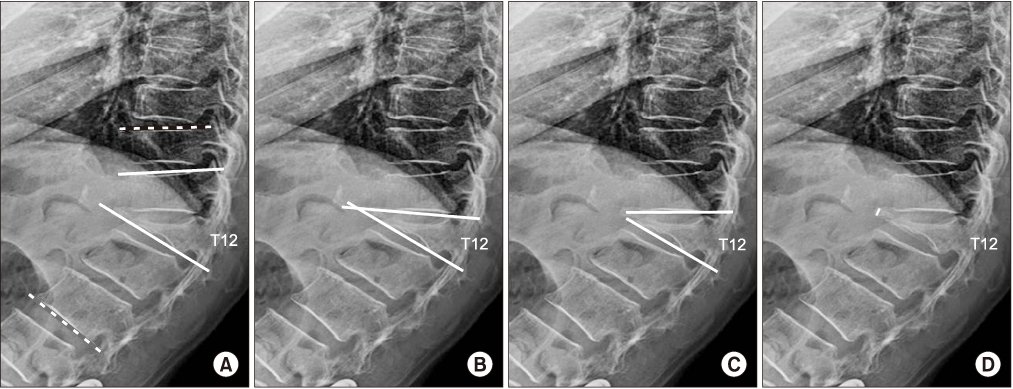
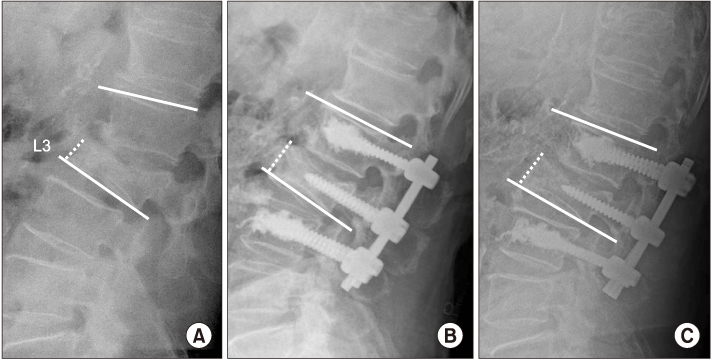
Twenty OVCF patients, who underwent only posterior fusion using pedicle screws with PMMA augmentation, were included in the study. The mean follow-up period was 15.6 months. The demographic data, bone mineral density (BMD), fusion segments, number of pedicle screws, and amount of PMMA were reviewed as medical records. To analyze the radiological outcomes, the radiologic parameters were measured as the time serial follow-up (preoperation, immediately postoperation, postoperation 6 weeks, 3, 6 months, and 1 year follow-up).
RESULTS
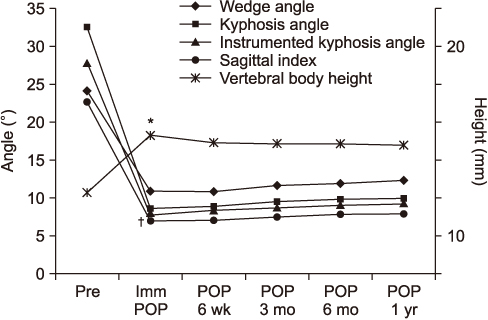
A total of 20 patients were examined (16 females [80.0%]; mean age, 69.1±8.9 years). The average BMD was −2.5±0.9 g/cm2. The average cement volume per vertebral body was 6.3 ml. The mean preoperative Cobb angle of focal kyphosis was 32.7°±7.0° and was improved significantly to 8.7°±6.9° postoperatively (p<0.001), with maintenance of the correction at the serial follow-up, postoperatively. The Cobb angle of instrumented kyphosis, wedge angle, and sagittal index showed similar patterns. In addition, the anterior part of fractured vertebral body height averaged 11.0±5.0 mm and was improved to 18.5±5.7 mm postoperatively (p=0.006), with maintenance of the improvement at the 3-month, 6-month, and 1-year follow-up.
CONCLUSION
The reinforcement of pedicle screws using PMMA augmentation may be a feasible surgical technique for OVCF. Moreover, it appears to be appropriate for improving the focal thoracolumbar/lumbar kyphosis and is maintained well after surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Melton LJ 3rd. Epidemiology of spinal osteoporosis. Spine (Phila Pa 1976). 1997; 22:2S–11S.
Article2. Rowe SM, Yoon TR, Ryang DH. An epidemiological study of hip fracture in Honam, Korea. Int Orthop. 1993; 17:139–143.
Article3. Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res. 1986; (203):7–17.
Article4. Shikata J, Yamamuro T, Iida H, Shimizu K, Yoshikawa J. Surgical treatment for paraplegia resulting from vertebral fractures in senile osteoporosis. Spine (Phila Pa 1976). 1990; 15:485–489.
Article5. Baba H, Maezawa Y, Kamitani K, Furusawa N, Imura S, Tomita K. Osteoporotic vertebral collapse with late neurological complications. Paraplegia. 1995; 33:281–289.
Article6. Sarzier JS, Evans AJ, Cahill DW. Increased pedicle screw pull-out strength with vertebroplasty augmentation in osteoporotic spines. J Neurosurg. 2002; 96:S309–S312.
Article7. Soshi S, Shiba R, Kondo H, Murota K. An experimental study on transpedicular screw fixation in relation to osteoporosis of the lumbar spine. Spine (Phila Pa 1976). 1991; 16:1335–1341.
Article8. Wittenberg RH, Lee KS, Shea M, White AA 3rd, Hayes WC. Effect of screw diameter, insertion technique, and bone cement augmentation of pedicular screw fixation strength. Clin Orthop Relat Res. 1993; (296):278–287.
Article9. Cook SD, Salkeld SL, Stanley T, Faciane A, Miller SD. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J. 2004; 4:402–408.10. Cohen D, Cullinane D, Iizuka M, Walk N, Kostuik J. Biomechanics of pedicle screw augmentation using polymethylmethacrylate. New Orleans: North American Spine Society;2000.11. Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994; 19:2415–2420.
Article12. McLain RF, McKinley TO, Yerby SA, Smith TS, Sarigul-Klijn N. The effect of bone quality on pedicle screw loading in axial instability. A synthetic model. Spine (Phila Pa 1976). 1997; 22:1454–1460.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Vertebral Augmentation for the Treatment of Osteoporotic Spinal Fractures
- Short Segment Pedicle Screw Fixation with Augmented Intra-Operative Vertebroplasty in Unstable Thoraco-Lumbar Fracture: Preliminary Report
- Surgical Treatment for Lumbar Spinal Stenosis with Fracture in Multiple Osteoporotic Compression Fractures
- Posterior Surgery with Selective Anterior Reinforcement and Screw Augmentation for a Delayed Myelopathy from an Osteoporotic Vertebral Compression Fracture
- Strategies for Vertebral Augmentation and Increasing Pedicle Screw Purchase in the Osteoporotic Spine Surgery