J Korean Ophthalmol Soc.
2019 Aug;60(8):792-796. 10.3341/jkos.2019.60.8.792.
Radial Keratoneuritis in Aeromonas Keratitis
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. sieh12@schmc.ac.kr
- 2Department of Laboratory Medicine and Genetics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea.
- KMID: 2455463
- DOI: http://doi.org/10.3341/jkos.2019.60.8.792
Abstract
- PURPOSE
We report a case of Aeromonas keratitis presenting as radial keratoneuritis.
CASE SUMMARY
A 33-year-old woman with a history of cleaning her contact lenses with tap water presented with decreased visual acuity for 1 day in the left eye. The patient showed diffuse corneal edema, stromal infiltration, and radial keratoneuritis, which were thought to be pathognomonic for Aeromonas keratitis. Based on the patient's clinical findings and past history, a diagnosis of Aeromonas keratitis was made and she was prescribed topical fortified cefazolin (50 mg/mL, 5%), tobramycin (3 mg/mL), and 0.02% chlorhexidine per hour. Culture results from the contact lens and contact lens solution confirmed infection by Aeromonas hydrophilia. Polymerase chain reaction results for Aeromonas were negative. After 8 days of treatment, the uncorrected visual acuity was 0.7/0.3 with improvement in her corneal findings.
CONCLUSIONS
Radial keratoneuritis is not always pathognomic for Aeromonas keratitis and can be present in Aeromonas keratitis. Therefore, ophthalmologists should be cautious when interpreting this clinical sign.
Keyword
MeSH Terms
Figure
Reference
-
1. Naginton J, Watson PG, Playfair TJ, et al. Amoebic infection of the eye. Lancet. 1974; 2:1537–1540.2. Lorenzo-Morales J, Khan NA, Walochnik J. An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment. Parasite. 2015; 22:10.3. Moore MB, McCulley JP, Kaufman HE, Robin JB. Radial keratoneuritis as a presenting sign in Acanthamoeba keratitis. Ophthalmology. 1986; 93:1310–1315.4. Feist RM, Sugar J, Tessler H. Radial keratoneuritis in Pseudomonas keratitis. Arch Ophthalmol. 1991; 109:774–775.
Article5. Mutoh T, Matsumoto Y, Chikuda M. A case of radial keratoneuritis in non-Acanthamoeba keratitis. Clin Ophthalmol. 2012; 6:1535–1538.
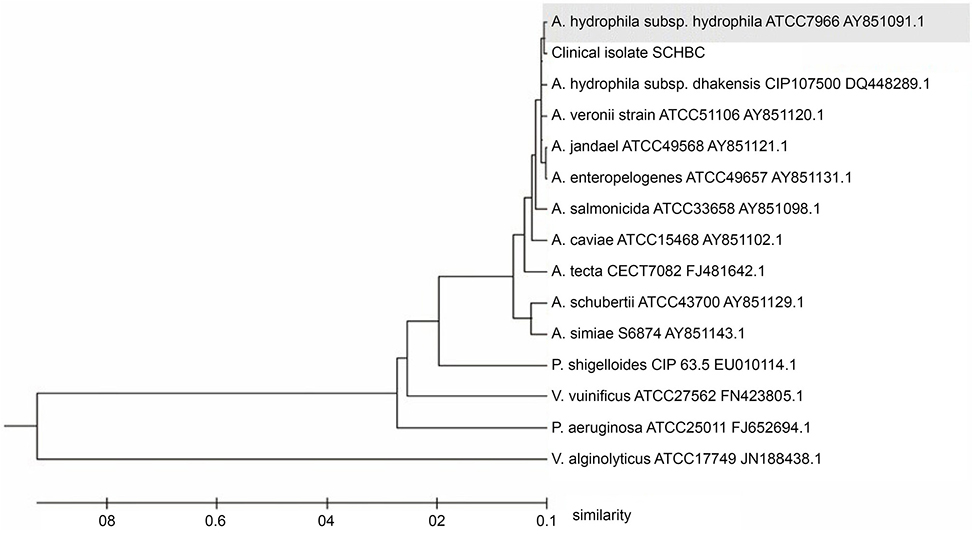
Article6. Shin HB, Yoon J, Lee Y, et al. Comparison of MALDI-TOF MS, housekeeping gene sequencing, and 16S rRNA gene sequencing for identification of Aeromonas clinical isolates. Yonsei Med J. 2015; 56:550–555.7. Tamura K, Peterson D, Peterson N, et al. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011; 28:2731–2739.
Article8. Lehmann OJ, Green SM, Morlet N, et al. Polymerase chain reaction analysis of corneal epithelial and tear samples in the diagnosis of Acanthamoeba keratitis. Invest Ophthalmol Vis Sci. 1998; 39:1261–1265.9. Kim YJ, Kim BS, Yoo WS, et al. A case of serratia marcescens keratitis presenting as radial keratoneuritis. J Korean Ophthalmol Soc. 2014; 55:1380–1383.10. Shilkin KB, Annear DI, Rowett LR, Laurence BH. Infection due to Aeromonas hydrophila. Med J Aust. 1968; 1:351–353.11. Feaster FT, Nisbet RM, Barber JC. Aeromonas hydrophila corneal ulcer. Am J Ophthalmol. 1978; 85:114–117.
Article12. Pinna A, Sechi LA, Zanetti S, et al. Aeromonas caviae keratitis associated with contact lens wear. Ophthalmology. 2004; 111:348–351.
Article13. Motukupally SR, Singh A, Garg P, Sharma S. Microbial keratitis due to aeromonas species at a tertiary eye care center in Southern India. Asia Pac J Ophthalmol (Phila). 2014; 3:294–298.
Article14. Persson S, Al-Shuweli S, Yapici S, et al. Identification of clinical aeromonas species by rpoB and gyrB sequencing and development of a multiplex PCR method for detection of Aeromonas hydrophila, A. caviae, A. veronii, and A. media. J Clin Microbiol. 2015; 53:653–656.15. Roels D, De Craene S, Kestelyn P. Keratoneuritis is not pathognomonic of Acanthamoeba keratitis: a case report of Pseudomonas keratitis. Int Ophthalmol. 2017; 37:257–258.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Serratia Marcescens Keratitis Presenting as Radial Keratoneuritis
- Diagnosis and Management of Acanthamoeba Keratitis
- Stuies on biochemical characteristics and hemolysin purification of Aeromonas
- Production of extracellular enzymes and histamine release from rat peritoneal mast cells by aeromonas hydrophila
- Properties of aeromonas hydrophilia toxins