J Korean Med Assoc.
2019 Aug;62(8):407-415. 10.5124/jkma.2019.62.8.407.
Colorectal cancer epidemiology in Korea
- Affiliations
-
- 1Department of Preventive Medicine, College of Medicine, Seoul, Korea. shinaesun@snu.ac.kr
- 2Cancer Research Institute, Seoul National University, Seoul, Korea.
- 3Cancer Registration and Statistics Branch, National Cancer Center, Goyang, Korea.
- 4Department of Surgery, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2455377
- DOI: http://doi.org/10.5124/jkma.2019.62.8.407
Abstract
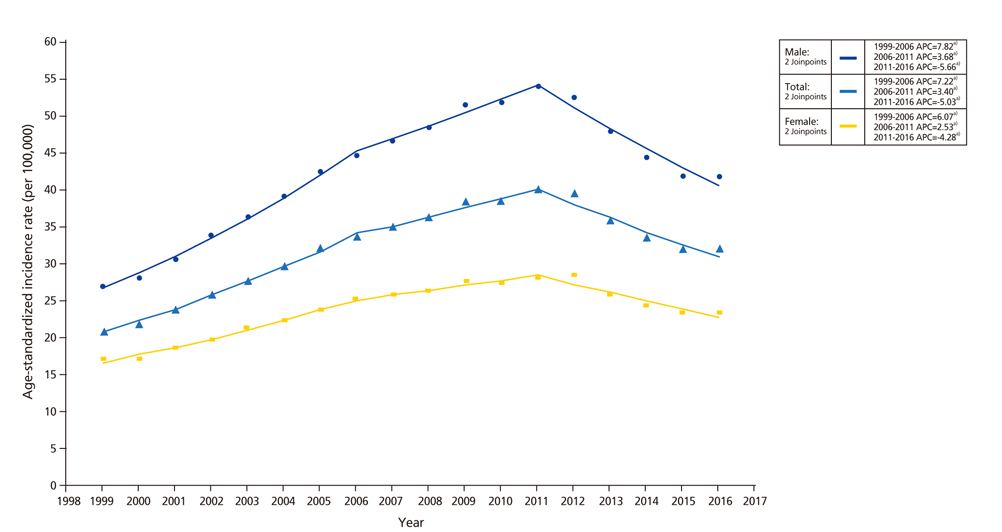
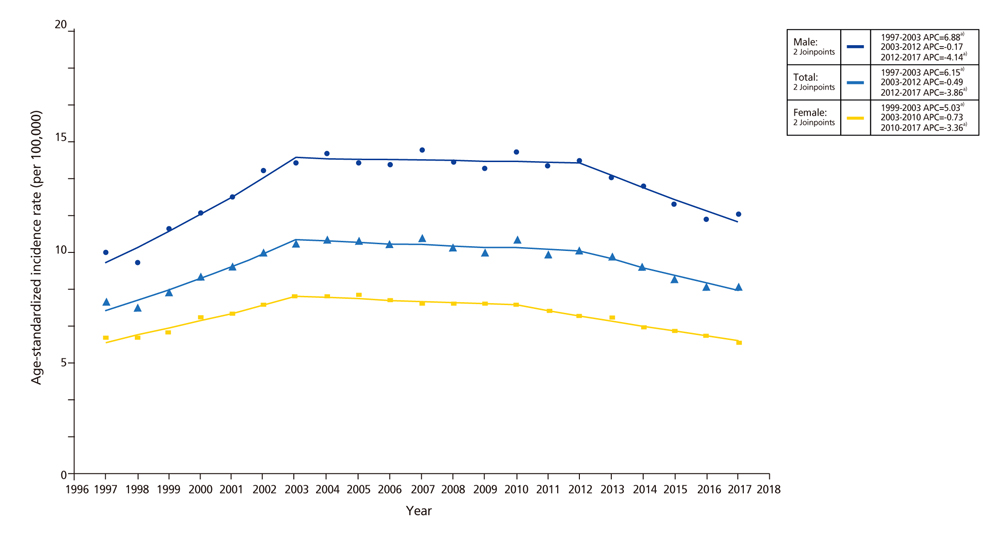
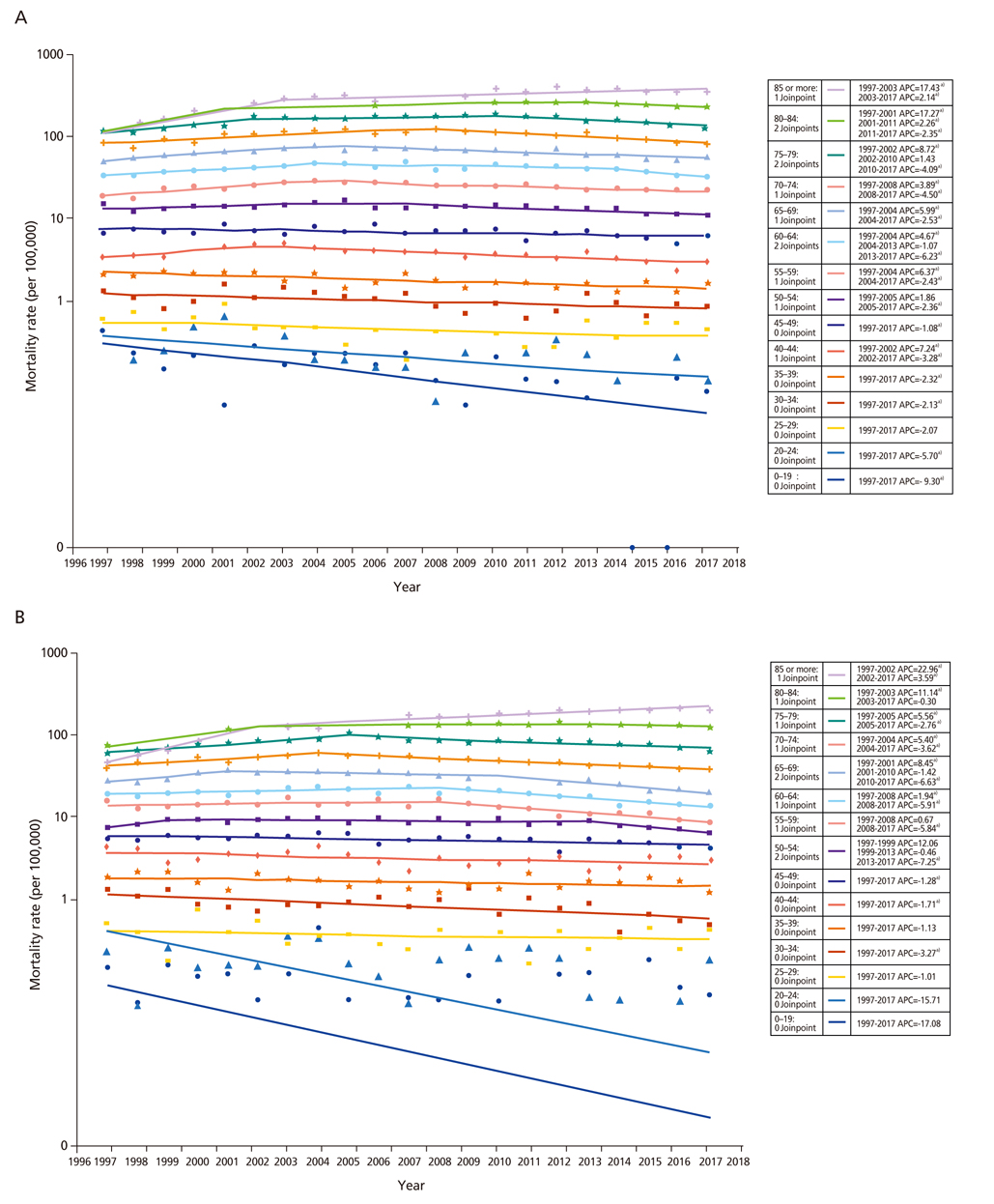
- Although colorectal cancer emerged as a major public health concern, its incidence as well as mortality are decreasing during recent years in Korea. Most important contributor for these reduction in disease burden is colorectal cancer screening. Besides screening, primary prevention through risk factor modification could reduce 10% to 54% of colorectal cancer incidence. These factors include limiting alcohol, processed and red meat consumption, and cigarette smoking, maintaining optimal weight, and engaging physical activities.
Keyword
MeSH Terms
Figure
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article2. World Cancer Research Fund International. Diet, nutrition, physical activity and cancer: a global perspective [Internet]. London: World Cancer Research Fund International;cited 2019 Jul 4. Available from: https://www.wcrf.org/dietandcancer.3. Jung KW, Won YJ, Kong HJ, Lee ES. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2016. Cancer Res Treat. 2019; 51:417–430.
Article4. The Lancet. GLOBOCAN 2018: counting the toll of cancer. Lancet. 2018; 392:985.5. Shin A, Kim KZ, Jung KW, Park S, Won YJ, Kim J, Kim DY, Oh JH. Increasing trend of colorectal cancer incidence in Korea, 1999–2009. Cancer Res Treat. 2012; 44:219–226.
Article6. Liang PS, Chen TY, Giovannucci E. Cigarette smoking and colorectal cancer incidence and mortality: systematic review and meta-analysis. Int J Cancer. 2009; 124:2406–2415.
Article7. Shin A, Jung KW, Woo H, Jeong SY. Colorectal cancer incidence in Korea is not the highest in the world. Cancer Res Treat. 2016; 48:864–867.
Article8. Young JP, Win AK, Rosty C, Flight I, Roder D, Young GP, et al. Rising incidence of early-onset colorectal cancer in Australia over two decades: report and review. J Gastroenterol Hepatol. 2015; 30:6–13.
Article9. Brenner DR, Ruan Y, Shaw E, De P, Heitman SJ, Hilsden RJ. Increasing colorectal cancer incidence trends among younger adults in Canada. Prev Med. 2017; 105:345–349.
Article10. Siegel RL, Fedewa SA, Anderson WF, Miller KD, Ma J, Rosenberg PS, Jemal A. Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst. 2017; 109:djw322.
Article11. International Agency for Research on Cancer. List of classifications by cancer sites with sufficient or limited evidence in humans, volumes 1 to 123 [Internet]. Lyon: International Agency for Research on Cancer;cited 2019 Jul 4. Available from: https://monographs.iarc.fr/wp-content/uploads/2018/07/Table4.pdf.12. Sung JJ, Chiu HM, Jung KW, Jun JK, Sekiguchi M, Matsuda T, Kyaw MH. Increasing trend in young-onset colorectal cancer in Asia: more cancers in men and more rectal cancers. Am J Gastroenterol. 2019; 114:322–329.
Article13. Woo HT, Sim JA, Mo J, Yun YH, Shin A. Regional differences in colorectal cancer mortality between 2000 and 2013 in Republic of Korea. J Epidemiol. 2018; 10. [Epub]. DOI: 10.2188/jea.JE20170331.
Article14. Korean Statistical Information Service. Statistics on cause of death [Internet]. Daejeon: Korean Statistical Information Service;cited 2019 Jul 4. Available from: http://kosis.kr/statisticsList/statisticsListIndex.do?menuId=M_01_01&vwcd=MT_ZTITLE&parmTabId=M_01_01&statId=1999038&themaId=D#SelectStatsBoxDiv.15. Shin A, Jung KW, Won YJ. Colorectal cancer mortality in Hong Kong of China, Japan, South Korea, and Singapore. World J Gastroenterol. 2013; 19:979–983.
Article16. National Cancer Center. Statistics on cancer registration 2016 [Internet]. Goyang: National Cancer Center;2019. cited 2019 Jul 4. Available from: http://ncc.re.kr/cancerStatsView.ncc?bbsnum=459&searchKey=total&searchValue=&pageNum=1.17. Abar L, Vieira AR, Aune D, Sobiecki JG, Vingeliene S, Polemiti E, Stevens C, Greenwood DC, Chan DS, Schlesinger S, Norat T. Height and body fatness and colorectal cancer risk: an update of the WCRF-AICR systematic review of published prospective studies. Eur J Nutr. 2018; 57:1701–1720.
Article18. Shin A, Joo J, Yang HR, Bak J, Park Y, Kim J, Oh JH, Nam BH. Risk predic-tion model for colorectal cancer: National Health Insurance Corporation study, Korea. PLoS One. 2014; 9:e88079.
Article19. Vieira AR, Abar L, Chan DS, Vingeliene S, Polemiti E, Stevens C, Greenwood D, Norat T. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Conti-nuous Update Project. Ann Oncol. 2017; 28:1788–1802.
Article20. Choi YJ, Myung SK, Lee JH. Light alcohol drinking and risk of cancer: a meta-analysis of cohort studies. Cancer Res Treat. 2018; 50:474–487.
Article21. McNabb S, Harrison TA, Albanes D, Berndt SI, Brenner H, Caan BJ, Campbell PT, Cao Y, Chang-Claude J, Chan A, Chen Z, English DR, Giles GG, Giovannucci EL, Goodman PJ, Hayes RB, Hoffmeister M, Jacobs EJ, Joshi AD, Larsson SC, Le Marchand L, Li L, Lin Y, Mannisto S, Milne RL, Nan H, Newton CC, Ogino S, Parfrey PS, Petersen PS, Potter JD, Schoen RE, Slattery ML, Su YR, Tangen CM, Tucker TC, Weinstein SJ, White E, Wolk A, Woods MO, Phipps AI, Peters U. Meta-analysis of 16 studies of the association of alcohol with colorectal cancer. Int J Cancer. 2019; 04. 29. [Epub]. DOI: 10.1002/ijc.32377.
Article22. Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008; 300:2765–2778.23. Jass JR. Classification of colorectal cancer based on correla-tion of clinical, morphological and molecular features. Histo-pathology. 2007; 50:113–130.
Article24. Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, Guha N, Mattock H, Straif K. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015; 16:1599–1600.
Article25. National Cancer Center. Importance of cancer prevention [Internet]. Goyang: National Cancer Center;cited 2019 Jul 4. Available from: http://ncc.re.kr/main.ncc?uri=manage01_3.26. Parkin DM, Boyd L, Walker LC. 16. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011; 105 Suppl 2:S77–S81.
Article27. Park S, Shin HR, Lee B, Shin A, Jung KW, Lee DH, Jee SH, Cho SI, Park SK, Boniol M, Boffetta P, Weiderpass E. Attributable fraction of alcohol consumption on cancer using population-based nationwide cancer incidence and mortality data in the Republic of Korea. BMC Cancer. 2014; 14:420.
Article28. Park S, Jee SH, Shin HR, Park EH, Shin A, Jung KW, Hwang SS, Cha ES, Yun YH, Park SK, Boniol M, Boffetta P. Attributable fraction of tobacco smoking on cancer using population-based nationwide cancer incidence and mortality data in Korea. BMC Cancer. 2014; 14:406.
Article29. Park S, Kim Y, Shin HR, Lee B, Shin A, Jung KW, Jee SH, Kim DH, Yun YH, Park SK, Boniol M, Boffetta P. Population-attributable causes of cancer in Korea: obesity and physical inactivity. PLoS One. 2014; 9:e90871.
Article30. Suh M, Song S, Cho HN, Park B, Jun JK, Choi E, Kim Y, Choi KS. Trends in participation rates for the National Cancer Screening Program in Korea, 2002–2012. Cancer Res Treat. 2017; 49:798–806.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gender-specific Colorectal Cancer: Epidemiologic Difference and Role of Estrogen
- Incidence pattern of colorectal cancer in Korea by subsite of origin
- Endoscopic diagnosis and treatment of early colorectal cancer
- Reply on "Data on the Characteristics and the Survival of Korean Patients With Colorectal Cancer From the Korea Central Cancer Registry"
- Screening strategy for colorectal cancer according to risk