Obstet Gynecol Sci.
2019 Jul;62(4):264-272. 10.5468/ogs.2019.62.4.264.
Investigation of human papillomavirus prevalence in married women and molecular characterization and phylogenetic analysis of the virus
- Affiliations
-
- 1Department of Medical Microbiology, School of Medicine, Atatürk University, Erzurum, Turkey. osaktas@atauni.edu.tr
- 2Department of Gynecology and Obstetrics, Health Sciences University, Erzurum Regional Training and Research Hospital, Erzurum, Turkey.
- 3Department of Birth, Women's Health and Diseases Nursing, Faculty of Nursing, Atatürk University, Erzurum, Turkey.
- KMID: 2451656
- DOI: http://doi.org/10.5468/ogs.2019.62.4.264
Abstract
OBJECTIVE
Human papillomaviruses (HPVs) are among the agents responsible for infection and cancer of the skin and mucous membranes in the human body. The aim of this study was to investigate the frequency and type distribution of HPVs in married female patients with gynecological complaints, who had visited the Maternity Hospital in Erzurum, Turkey.
METHODS
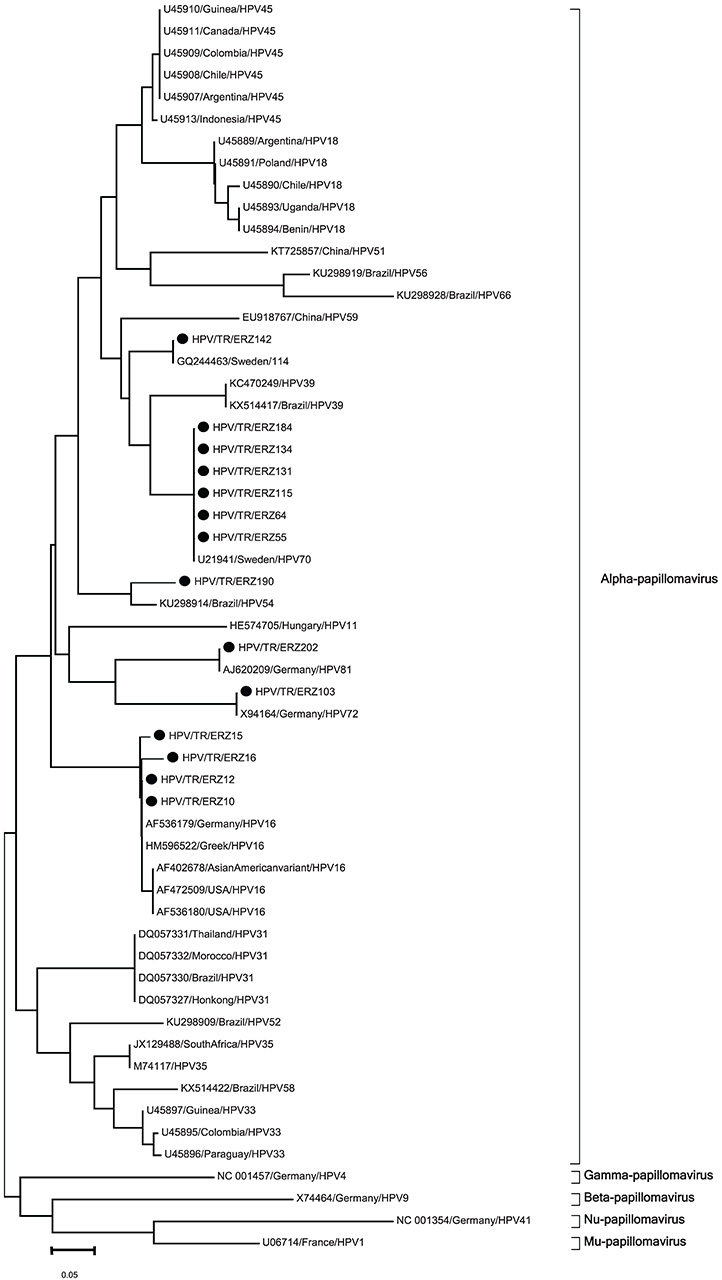
In this study, 263 cervical swab samples were taken from married women using the Pap smear method and were investigated for positive reactivity against HPV. The L1 gene region of HPV was investigated using molecular methods. For this purpose, polymerase chain reaction (PCR) assays and sequence analysis of positive samples were performed. Phylogenetic analyses were performed using a bioinformatics approach after sequencing.
RESULTS
HPV-DNA was detected in 17 (6.5%) samples. Highest positive reactivity to HPV-DNA was found in the 35-44 age group at 9.2%. Fourteen out of seventeen positive samples were included in the phylogenetic analysis. All isolates clustered in the Alphapapillomavirus genus. Six samples were found to be HPV 70 positive, four were HPV 16 positive, and the rest were HPV 54, 72, 81, and 114 positive. When genotyping data were evaluated according to the risk group, we found that 28.6% of the 14 samples were found to be high risk-HPV, and 71.4% were low risk-HPV.
CONCLUSIONS
As per our knowledge, this is the first report on the phylogenetic analysis of HPV genotypes isolated from women in Turkey. The prevalence of low- and-high risk HPV was determined in married women in Erzurum, and these results contribute to the epidemiological data on the distribution of HPV types for this region.
MeSH Terms
Figure
Reference
-
1. Abramowitz L, Lacau Saint Guily J, Moyal-Barracco M, Bergeron C, Borne H, Dahlab A, et al. Epidemiological and economic burden of potentially HPV-related cancers in France. PLoS One. 2018; 13:e0202564.
Article2. Chow LT, Broker TR, Steinberg BM. The natural history of human papillomavirus infections of the mucosal epithelia. APMIS. 2010; 118:422–449.
Article3. Thun MJ, DeLancey JO, Center MM, Jemal A, Ward EM. The global burden of cancer: priorities for prevention. Carcinogenesis. 2010; 31:100–110.
Article4. Ceccarelli M, Rullo EV, Facciolà A, Madeddu G, Cacopardo B, Taibi R, et al. Head and neck squamous cell carcinoma and its correlation with human papillomavirus in people living with HIV: a systematic review. Oncotarget. 2018; 9:17171–17180.
Article5. Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007; 370:890–907.
Article6. Rompalo A. Preventing sexually transmitted infections: back to basics. J Clin Invest. 2011; 121:4580–4583.
Article7. Sahasrabuddhe VV, Parham GP, Mwanahamuntu MH, Vermund SH. Cervical cancer prevention in low- and middle-income countries: feasible, affordable, essential. Cancer Prev Res (Phila). 2012; 5:11–17.
Article8. Republic of Turkey Ministry of Health. Health Statistics Yearbook 2016 [Internet]. Ankara (TR): General Directorate of Health Research;c2018. cited 2018 Oct 21. Available from: https://dosyasb.saglik.gov.tr/Eklenti/13160,sy2016enpdf.pdf?0.9. Tulan D, Türko ES. Women entrepreneurship: a survey in Erzurum province. Finans Ekon Sos Araşt Derg. 2018; 3:285–306.10. Entiauspe L, Nunes E, Collares T, da Silveira MF, Seixas F. Comparison between two methods for molecular characterization of human papillomavirus. J Bras Doenças Sex Transm. 2013; 25:13–15.
Article11. Ozgul N. Genital warts. Turkiye Klinikleri J Gynecol Obstet Spec Top. 2017; 10:174–180.12. Bruni L, Diaz M, Castellsagué X, Ferrer E, Bosch FX, de Sanjosé S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010; 202:1789–1799.
Article13. Phoolcharoen N, Kantathavorn N, Sricharunrat T, Saeloo S, Krongthong W. A population-based study of cervical cytology findings and human papillomavirus infection in a suburban area of Thailand. Gynecol Oncol Rep. 2017; 21:73–77.
Article14. Martins TR, Mendes de Oliveira C, Rosa LR, de Campos Centrone C, Rodrigues CL, Villa LL, et al. HPV genotype distribution in Brazilian women with and without cervical lesions: correlation to cytological data. Virol J. 2016; 13:138.
Article15. Dursun P, Ayhan A, Mutlu L, Çağlar M, Haberal A, Güngör T, et al. HPV types in Turkey: multicenter hospital based evaluation of 6388 patients in Turkish gynecologic oncology group centers. Turk Patoloji Derg. 2013; 29:210–216.
Article16. Coscia MF, Monno R, Ballini A, Mirgaldi R, Dipalma G, Pettini F, et al. Human papilloma virus (HPV) genotypes prevalence in a region of South Italy (Apulia). Ann Ist Super Sanita. 2015; 51:248–251.17. Kim MJ, Kim JJ, Kim S. Type-specific prevalence of high-risk human papillomavirus by cervical cytology and age: data from the health check-ups of 7,014 Korean women. Obstet Gynecol Sci. 2013; 56:110–120.
Article18. Ouh YT, Min KJ, Cho HW, Ki M, Oh JK, Shin SY, et al. Prevalence of human papillomavirus genotypes and precancerous cervical lesions in a screening population in the Republic of Korea, 2014–2016. J Gynecol Oncol. 2018; 29:e14.
Article19. Bansal D, Elmi AA, Skariah S, Haddad P, Abu-Raddad LJ, Al Hamadi AH, et al. Molecular epidemiology and genotype distribution of Human Papillomavirus (HPV) among Arab women in the State of Qatar. J Transl Med. 2014; 12:300.
Article20. Altun Z, Yarkin F, Vardar MA, Uguz AH. The prevalence of human papilloma virus infection among women who admitted to Cukurova University Faculty of Medicine Hospital. Turkiye Klinikleri J Med Sci. 2011; 31:307–314.21. Findik D, Dagi HT, Arslan U, Findik Y. Frequency and genotype distribution of human papillomavirus in cervical specimens. Genel Tıp Derg. 2012; 22:116–120.22. Avci GA, Bozdayi G, Taskiran Ç, Ozkan S, Onan MA. Phylogenetic analysis and prevalence of human papillomavirus (HPV) in women with cervical pathologies. J Turk Soc Obstet Gynecol. 2013; 10:151–159.23. Unal B, Sezer C. Analysis of high risk HPV subtypes associated with cervical intraepithelial neoplasia: a single centre retrospective study in the Mediterranean region of Turkey. Turk Patoloji Derg. 2014; 30:85–86.
Article24. Bulut Y, Belhan M, Özercan İH. Detection of human papillomavirus genotypes by pyrosequencing method in uterine cervical cancer samples. Firat Univ Med J Health Sci. 2016; 30:71–75.25. Barışık NO, Keser SH, Gül AE, Şimşek EE, Özdemir HG. Prevalence of high-risk human papilloma virus and identification of type using real-time polymerase chain reaction analysis and liquid-based cytology. South Clin Istanb Eurasia. 2017; 28:175–180.26. Giuliodori K, Campanati A, Liberati G, Ganzetti G, Giangiacomi M, Marinelli K, et al. Lifelong widespread warts associated with human papillomavirus type 70/85: a new diagnostic entity? Acta Dermatovenerol Alp Panonica Adriat. 2016; 25:11–13.
Article27. Potocnik M, Kocjan B, Seme K, Poljak M. Distribution of human papillomavirus (HPV) genotypes in genital warts from males in Slovenia. Acta Dermatovenerol Alp Panonica Adriat. 2007; 16:91–96.28. Vergori A, Garbuglia AR, Piselli P, Del Nonno F, Sias C, Lupi F, et al. Oral human papillomavirus DNA detection in HIV-positive men: prevalence, predictors, and co-occurrence at anal site. BMC Infect Dis. 2018; 18:25.
Article29. Ekström J, Forslund O, Dillner J. Three novel papillomaviruses (HPV109, HPV112 and HPV114) and their presence in cutaneous and mucosal samples. Virology. 2010; 397:331–336.
Article30. Aziz H, Iqbal H, Mahmood H, Fatima S, Faheem M, Sattar AA, et al. Human papillomavirus infection in females with normal cervical cytology: genotyping and phylogenetic analysis among women in Punjab, Pakistan. Int J Infect Dis. 2018; 66:83–89.
Article31. Chen Z, Schiffman M, Herrero R, DeSalle R, Anastos K, Segondy M, et al. Classification and evolution of human papillomavirus genome variants: alpha-5 (HPV26, 51, 69, 82), alpha-6 (HPV30, 53, 56, 66), alpha-11 (HPV34, 73), alpha-13 (HPV54) and alpha-3 (HPV61). Virology. 2018; 516:86–101.
Article32. Cui F, Zhang Z, Xu J, Ding X, Mu X, Wan Q, et al. Genetic variability and lineage phylogeny of human papillomavirus type 45 based on E6 and E7 genes in Southwest China. Virus Res. 2018; 255:85–89.
Article33. Conde-Ferraez L, Pacheco-Arjona R, Novelo Canul C, Gomez-Carballo J, Ramirez-Prado JH, Ayora-Talavera G, et al. Genetic variability in E6 and E7 oncogenes from human papillomavirus type 58 in Mexican women. Intervirology. 2017; 60:235–246.
Article34. Ramas V, Mirazo S, Bonilla S, Ruchansky D, Arbiza J. Analysis of human papillomavirus 16 E6, E7 genes and Long Control Region in cervical samples from Uruguayan women. Gene. 2018; 654:103–109.
Article35. Zhang J, Zhang S, Wang M, Ding X, Wen Q, Chen Z, et al. Genetic variability in E5, E6, E7 and L1 genes of human papillomavirus type 31. Mol Med Rep. 2018; 17:5498–5507.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of Human Papilloma Virus Infection in Perimenopausal Women in Bucheon Province
- Detection and typing of human papillomavirus DNA by PCR using consensus primers in various cervical lesions of Korean women
- Molecular characteristics of Budgerigar fledgling disease polyomavirus detected from parrots in South Korea
- Molecular characterization and phylogenetic analysis of pseudorabies virus variants isolated from Guangdong province of southern China during 2013–2014
- Why Should You Care About Oral Gonorrhea and Oral Human Papillomavirus Infection?