Hip Pelvis.
2019 Mar;31(1):33-39. 10.5371/hp.2019.31.1.33.
Comparison of the Incidence of Intra-operative Fractures in Hip Hemi-arthroplasty Performed in Supine and Lateral Positions
- Affiliations
-
- 1Department of Orthopedic Surgery, Yamaguchi Red Cross Hospital, Yamaguchi, Japan. kamoknts@gaea.ocn.ne.jp
- KMID: 2448039
- DOI: http://doi.org/10.5371/hp.2019.31.1.33
Abstract
- PURPOSE
The difficulty of femoral preparation with supine-position hip hemi-arthroplasty (HA) often leads to intra-operative fractures (IOFs). We aimed to clarify the incidence and types of IOFs in HA for hip fractures performed in the supine and lateral positions.
MATERIALS AND METHODS
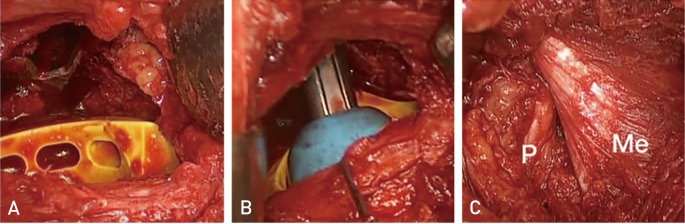
We retrospectively investigated cases of HA for acute femoral neck fractures from June 2013 to May 2018. We examined the incidence and types of IOFs according to different approaches. We defined supine-position in HA as the supine and hip-hyperextended (over-range) femoral preparation position, and lateral position as the lateral and hip-flexed femoral preparation position. We used a short tapered wedged stem.
RESULTS
Supine-position HA was used in 46 patients (23.7%) and lateral-position HA in 148 patients (76.3%). IOFs in supine-position HA occurred in 8 patients (17.4%) and included five Vancouver AGT and three Vancouver B2 fractures. IOFs in lateral-position HA occurred in 3 patients (2.0%) and included one Vancouver AGT and two Vancouver B fractures. Supine-position HA was a risk factor for IOFs (adjusted odds ratio, 9.71; 95% confidence interval, 2.37-39.8; P < 0.01)
CONCLUSION
Supine-position in HA is an IOF risk factor and significantly increases the incidence of great trochanter fractures of Vancouver type A.
Keyword
MeSH Terms
Figure
Reference
-
1. Aslam-Pervez N, Riaz O, Gopal S, Hossain F. Predictors of intraoperative fractures during hemiarthroplasty for the treatment of fragility hip fractures. Clin Orthop Surg. 2018; 10:14–19. PMID: 29564042.
Article2. Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995; 44:293–304. PMID: 7797866.3. Davidson D, Pike J, Garbuz D, Duncan CP, Masri BA. Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J Bone Joint Surg Am. 2008; 90:2000–2012. PMID: 18762663.4. Cooper HJ, Rodriguez JA. Early post-operative periprosthetic femur fracture in the presence of a non-cemented tapered wedge femoral stem. HSS J. 2010; 6:150–154. PMID: 21886528.
Article5. Miettinen SS, Mäkinen TJ, Kostensalo I, et al. Risk factors for intraoperative calcar fracture in cementless total hip arthroplasty. Acta Orthop. 2016; 87:113–119. PMID: 26541230.
Article6. van der Sijp MPL, van Delft D, Krijnen P, Niggebrugge AHP, Schipper IB. Surgical approaches and hemiarthroplasty outcomes for femoral neck fractures: a meta-analysis. J Arthroplasty. 2018; 33:1617–1627.e9. PMID: 29398259.
Article7. van den Bekerom MP, Sierevelt IN, Bonke H, Raaymakers EL. The natural history of the hemiarthroplasty for displaced intracapsular femoral neck fractures. Acta Orthop. 2013; 84:555–560. PMID: 24286565.8. Schneider K, Audigé L, Kuehnel SP, Helmy N. The direct anterior approach in hemiarthroplasty for displaced femoral neck fractures. Int Orthop. 2012; 36:1773–1781. PMID: 22527335.
Article9. Baba T, Shitoto K, Kaneko K. Bipolar hemiarthroplasty for femoral neck fracture using the direct anterior approach. World J Orthop. 2013; 4:85–89. PMID: 23610757.
Article10. Unger AC, Dirksen B, Renken FG, Wilde E, Willkomm M, Schulz AP. Treatment of femoral neck fracture with a minimal invasive surgical approach for hemiarthroplasty - clinical and radiological results in 180 geriatric patients. Open Orthop J. 2014; 8:225–231. PMID: 25136389.
Article11. Kamo K, Kido H, Kido S, et al. [The concept of the superior approach for hip arthroplasty]. Jpn J Joint Dis. 2017; 36:457–460. Japanese.12. Higuchi F, Gotoh M, Yamaguchi N, et al. Minimally invasive uncemented total hip arthroplasty through an anterolateral approach with a shorter skin incision. J Orthop Sci. 2003; 8:812–817. PMID: 14648270.
Article13. Moore AT. The self-locking metal hip prosthesis. J Bone Joint Surg Am. 1957; 39-A:811–827. PMID: 13438939.
Article14. Nakamura S, Matsuda K, Arai N, Wakimoto N, Matsushita T. Mini-incision posterior approach for total hip arthroplasty. Int Orthop. 2004; 28:214–217. PMID: 15168084.
Article15. Murphy SB, Ecker TM, Tannast M. THA performed using conventional and navigated tissue-preserving techniques. Clin Orthop Relat Res. 2006; 453:160–167. PMID: 17312591.
Article16. Tsukada S, Wakui M. Minimally invasive intermuscular approach does not improve outcomes in bipolar hemiarthroplasty for femoral neck fracture. J Orthop Sci. 2010; 15:753–757. PMID: 21116892.
Article17. Pala E, Trono M, Bitonti A, Lucidi G. Hip hemiarthroplasty for femur neck fractures: minimally invasive direct anterior approach versus postero-lateral approach. Eur J Orthop Surg Traumatol. 2016; 26:423–427. PMID: 27026091.
Article18. Bodrogi AW, Sciortino R, Fitch DA, Gofton W. Use of the supercapsular percutaneously assisted total hip approach for femoral neck fractures: surgical technique and case series. J Orthop Surg Res. 2016; 11:113. PMID: 27733183.
Article19. Chana R, Mansouri R, Jack C, et al. The suitability of an uncemented hydroxyapatite coated (HAC) hip hemiarthroplasty stem for intra-capsular femoral neck fractures in osteoporotic elderly patients: the Metaphyseal-Diaphyseal Index, a solution to preventing intra-operative periprosthetic fracture. J Orthop Surg Res. 2011; 6:59. PMID: 22099169.
Article20. Bertin KC, Röttinger H. Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res. 2004; (429):248–255. PMID: 15577495.21. Pflüger G, Junk-Jantsch S, Schöll V. Minimally invasive total hip replacement via the anterolateral approach in the supine position. Int Orthop. 2007; 31(Suppl 1):S7–S11. PMID: 17668206.
Article22. Smith-Petersen MN. Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am. 1949; 31A:40–46. PMID: 18122877.
Article23. Siguier T, Siguier M, Brumpt B. Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop Relat Res. 2004; (426):164–173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Total Hip Replacement for Displaced Femoral Neck Fracture in Old Age Group
- Usefulness of a Modular Hip System for Combined Anteversion in Cementless Total Hip Arthroplasty
- Lateral Insufficiency Fracture of the Femur caused by Osteopenia & Varus angulation after Hip Arthroplasty: Case Report
- Modified Posterior Approach to Total Hip Arthroplasty
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty