Hip Pelvis.
2019 Mar;31(1):18-22. 10.5371/hp.2019.31.1.18.
Outcomes of Magnetic Resonance Imaging Detected Occult Neck of Femur Fractures: Do They Represent a Less Severe Injury with Improved Outcomes?
- Affiliations
-
- 1Department of Orthopaedic and Trauma Surgery, Ninewells Hospital and Medical School, University of Dundee, Dundee, Scotland, UK. raval.prashant@gmail.com
- 2Tayside Orthopaedic Rehabilitation Technology (TORT) Centre, Ninewells Hospital and Medical School, University of Dundee, Dundee, Scotland, UK.
- 3Department of Clinical Radiology, Ninewells Hospital and Medical School, Dundee, Scotland, UK.
- KMID: 2448037
- DOI: http://doi.org/10.5371/hp.2019.31.1.18
Abstract
- PURPOSE
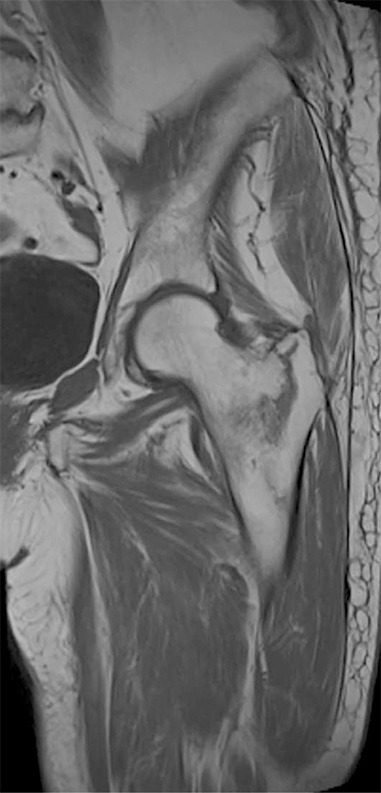
Occult hip fractures in the elderly can be missed on standard radiographs and are a known cause of morbidity. These are generally diagnosed on either magnetic resonance imaging (MRI) or computed tomography scan, depending upon local hospital policy. While there is an abundance of literature on hip fractures in general, little is known about the clinical outcome of patients with occult hip fractures. The aim of this study was to review the demographics, injury characteristics, management and clinical outcome of patients diagnosed with occult femoral neck fractures on MRI.
MATERIALS AND METHODS
Using an existing hospital database, a retrospective analysis of all patients with occult hip fractures diagnosed by MRI scan from 2005 to 2014 was conducted.
RESULTS
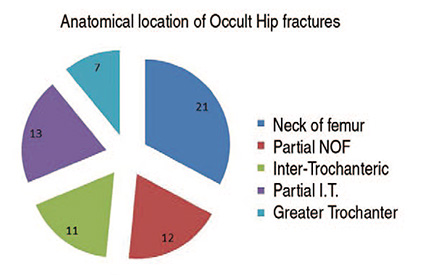
Sixty-four patients (23 males and 41 females) were included. The mean duration of hospitalisation was 16 days. A significantly higher percentage of patients were discharged to their pre-existing residence compared to National Institute for Health and Care Excellence (NICE) commissioning guidelines (66% vs. 45%). The 30- and 60-day mortalities were 3% and 10%, respectively. Mortality was lower in patients who underwent internal fixation (n=3/31) compared with those undergoing replacement (hemi/total hip arthroplasty) (n=5/12) (P=0.056).
CONCLUSION
Patients with occult hip fractures diagnosed on an MRI scan are more likely to be discharged to their pre-existing residence and have lower mortality rates compared to NICE guidelines and National Hip Fracture Database (NHFD).
Keyword
MeSH Terms
Figure
Reference
-
1. British Orthopaedic Association. The care of patients with fragility fracture. London: British Orthopaedic Association;2007.2. National Clinical Guideline Centre. NICE Clinical Guidelines, No. 124. The management of hip fracture in adults. London: Royal College of Physicians (UK);2011.3. Alam A, Willett K, Ostlere S. The MRI diagnosis and management of incomplete intertrochanteric fractures of the femur. J Bone Joint Surg Br. 2005; 87:1253–1255.
Article4. Chana R, Noorani A, Ashwood N, Chatterji U, Healy J, Baird P. The role of MRI in the diagnosis of proximal femoral fractures in the elderly. Injury. 2006; 37:185–189.
Article5. Pihlajama¨ki HK, Ruohola JP, Weckstro¨m M, Kiuru MJ, Visuri TI. Long-term outcome of undisplaced fatigue fractures of the femoral neck in young male adults. J Bone Joint Surg Br. 2006; 88:1574–1579.6. Iwata T, Nozawa S, Dohjima T, et al. The value of T1-weighted coronal MRI scans in diagnosing occult fracture of the hip. J Bone Joint Surg Br. 2012; 94:969–973.
Article7. Lubovsky O, Liebergall M, Mattan Y, Weil Y, Mosheiff R. Early diagnosis of occult hip fractures MRI versus CT scan. Injury. 2005; 36:788–792.8. Hossain M, Barwick C, Sinha AK, Andrew JG. Is magnetic resonance imaging (MRI) necessary to exclude occult hip fracture? Injury. 2007; 38:1204–1208.
Article9. Hakkarinen DK, Banh KV, Hendey GW. Magnetic resonance imaging identifies occult hip fractures missed by 64-slice computed tomography. J Emerg Med. 2012; 43:303–307.
Article10. Royal College of Physicians. National Hip Fracture Database (NHFD) annual report 2017. London: Royal College of Physicians;2017.11. Todd CJ, Freeman CJ, Camilleri-Ferrante C, et al. Differences in mortality after fracture of hip: the east Anglian audit. BMJ. 1995; 310:904–908.
Article12. Hapuarachchi KS, Ahluwalia RS, Bowditch MG. Neck of femur fractures in the over 90s: a select group of patients who require prompt surgical intervention for optimal results. J Orthop Traumatol. 2014; 15:13–19.
Article13. National Institute for Health and Clinical Excellence (NICE). NICE Guidance CMG 46. The management of hip fractures in adults. London: NICE;2012.14. Kim SJ, Ahn J, Kim HK, Kim JH. Is magnetic resonance imaging necessary in isolated greater trochanter fracture? A systemic review and pooled analysis. BMC Musculoskelet Disord. 2015; 16:395.
Article15. Beloosesky Y, Hershkovitz A, Guz A, Golan H, Salai M, Weiss A. Clinical characteristics and long-term mortality of occult hip fracture elderly patients. Injury. 2010; 41:343–347.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Occult Intertrochanteric Fracture Mimicking the Fracture of Greater Trochanter
- The Frequency of Occult Intertrochanteric Fractures among Individuals with Isolated Greater Trochanteric Fractures
- Occult Fractures of the Subtalar Joint
- The Diagnosis of Osteoporotic Occult Vertebral Fracture and Vertebroplasty
- Internal Fixation of Pauwels Type-3 Undisplacedincomplete Insufficiency Femoral Neck Fractures with Cephalomedullary Nails