Clin Endosc.
2019 Mar;52(2):120-128. 10.5946/ce.2019.047.
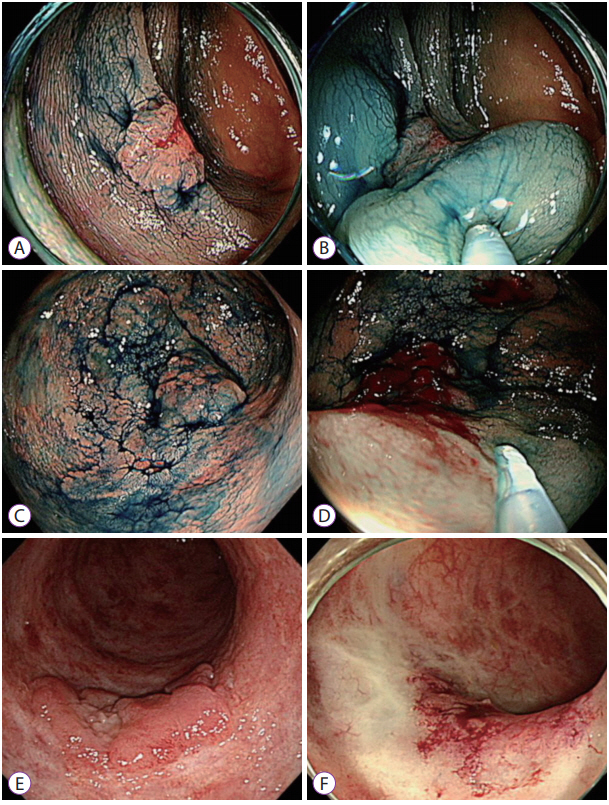
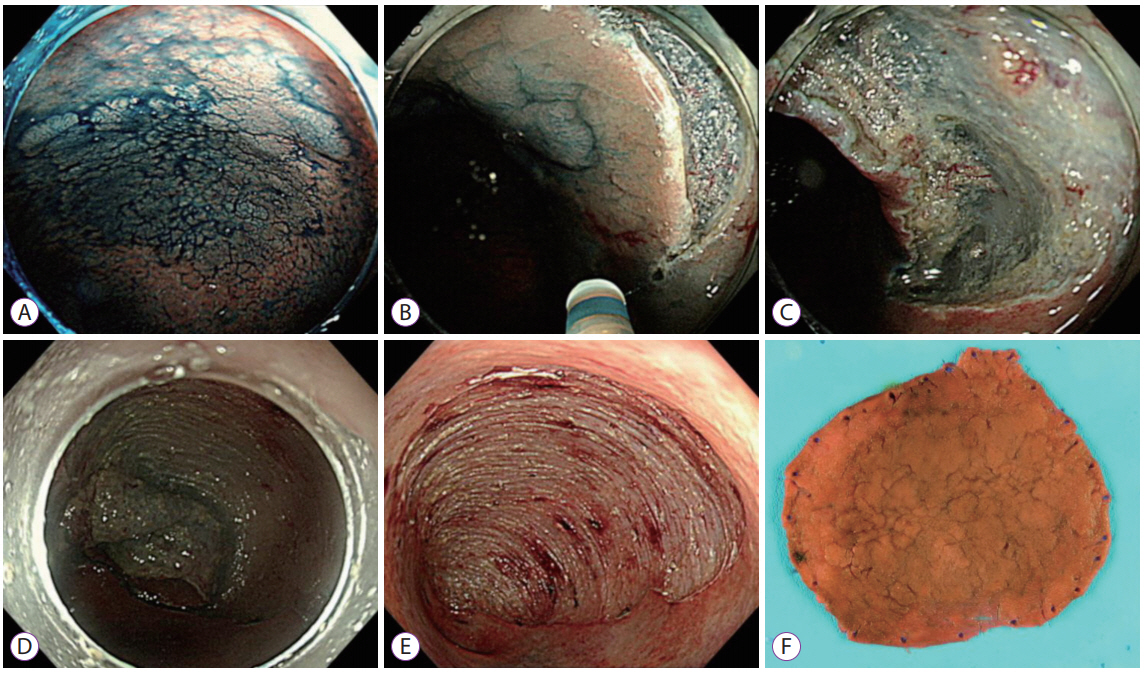
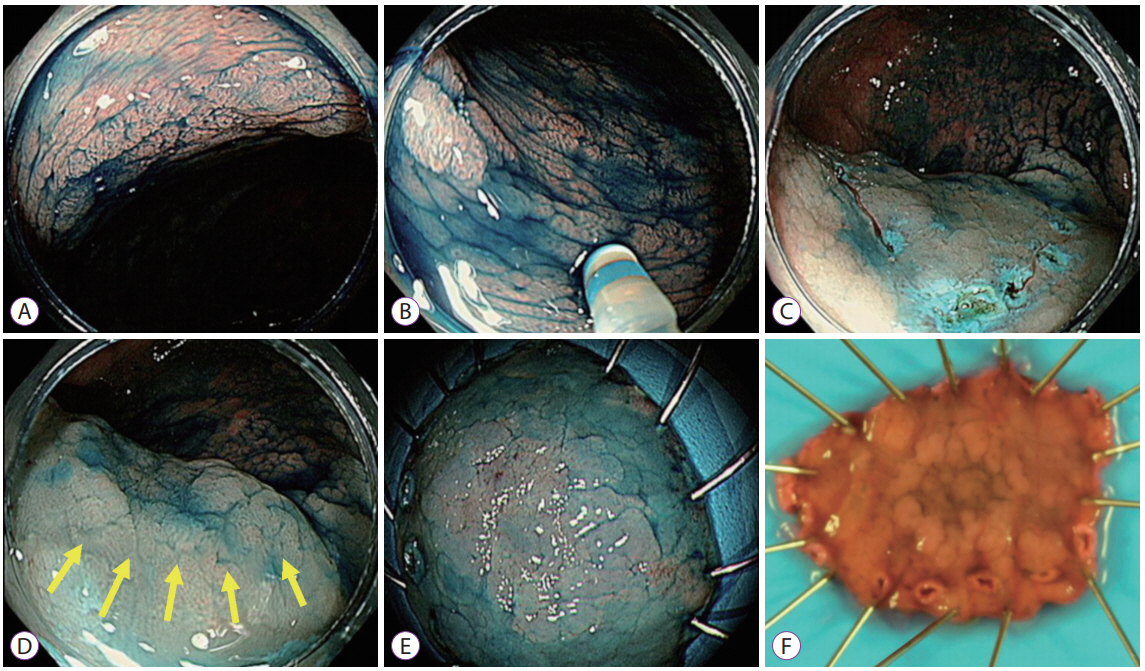
Endoscopic Submucosal Dissection for Colitis-Associated Dysplasia
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dhyang@amc.seoul.kr
- 2Division of Gastroenterohepatology, Department of Internal Medicine, University of Sumatera Utara, Adam Malik General Hospital, Medan, Indonesia.
- KMID: 2447668
- DOI: http://doi.org/10.5946/ce.2019.047
Abstract
- Dysplasia is a precancerous lesion of colorectal cancer in patients with long-standing inflammatory bowel diseases (IBDs), such as ulcerative colitis and Crohn's disease. Recent guidelines suggest endoscopic resection as a key modality for the treatment of endoscopically resectable dysplasia in patients with colitis. Endoscopic submucosal dissection (ESD) has been suggested as one of the therapeutic options for dysplasia that is potentially resectable but not suitable for the conventional endoscopic mucosal resection technique. Several recent studies supported the feasibility of ESD for the treatment of colitis-associated dysplasia in terms of the en bloc and complete resection rates and the risk of procedure-related complications. However, these studies were performed exclusively in expert centers. Moreover, the local and metachronous recurrence rates were relatively high, and long-term outcome data are still lacking. Endoscopists should be highly skilled in colorectal ESD and have an intensive understanding of not only the lesions but also the conditions of patients with IBDs. Therefore, the decision to perform ESD for colitis-associated dysplasia should be made scrupulously after careful discussion with patients, in collaboration with a multidisciplinary IBD team including physicians, surgeons, and pathologists specialized in IBDs.
MeSH Terms
Figure
Cited by 1 articles
-
Endoscopic molecular imaging in inflammatory bowel disease
Nam Seok Ham, Seung-Jae Myung
Intest Res. 2021;19(1):33-44. doi: 10.5217/ir.2019.09175.
Reference
-
1. Jess T, Rungoe C, Peyrin-Biroulet L. Risk of colorectal cancer in patients with ulcerative colitis: a meta-analysis of population-based cohort studies. Clin Gastroenterol Hepatol. 2012; 10:639–645.
Article2. Colman RJ, Rubin DT. Histological inflammation increases the risk of colorectal neoplasia in ulcerative colitis: a systematic review. Intest Res. 2016; 14:202–210.
Article3. Zhiqin W, Palaniappan S, Raja Ali RA. Inflammatory bowel disease-related colorectal cancer in the Asia-Pacific region: past, present, and future. Intest Res. 2014; 12:194–204.
Article4. Velayos F, Kathpalia P, Finlayson E. Changing paradigms in detection of dysplasia and management of patients with inflammatory bowel disease: is colectomy still necessary? Gastroenterology. 2017; 152:440–450.e1.5. Rubin PH, Friedman S, Harpaz N, et al. Colonoscopic polypectomy in chronic colitis: conservative management after endoscopic resection of dysplastic polyps. Gastroenterology. 1999; 117:1295–1300.
Article6. Engelsgjerd M, Farraye FA, Odze RD. Polypectomy may be adequate treatment for adenoma-like dysplastic lesions in chronic ulcerative colitis. Gastroenterology. 1999; 117:1288–1294. discussion 1488-1491.
Article7. Wanders LK, Dekker E, Pullens B, Bassett P, Travis SP, East JE. Cancer risk after resection of polypoid dysplasia in patients with longstanding ulcerative colitis: a meta-analysis. Clin Gastroenterol Hepatol. 2014; 12:756–764.
Article8. Mooiweer E, van der Meulen-de Jong AE, Ponsioen CY, et al. Incidence of interval colorectal cancer among inflammatory bowel disease patients undergoing regular colonoscopic surveillance. Clin Gastroenterol Hepatol. 2015; 13:1656–1661.
Article9. Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7:982–1018.
Article10. Laine L, Kaltenbach T, Barkun A, McQuaid KR, Subramanian V, Soetikno R. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015; 148:639–651.e28.
Article11. American Society for Gastrointestinal Endoscopy Standards of Practice Committee, Shergill AK, Lightdale JR, et al. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015; 81:1101–1121. e1-e13.
Article12. Soetikno R, Subramanian V, Kaltenbach T, et al. The detection of nonpolypoid (flat and depressed) colorectal neoplasms in patients with inflammatory bowel disease. Gastroenterology. 2013; 144:1349–1352. 1352.e1-e6.
Article13. Blackstone MO, Riddell RH, Rogers BH, Levin B. Dysplasia-associated lesion or mass (DALM) detected by colonoscopy in long-standing ulcerative colitis: an indication for colectomy. Gastroenterology. 1981; 80:366–374.
Article14. Itzkowitz SH, Harpaz N. Diagnosis and management of dysplasia in patients with inflammatory bowel diseases. Gastroenterology. 2004; 126:1634–1648.
Article15. Lee SH, Shin SJ, Park DI, et al. Korean guideline for colonoscopic polypectomy. Clin Endosc. 2012; 45:11–24.
Article16. Kudo S, Rubio CA, Teixeira CR, Kashida H, Kogure E. Pit pattern in colorectal neoplasia: endoscopic magnifying view. Endoscopy. 2001; 33:367–373.
Article17. Kudo S, Lambert R, Allen JI, et al. Nonpolypoid neoplastic lesions of the colorectal mucosa. Gastrointest Endosc. 2008; 68(4 Suppl):S3–S47.
Article18. Ikematsu H, Matsuda T, Emura F, et al. Efficacy of capillary pattern type IIIA/IIIB by magnifying narrow band imaging for estimating depth of invasion of early colorectal neoplasms. BMC Gastroenterol. 2010; 10:33.
Article19. Sumimoto K, Tanaka S, Shigita K, et al. Diagnostic performance of Japan NBI Expert Team classification for differentiation among noninvasive, superficially invasive, and deeply invasive colorectal neoplasia. Gastrointest Endosc. 2017; 86:700–709.
Article20. Backes Y, Moss A, Reitsma JB, Siersema PD, Moons LM. Narrow band imaging, magnifying chromoendoscopy, and gross morphological features for the optical diagnosis of T1 colorectal cancer and deep submucosal invasion: a systematic review and meta-analysis. Am J Gastroenterol. 2017; 112:54–64.
Article21. Wada Y, Kashida H, Kudo SE, Misawa M, Ikehara N, Hamatani S. Diagnostic accuracy of pit pattern and vascular pattern analyses in colorectal lesions. Dig Endosc. 2010; 22:192–199.
Article22. Li M, Ali SM, Umm-a-OmarahGilani S, Liu J, Li YQ, Zuo XL. Kudo’s pit pattern classification for colorectal neoplasms: a meta-analysis. World J Gastroenterol. 2014; 20:12649–12656.
Article23. Hata K, Watanabe T, Motoi T, Nagawa H. Pitfalls of pit pattern diagnosis in ulcerative colitis-associated dysplasia. Gastroenterology. 2004; 126:374–376.
Article24. Bisschops R, Bessissow T, Dekker E, et al. Pit pattern analysis with high-definition chromoendoscopy and narrow-band imaging for optical diagnosis of dysplasia in patients with ulcerative colitis. Gastrointest Endosc. 2017; 86:1100–1106.e1.
Article25. Carballal S, Maisterra S, López-Serrano A, et al. Real-life chromoendoscopy for neoplasia detection and characterisation in long-standing IBD. Gut. 2018; 67:70–78.
Article26. Kiesslich R, Fritsch J, Holtmann M, et al. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003; 124:880–888.
Article27. Kinoshita S, Uraoka T, Nishizawa T, et al. The role of colorectal endoscopic submucosal dissection in patients with ulcerative colitis. Gastrointest Endosc. 2018; 87:1079–1084.
Article28. Uno Y, Munakata A. The non-lifting sign of invasive colon cancer. Gastrointest Endosc. 1994; 40:485–489.
Article29. Saito Y, Otake Y, Sakamoto T, et al. Indications for and technical aspects of colorectal endoscopic submucosal dissection. Gut Liver. 2013; 7:263–269.
Article30. Yang DH, Jeong GH, Song Y, et al. The feasibility of performing colorectal endoscopic submucosal dissection without previous experience in performing gastric endoscopic submucosal dissection. Dig Dis Sci. 2015; 60:3431–3441.
Article31. Toyonaga T, Nishino E, Man IM, East JE, Azuma T. Principles of quality controlled endoscopic submucosal dissection with appropriate dissection level and high quality resected specimen. Clin Endosc. 2012; 45:362–374.
Article32. Iacopini F, Saito Y, Yamada M, et al. Curative endoscopic submucosal dissection of large nonpolypoid superficial neoplasms in ulcerative colitis (with videos). Gastrointest Endosc. 2015; 82:734–738.
Article33. Yang DH, Kim J, Song EM, et al. Outcomes of ulcerative colitis-associated dysplasia patients referred for potential endoscopic submucosal dissection. J Gastroenterol Hepatol. 2019 Feb 6 [Epub]. https://doi.org/10.1111/jgh.14623.
Article34. Fujishiro M, Yahagi N, Kashimura K, et al. Comparison of various submucosal injection solutions for maintaining mucosal elevation during endoscopic mucosal resection. Endoscopy. 2004; 36:579–583.
Article35. Vieth M, Neumann H. Current issues in inflammatory bowel disease neoplasia. Histopathology. 2015; 66:37–48.
Article36. Langner C, Magro F, Driessen A, et al. The histopathological approach to inflammatory bowel disease: a practice guide. Virchows Arch. 2014; 464:511–527.
Article37. Allende D, Elmessiry M, Hao W, et al. Inter-observer and intra-observer variability in the diagnosis of dysplasia in patients with inflammatory bowel disease: correlation of pathological and endoscopic findings. Colorectal Dis. 2014; 16:710–718. discussion 718.
Article38. Eaden J, Abrams K, McKay H, Denley H, Mayberry J. Inter-observer variation between general and specialist gastrointestinal pathologists when grading dysplasia in ulcerative colitis. J Pathol. 2001; 194:152–157.
Article39. Odze RD, Goldblum J, Noffsinger A, Alsaigh N, Rybicki LA, Fogt F. Interobserver variability in the diagnosis of ulcerative colitis-associated dysplasia by telepathology. Mod Pathol. 2002; 15:379–386.
Article40. Suzuki N, Toyonaga T, East JE. Endoscopic submucosal dissection of colitis-related dysplasia. Endoscopy. 2017; 49:1237–1242.
Article41. Ten Hove JR, Mooiweer E, Dekker E, et al. Low rate of dysplasia detection in mucosa surrounding dysplastic lesions in patients undergoing surveillance for inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2017; 15:222–228.e2.
Article42. Krugliak Cleveland N, Huo D, Sadiq F, et al. Assessment of peri-polyp biopsy specimens of flat mucosa in patients with inflammatory bowel disease. Gastrointest Endosc. 2018; 87:1304–1309.
Article43. Lahiff C, Mun Wang L, Travis SPL, East JE. Diagnostic yield of dysplasia in polyp-adjacent biopsies for patients with inflammatory bowel disease: a cross-sectional study. J Crohns Colitis. 2018; 12:670–676.
Article44. Patel N, Patel K, Ashrafian H, Athanasiou T, Darzi A, Teare J. Colorectal endoscopic submucosal dissection: systematic review of mid-term clinical outcomes. Dig Endosc. 2016; 28:405–416.
Article45. Akintoye E, Kumar N, Aihara H, Nas H, Thompson CC. Colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Endosc Int Open. 2016; 4:E1030–E1044.
Article46. Fuccio L, Hassan C, Ponchon T, et al. Clinical outcomes after endoscopic submucosal dissection for colorectal neoplasia: a systematic review and meta-analysis. Gastrointest Endosc. 2017; 86:74–86.e17.
Article47. Baars JE, Siegel CA, van’t Spijker A, Markus T, Kuipers EJ, van der Woude CJ. Inflammatory bowel disease-patients are insufficiently educated about the basic characteristics of their disease and the associated risk of colorectal cancer. Dig Liver Dis. 2010; 42:777–784.
Article48. Siegel CA, Schwartz LM, Woloshin S, et al. When should ulcerative colitis patients undergo colectomy for dysplasia? Mismatch between patient preferences and physician recommendations. Inflamm Bowel Dis. 2010; 16:1658–1662.
Article49. Lopez A, Collet-Fenetrier B, Belle A, Peyrin-Biroulet L. Patients’ knowledge and fear of colorectal cancer risk in inflammatory bowel disease. J Dig Dis. 2016; 17:383–391.
Article50. Hahnloser D, Pemberton JH, Wolff BG, Larson DR, Crownhart BS, Dozois RR. Results at up to 20 years after ileal pouch-anal anastomosis for chronic ulcerative colitis. Br J Surg. 2007; 94:333–340.
Article51. Heikens JT, de Vries J, Goos MR, Oostvogel HJ, Gooszen HG, van Laarhoven CJ. Quality of life and health status before and after ileal pouchanal anastomosis for ulcerative colitis. Br J Surg. 2012; 99:263–269.
Article52. Yoon YS, Cho YB, Park KJ, et al. Surgical outcomes of Korean ulcerative colitis patients with and without colitis-associated cancer. World J Gastroenterol. 2015; 21:3547–3553.
Article53. Fazio VW, Kiran RP, Remzi FH, et al. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg. 2013; 257:679–685.54. Beaugerie L, Itzkowitz SH. Cancers complicating inflammatory bowel disease. N Engl J Med. 2015; 372:1441–1452.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- History and Development of Accessories for Endoscopic Submucosal Dissection
- A Case of Endoscopic Full-Thickness Resection in a Patient with Gastric High-Grade Dysplasia Unsuitable for Endoscopic Submucosal Dissection
- The Clinical Accuracy of Endoscopic Ultrasonography and White Light Imaging in Gastric Endoscopic Submucosal Dissection
- Recent Advance in the Management of Dysplasia in the Ulcerative Colitis
- Debates on Colorectal Endoscopic Submucosal Dissection - Traction for Effective Dissection: Gravity Is Enough