J Korean Fract Soc.
2019 Apr;32(2):102-106. 10.12671/jkfs.2019.32.2.102.
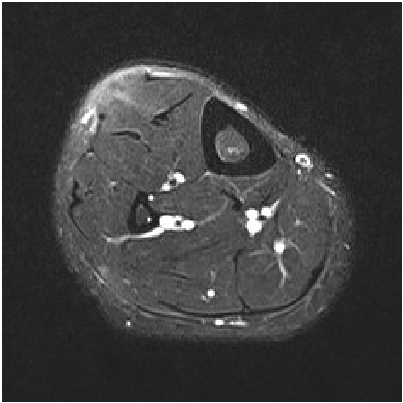
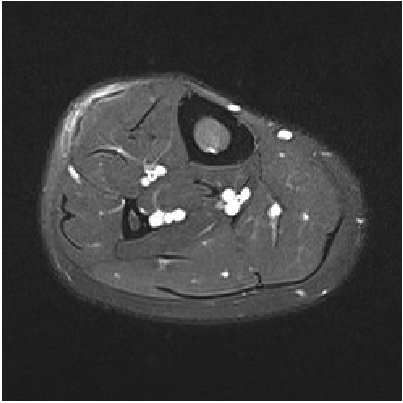
Surgical Repair of Tibialis Anterior Muscle Herniation Using a Synthetic Mesh That Was Beneath the Fascia after a Military Training Program: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Armed Forces Daejeon Hospital, Daejeon, Korea.
- 2Department of Orthopedic Surgery, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon, Korea. sysoo3180@naver.com
- KMID: 2443112
- DOI: http://doi.org/10.12671/jkfs.2019.32.2.102
Abstract
- Tibialis anterior muscle herniation is the most common type of skeletal muscle herniation of the lower legs. The treatment of muscle herniation relies on the patient's symptoms. For patients with chronic large fascial defects, fascial grafting with synthetic mesh can be considered. In this case of a patient who was exposed to excessive strain on his lower legs during a military training program, the use of a secure repair technique with synthetic mesh was required. This paper presents a case of tibialis anterior muscle herniation that was treated successfully with a monofilament knitted polypropylene mesh covered by the tibialis anterior fascia. The advantages of this technique include early rehabilitation and an early return to work. No significant difference in the clinical results compared to other methods were observed and there were no complications. The military training program appeared to have aggravated the patient's symptoms of tibialis anterior muscle herniation. On the other hand, larger scale study will be needed to determine if this program actually affects the clinical outcomes.
MeSH Terms
Figure
Reference
-
1. Miniaci A, Rorabeck CH. Tibialis anterior muscle hernia: a rationale for treatment. Can J Surg. 1987; 30:79–80.2. Siliprandi L, Martini G, Chiarelli A, Mazzoleni F. Surgical repair of an anterior tibialis muscle hernia with Mersilene mesh. Plast Reconstr Surg. 1993; 91:154–157.
Article3. Marques A, Brenda E, Amarante MT. Bilateral multiple muscle hernias of the leg repaired with Marlex mesh. Br J Plast Surg. 1994; 47:444–446.
Article4. Nguyen JT, Nguyen JL, Wheatley MJ, Nguyen TA. Muscle hernias of the leg: a case report and comprehensive review of the literature. Can J Plast Surg. 2013; 21:243–247.
Article5. Ihde H. On muscular hernia of the leg. Acta Chir Scand. 1929; 65:97–120.6. Kim M, Hong SP, Hwang SM, Park H, Ahn SK. Tibialis anterior muscle herniation developed after trauma. Int J Dermatol. 2008; 47:845–847.
Article7. Rho NK, Kim WS, Kim YJ, Yoo KH, Kim BJ, Kim MN. The use of dynamic ultrasonography for the confirmation of lower leg muscle herniation. Ann Dermatol. 2008; 20:190–192.
Article8. Harman EA, Gutekunst DJ, Frykman PN, et al. Effects of two different eight-week training programs on military physical performance. J Strength Cond Res. 2008; 22:524–534.
Article9. Simon HE, Sacchet HA. Muscle hernias of the leg: review of literature and report of twelve cases. Am J Surg. 1945; 67:87–97.10. Choi YR, Hong CG. Repair of tibialis anterior muscle herniation using periosteum. Orthopedics. 2014; 37:748–750.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Tibial Muscle Hernia Treated with Local Periosteal Rotational Flap: A Case Report
- Bilateral Tibialis Anterior Muscle Herniation
- The Use of Dynamic Ultrasonography for the Confirmation of Lower Leg Muscle Herniation
- Diagnosis of Herniated Tibialis Anterior Muscle by Dynamic Ultrasonography: A Case Report
- Avulsion Fracture of Medial Cuneiform by Tibialis Anterior Tendon (A Case Report)