Ann Dermatol.
2008 Dec;20(4):190-192. 10.5021/ad.2008.20.4.190.
The Use of Dynamic Ultrasonography for the Confirmation of Lower Leg Muscle Herniation
- Affiliations
-
- 1Leaders Clinic, Seoul, Korea.
- 2Department of Dermatology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Dermatology, College of Medicine, Chung-Ang University, Seoul, Korea. beomjoon@unitel.co.kr
- KMID: 2156391
- DOI: http://doi.org/10.5021/ad.2008.20.4.190
Abstract
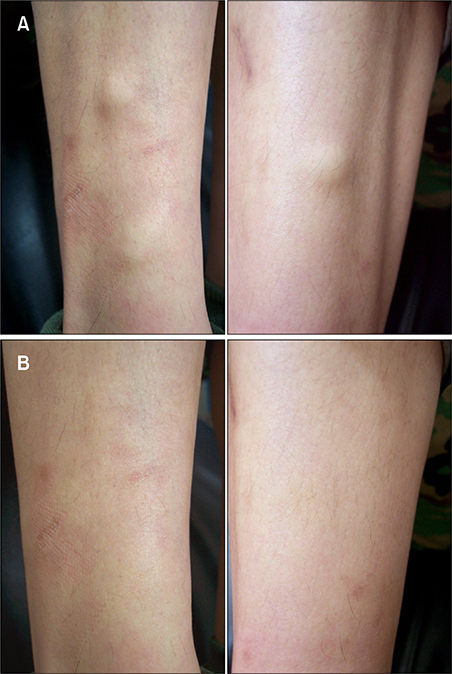
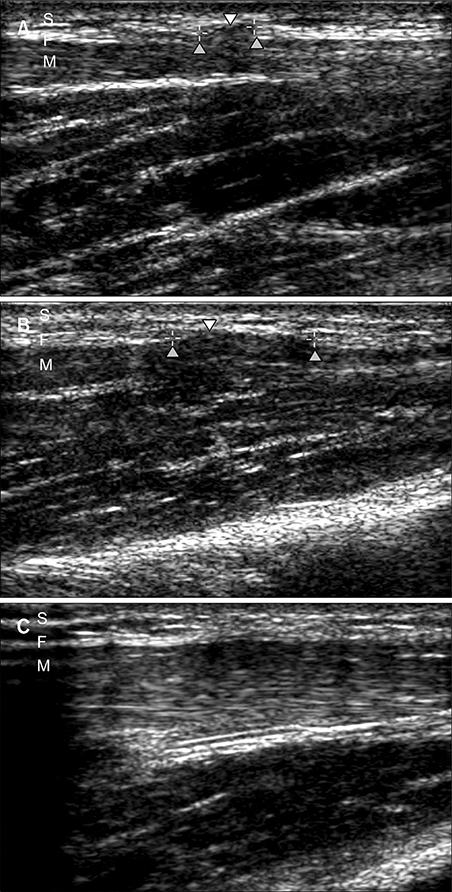
- The term muscle herniation represents focal muscular protrusions through an acquired or congenital fascial defect. The anterior tibialis muscle is the most common site of herniation. Dynamic ultrasonography has become an important tool in dermatology for diagnosing suspected muscle herniation because it is a non-invasive, highly accurate, readily available and cost-effective imaging technique. We present here the case of a 21-year-old male Korean soldier who underwent dynamic ultrasonography to confirm the diagnosis of anterior tibialis muscle herniation.
Figure
Cited by 1 articles
-
Surgical Repair of Tibialis Anterior Muscle Herniation Using a Synthetic Mesh That Was Beneath the Fascia after a Military Training Program: A Case Report
Kyoung-Ho Kim, Young-Soo Shin
J Korean Fract Soc. 2019;32(2):102-106. doi: 10.12671/jkfs.2019.32.2.102.
Reference
-
1. Lane JE, Woody CM, Lesher JL. Tibialis anterior muscle herniation. Dermatol Surg. 2002; 28:641–642.
Article2. Bates DG. Dynamic ultrasound findings of bilateral anterior tibialis muscle herniation in a pediatric patient. Pediatr Radiol. 2001; 31:753–755.
Article3. Mellado JM, Perez del Palomar L. Muscle hernias of the lower leg: MRI findings. Skeletal Radiol. 1999; 28:465–469.
Article4. Bianchi S, Abdelwahab IF, Mazzola CG, Ricci G, Damiani S. Sonographic examination of muscle herniation. J Ultrasound Med. 1995; 14:357–360.
Article5. Berglund HT, Stocks GW. Muscle hernia in a recreational athlete. Orthop Rev. 1993; 22:1246–1248.6. Egan TJ, Lemos M, Iorio R. Muscular herniation of the lower extremities. Am J Orthop. 1998; 27:102–106.7. Naversen DN, Trask DM, Watson FH, Burket JM. Painful tumors of the skin: "LEND AN EGG". J Am Acad Dermatol. 1993; 28(2 pt 2):298–300.
Article8. Zeiss J, Ebraheim NA, Woldenberg LS. Magnetic resonance imaging in the diagnosis of anterior tibialis muscle herniation. Clin Orthop Relat Res. 1989; 244:249–253.
Article9. Schmid-Wendtner MH, Burgdorf W. Ultrasound scanning in dermatology. Arch Dermatol. 2005; 141:217–224.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of Herniated Tibialis Anterior Muscle by Dynamic Ultrasonography: A Case Report
- Bilateral Tibialis Anterior Muscle Herniation
- Dynamic Ultrasonography in Musculoskeletal System-Lower Extremity and Miscellaneous disorders
- Usefulness of Ultrasonographic Examination of Diagnosis of Muscle Hernia
- Surgical Repair of Tibialis Anterior Muscle Herniation Using a Synthetic Mesh That Was Beneath the Fascia after a Military Training Program: A Case Report