J Cardiovasc Imaging.
2019 Apr;27(2):122-133. 10.4250/jcvi.2019.27.e20.
Prognostic Implications of the Left Atrial Volume Index in Patients with Progressive Mitral Stenosis
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, Seoul, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Myungji Hospital, Goyang, Korea.
- 3Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. hjchang@yuhs.ac
- KMID: 2442746
- DOI: http://doi.org/10.4250/jcvi.2019.27.e20
Abstract
- BACKGROUND
Limited data are available on the prognosis of progressive mitral stenosis (MS). We evaluated the factors associated with adverse events in patients with progressive MS.
METHODS
We retrospectively analyzed 259 consecutive patients with pure progressive MS with a mitral valve area (MVA) between 1.5 and 2.0 cm². The primary outcome measures were a composite endpoint of cardiac death, heart failure hospitalization, mitral valve surgery or percutaneous mitral valvuloplasty, and ischemic stroke.
RESULTS
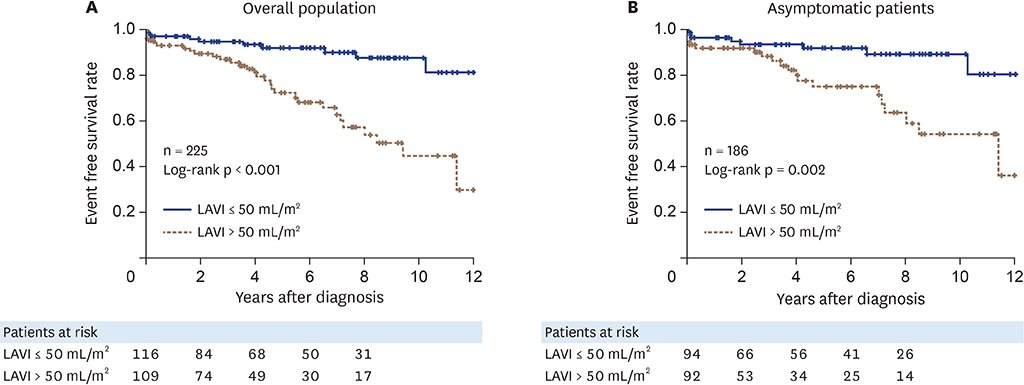
The mean patient age was 62 ± 12 years, and the mean MVA was 1.71 ± 0.15 cm². Over a median follow-up duration of 52 months, a total of 41 patients (18.3%) experienced the composite endpoint. In multivariable Cox regression analysis, prior stroke (hazard ratio [HR], 4.54; 95% confidence interval [CI], 2.16-9.54; p < 0.001) and left atrial volume index (LAVI) of > 50 mL/m² (HR, 4.45; 95% CI, 1.31-15.31; p = 0.017) were identified as independent predictors of the composite endpoint, even after adjusting for age and sex. Patients with a LAVI ≤ 50 mL/m² demonstrated favorable event-free survival compared with those with a LAVI > 50 mL/m² in either the overall population (p < 0.001) or asymptomatic patients (p = 0.002). Atrial fibrillation (AF), left ventricular mass index (LVMI), MVA, and mean diastolic pressure were factors independently associated with LAVI (all p < 0.05).
CONCLUSIONS
A deleterious impact of a high LAVI on outcome was observed in patients with progressive MS. The LAVI was mainly influenced by the presence of AF, the severity of MS, and LVMI in this population.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prognostic Value of Left Atrial Volume in Patients with Progressive Mitral Stenosis: A Possible Analogy with Left Ventricular Mass in the Setting of Pressure Overload
Jun-Bean Park
J Cardiovasc Imaging. 2019;27(2):134-136. doi: 10.4250/jcvi.2019.27.e23.
Reference
-
1. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:e57–e185.2. Boon NA, Bloomfield P. The medical management of valvar heart disease. Heart. 2002; 87:395–400.
Article3. Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2017; 38:2739–2791.4. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137:263–272.5. Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003; 139:137–147.
Article6. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14.
Article7. Sanfilippo AJ, Abascal VM, Sheehan M, et al. Atrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic study. Circulation. 1990; 82:792–797.
Article8. Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713.9. Hatle L, Angelsen B, Tromsdal A. Noninvasive assessment of atrioventricular pressure half-time by Doppler ultrasound. Circulation. 1979; 60:1096–1104.
Article10. Nunes MC, Hung J, Barbosa MM, et al. Impact of net atrioventricular compliance on clinical outcome in mitral stenosis. Circ Cardiovasc Imaging. 2013; 6:1001–1008.
Article11. Flachskampf FA, Weyman AE, Guerrero JL, Thomas JD. Calculation of atrioventricular compliance from the mitral flow profile: analytic and in vitro study. J Am Coll Cardiol. 1992; 19:998–1004.
Article12. Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017; 30:303–371.13. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.
Article14. Heidbuchel H, Verhamme P, Alings M, et al. Updated European Heart Rhythm Association practical guide on the use of non-vitamin-K antagonist anticoagulants in patients with non-valvular atrial fibrillation: executive summary. Eur Heart J. 2017; 38:2137–2149.
Article15. Takemoto Y, Barnes ME, Seward JB, et al. Usefulness of left atrial volume in predicting first congestive heart failure in patients ≥ 65 years of age with well-preserved left ventricular systolic function. Am J Cardiol. 2005; 96:832–836.16. Pritchett AM, Mahoney DW, Jacobsen SJ, Rodeheffer RJ, Karon BL, Redfield MM. Diastolic dysfunction and left atrial volume: a population-based study. J Am Coll Cardiol. 2005; 45:87–92.17. Tamura H, Watanabe T, Nishiyama S, et al. Increased left atrial volume index predicts a poor prognosis in patients with heart failure. J Card Fail. 2011; 17:210–216.
Article18. Yang WI, Shim CY, Kim YJ, et al. Left atrial volume index: a predictor of adverse outcome in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2009; 22:1338–1343.
Article19. Tani T, Yagi T, Kitai T, et al. Left atrial volume predicts adverse cardiac and cerebrovascular events in patients with hypertrophic cardiomyopathy. Cardiovasc Ultrasound. 2011; 9:34.
Article20. Møller JE, Hillis GS, Oh JK, et al. Left atrial volume: a powerful predictor of survival after acute myocardial infarction. Circulation. 2003; 107:2207–2212.21. Beinart R, Boyko V, Schwammenthal E, et al. Long-term prognostic significance of left atrial volume in acute myocardial infarction. J Am Coll Cardiol. 2004; 44:327–334.
Article22. Messika-Zeitoun D, Bellamy M, Avierinos JF, et al. Left atrial remodelling in mitral regurgitation--methodologic approach, physiological determinants, and outcome implications: a prospective quantitative Doppler-echocardiographic and electron beam-computed tomographic study. Eur Heart J. 2007; 28:1773–1781.
Article23. Le Tourneau T, Messika-Zeitoun D, Russo A, et al. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. J Am Coll Cardiol. 2010; 56:570–578.
Article24. Ancona R, Comenale Pinto S, Caso P, et al. Two-dimensional atrial systolic strain imaging predicts atrial fibrillation at 4-year follow-up in asymptomatic rheumatic mitral stenosis. J Am Soc Echocardiogr. 2013; 26:270–277.
Article25. Casaclang-Verzosa G, Gersh BJ, Tsang TS. Structural and functional remodeling of the left atrium: clinical and therapeutic implications for atrial fibrillation. J Am Coll Cardiol. 2008; 51:1–11.26. Cho IJ, Hong GR, Lee SH, et al. Differences in characteristics, left atrial reverse remodeling, and functional outcomes after mitral valve replacement in patients with low-gradient very severe mitral stenosis. J Am Soc Echocardiogr. 2016; 29:759–767.27. Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016; 29:277–314.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Value of Left Atrial Volume in Patients with Progressive Mitral Stenosis: A Possible Analogy with Left Ventricular Mass in the Setting of Pressure Overload
- Relation between Atrial Fibrillation and Echocardiographic Size of Left Atrium
- Echocardiographic Study on the Mitral Valvular Heart Diseases
- Free-Floating Left Atrial Thrombus with Recurrent cerebral Embolic Event Associated Mitral Stenosis
- Assessment of Left Atrial Function Using Instantaneous Pressure-Volume Relations in Mitral Stenosis before and after Percutaneous Mitral Balloon Valvuloplasty