Ann Rehabil Med.
2018 Feb;42(1):42-51. 10.5535/arm.2018.42.1.42.
Usefulness of Early Videofluoroscopic Swallowing Study in Acute Stroke Patients With Dysphagia
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Dong-A University College of Medicine & Busan-Ulsan Regional Cardiocerebrovascular Center, Busan, Korea. flaehdrbs@naver.com
- KMID: 2440968
- DOI: http://doi.org/10.5535/arm.2018.42.1.42
Abstract
OBJECTIVE
To demonstrate the usefulness of early videofluoroscopic swallowing study (VFSS) and to investigate change patterns in dietary methods in stroke patients with dysphagia.
METHODS
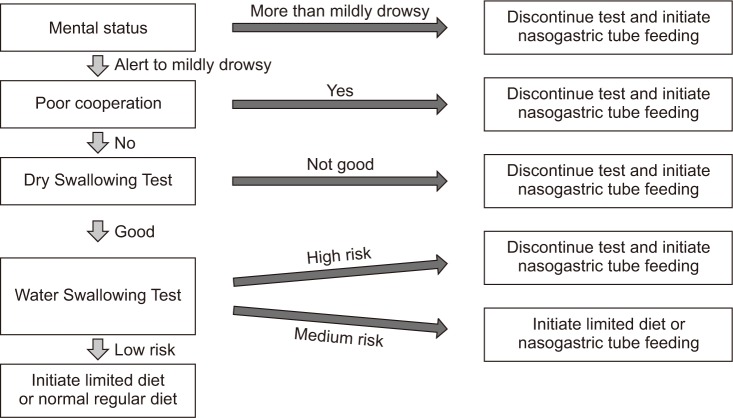
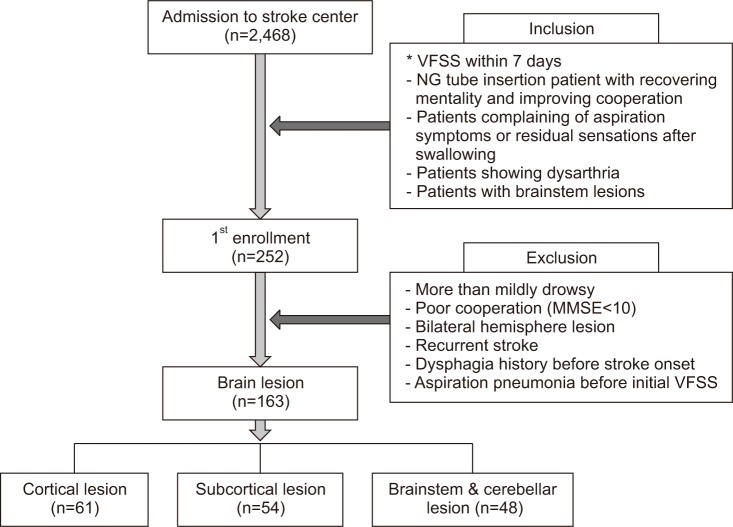
The VFSS was performed within 7 days of stroke onset in neurologically stable patients. The patients were divided into three groups according to type of brain lesion: cortical lesion (CL), subcortical lesion (SCL), and brainstem/cerebellar lesion (BCL). Based on the VFSS results, this study investigated change patterns in feeding method and discrepancies in the aspiration risk predicted by the Water Swallowing Test (WST) and the VFSS. Complications, such as aspiration pneumonia, were also evaluated.
RESULTS
A total of 163 patients met the inclusion criteria and the VFSS was performed within 7 days of stroke. Patients considered at risk for aspiration (Penetration-Aspiration Scale [PAS] scores of 6 to 8) were found in all three groups using the VFSS (47.5% of the CL group, 59.3% of the SCL group, and 47.9% of the BCL group). After early VFSS, 79.7% of the patients were assessed to require restricted feeding methods. A 19.0% discrepancy was found between the WST and VFSS results. At 3-week follow-up after the VFSS, aspiration pneumonia was observed in 12 patients (7.4%) with restricted feeding methods.
CONCLUSION
Early VFSS during the acute period can facilitate determination of the most appropriate feeding method, and support effective dysphagia management for stroke patients.
MeSH Terms
Figure
Cited by 2 articles
-
Epiglottic Retroflexion is a Key Indicator of Functional Recovery of Post-stroke Dysphagia
Ji Soo Choi, Hyun Bang, Goo Joo Lee, Han Gil Seo, Byung-Mo Oh, Tai Ryoon Han
Ann Rehabil Med. 2020;44(1):1-10. doi: 10.5535/arm.2020.44.1.1.Correlation of Videofluoroscopic Swallowing Study Findings With Radionuclide Salivagram in Chronic Brain-Injured Patients
Ga Yang Shim, Ju Sun Oh, Seunghee Han, Kyungyeul Choi, Son Mi Lee, Min Woo Kim
Ann Rehabil Med. 2021;45(2):108-115. doi: 10.5535/arm.20171.
Reference
-
1. Axelsson K, Norberg A, Asplund K. Eating after a stroke: towards an integrated view. Int J Nurs Stud. 1984; 21:93–99. PMID: 6589215.2. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.3. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.4. Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003; 60:620–625. PMID: 12601102.
Article5. Doggett DL, Tappe KA, Mitchell MD, Chapell R, Coates V, Turkelson CM. Prevention of pneumonia in elderly stroke patients by systematic diagnosis and treatment of dysphagia: an evidence-based comprehensive analysis of the literature. Dysphagia. 2001; 16:279–295. PMID: 11720404.
Article6. Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S, et al. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005; 36:1972–1976. PMID: 16109909.
Article7. Middleton S, McElduff P, Ward J, Grimshaw JM, Dale S, D'Este C, et al. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): a cluster randomised controlled trial. Lancet. 2011; 378:1699–1706. PMID: 21996470.
Article8. Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000; 283:3102–3109. PMID: 10865305.9. Gomes CA Jr, Lustosa SA, Matos D, Andriolo RB, Waisberg DR, Waisberg J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst Rev. 2010; 11:CD008096.10. Heckert KD, Komaroff E, Adler U, Barrett AM. Postacute reevaluation may prevent dysphagia-associated morbidity. Stroke. 2009; 40:1381–1385. PMID: 19228843.
Article11. Palmer JB, Kuhlemeier KV, Tippett DC, Lynch C. A protocol for the videofluorographic swallowing study. Dysphagia. 1993; 8:209–214. PMID: 8359040.
Article12. Smithard DG. Dysphagia management and stroke units. Curr Phys Med Rehabil Rep. 2016; 4:287–294. PMID: 28018754.
Article13. Smith Hammond CA, Goldstein LB, Horner RD, Ying J, Gray L, Gonzalez-Rothi L, et al. Predicting aspiration in patients with ischemic stroke: comparison of clinical signs and aerodynamic measures of voluntary cough. Chest. 2009; 135:769–777. PMID: 19017886.14. Massey R, Jedlicka D. The Massey Bedside Swallowing Screen. J Neurosci Nurs. 2002; 34:252–253. PMID: 12391741.
Article15. Han DS, Chang YC, Lu CH, Wang TG. Comparison of disordered swallowing patterns in patients with recurrent cortical/subcortical stroke and first-time brainstem stroke. J Rehabil Med. 2005; 37:189–191. PMID: 16040477.
Article16. Gonzalez-Fernandez M, Kleinman JT, Ky PK, Palmer JB, Hillis AE. Supratentorial regions of acute ischemia associated with clinically important swallowing disorders: a pilot study. Stroke. 2008; 39:3022–3028. PMID: 18688014.17. Galovic M, Leisi N, Muller M, Weber J, Abela E, Kagi G, et al. Lesion location predicts transient and extended risk of aspiration after supratentorial ischemic stroke. Stroke. 2013; 44:2760–2767. PMID: 23887840.
Article18. Lee SJ, Lee KW, Kim SB, Lee JH, Park MK. Voluntary cough and swallowing function characteristics of acute stroke patients based on lesion type. Arch Phys Med Rehabil. 2015; 96:1866–1872. PMID: 26184890.
Article19. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article20. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article21. Flowers HL, Skoretz SA, Streiner DL, Silver FL, Martino R. MRI-based neuroanatomical predictors of dysphagia after acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2011; 32:1–10.
Article22. Perry L, Love CP. Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia. 2001; 16:7–18. PMID: 11213249.
Article23. Kidd D, Lawson J, Nesbitt R, MacMahon J. The natural history and clinical consequences of aspiration in acute stroke. QJM. 1995; 88:409–413. PMID: 7648232.24. ECRI Health Technology Assessment Group. Diagnosis and treatment of swallowing disorders (dysphagia) in acute-care stroke patients. Evid Rep Technol Assess (Summ). 1999; 8:1–6.25. Vernino S, Brown RD Jr, Sejvar JJ, Sicks JD, Petty GW, O'Fallon WM. Cause-specific mortality after first cerebral infarction: a population-based study. Stroke. 2003; 34:1828–1832. PMID: 12855836.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Instrumental Assessment of Swallowing
- The Functional Dysphagia Scale Using Videofluoroscopic Swallowing Study in Stroke Patients
- Scoring System in Videofluoroscopic Swallowing Study
- Validation of Gugging Swallowing Screen for Patients with Stroke Based on Videofluoroscopic Swallowing Study
- Dysphagia Pattern according to Stroke Location