Korean J Gastroenterol.
2019 Feb;73(2):105-108. 10.4166/kjg.2019.73.2.105.
Achalasia Cardia Resulting in Bronchial Obstruction: A Case Series and Literature Review
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, SBH Health System, Bronx, NY, USA.
- 2Division of Gastroenterology and Hepatology, Mercy One Des Moines Medical Center, Des Moines, IA, USA. tagoresunkara@hotmail.com
- 3Division of Gastroenterology and Hepatology, Bronx Lebanon Hospital Center, Bronx, NY, USA.
- KMID: 2438710
- DOI: http://doi.org/10.4166/kjg.2019.73.2.105
Abstract
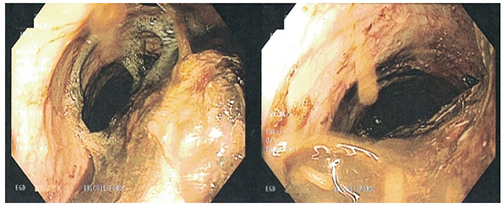
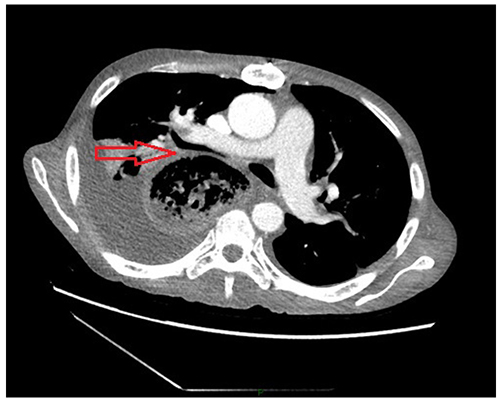
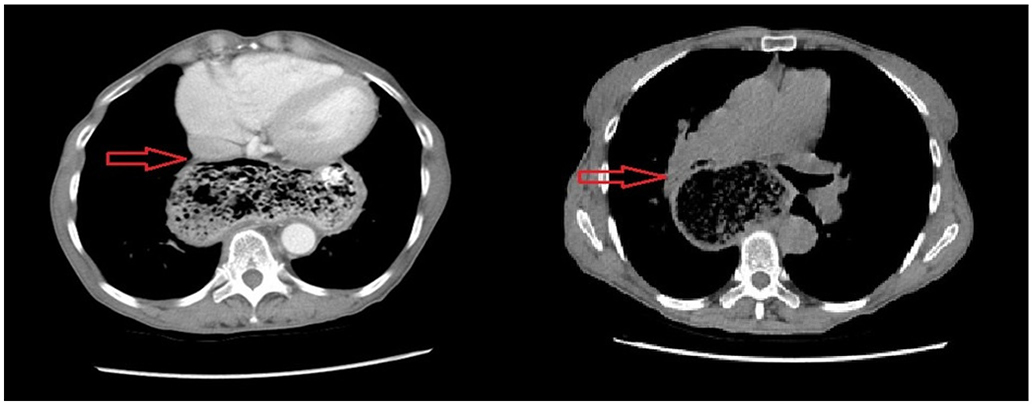
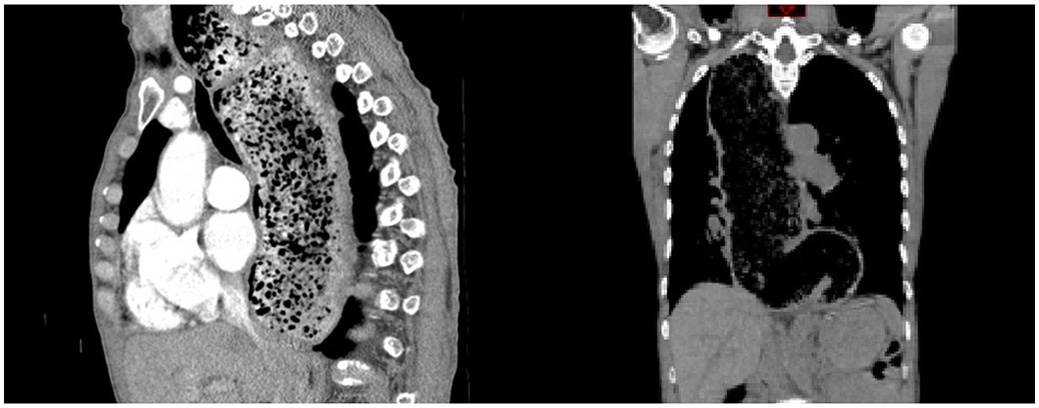
- Achalasia is a motility disorder of the esophagus that is characterized by loss of ganglionic neurons within the myenteric plexus of the lower esophageal sphincter (LES) resulting in failure of the LES to relax. Clinically this disorder presents with simultaneous dysphagia to solids and liquids, and if left untreated, leads to esophageal dilation, which can give rise to many adverse consequences. Extrinsic compression of respiratory structures is one such consequence, and rarely, cases of tracheal compression secondary to achalasia have been reported. However, cases of extrinsic bronchial compression are yet rarer. Here, we present a case series comprised of two patients with achalasia who presented with extrinsic bronchial compression by a dilated esophagus secondary to achalasia.
Keyword
MeSH Terms
Figure
Reference
-
1. Ali HA, Murali G, Mukhtar B. Respiratory failure due to achalasia cardia. Respir Med CME. 2009; 2:40–43.
Article2. Ates F, Vaezi MF. The pathogenesis and management of achalasia: current status and future directions. Gut Liver. 2015; 9:449–463.
Article3. Pandolfino JE, Gawron AJ. Achalasia: a systematic review. JAMA. 2015; 313:1841–1852.4. Khan AA, Shah SW, Alam A, et al. Achalasia esophagus; presenting as acute air way obstruction. J Pak Med Assoc. 2007; 57:423–425.5. Bello CT, Lewin JR, Norris CM, Farrar GE Jr. Achalasia (cardiospasm); report of a case with extreme and unusual manifestations. Ann Intern Med. 1950; 32:1184–1190.
Article6. Hifumi T, Okada I, Inoue J, Koido Y. Cardiopulmonary arrest owing to oesophageal achalasia recovered completely with cardiopulmonary resuscitation followed by therapeutic hypothermia. BMJ Case Rep. 2013; 2013:pii: bcr2012008378.
Article7. Becker DJ, Castell DO. Acute airway obstruction in achalasia. Possible role of defective belch reflex. Gastroenterology. 1989; 97:1323–1326.8. Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol. 2011; 8:311–319.
Article9. Massey BT, Hogan WJ, Dodds WJ, Dantas RO. Alteration of the upper esophageal sphincter belch reflex in patients with achalasia. Gastroenterology. 1992; 103:1574–1579.
Article10. Andolfi C, Kavitt RT, Herbella FA, Patti MG. Achalasia and respiratory symptoms: effect of laparoscopic heller myotomy. J Laparoendosc Adv Surg Tech A. 2016; 26:675–679.
Article11. Gupta M, Ghoshal UC, Jindal S, Misra A, Nath A, Saraswat VA. Respiratory dysfunction is common in patients with achalasia and improves after pneumatic dilation. Dig Dis Sci. 2014; 59:744–752.
Article12. González ES, Bellver VO, Jaime FC, Cortés JA, Gil VG. Opioid-induced lower esophageal sphincter dysfunction. J Neurogastroenterol Motil. 2015; 21:618–620.
Article13. Ravi K, Murray JA, Geno DM, Katzka DA. Achalasia and chronic opiate use: innocent bystanders or associated conditions? Dis Esophagus. 2016; 29:15–21.
Article14. Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008; 135:1526–1533.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Review of Factors Predicting Outcome of Pneumatic Dilation in Patients With Achalasia Cardia
- An extremely rare coexistence of achalasia cardia with esophageal leiomyoma: An endoscopic treatment approach
- Achalasia Cardia Subtyping by High-Resolution Manometry Predicts the Therapeutic Outcome of Pneumatic Balloon Dilatation
- Role of Peroral Endoscopic Myotomy in Advanced Achalasia Cardia With Sigmoid and/or Megaesophagus: A Systematic Review and Metanalysis
- Achalasia During Pregnancy: Proposed Management Algorithm Based on a Thorough Literature Review