Intest Res.
2019 Jan;17(1):107-118. 10.5217/ir.2018.00099.
Health-related quality of life of patients with inflammatory bowel disease in Singapore
- Affiliations
-
- 1Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore.
- 2Department of Pharmacy, Woodlands Health Campus, Singapore.
- 3Department of Pharmacy, Singapore General Hospital, Singapore. ong.wan.chee@sgh.com.sg
- KMID: 2438449
- DOI: http://doi.org/10.5217/ir.2018.00099
Abstract
- BACKGROUND/AIMS
Inflammatory bowel disease (IBD) is associated with considerable impairment of patients' health-related quality of life (HRQoL). Knowledge of factors that significantly affect IBD patients' HRQoL can contribute to better patient care. However, the HRQoL of IBD patients in non-Western countries are limited. Hence, we assessed the HRQoL of Singaporean IBD patients and identified its determinants.
METHODS
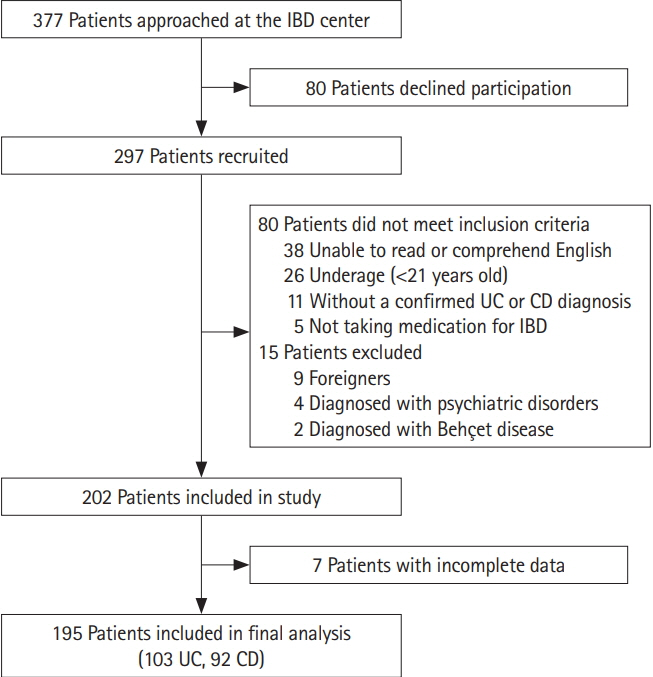
A prospective, cross-sectional study was conducted at Singapore General Hospital outpatient IBD Centre. The HRQoL of IBD patients was assessed using the short IBD questionnaire (SIBDQ), Short Form-36 physical and mental component summary (SF-36 PCS/MCS) and EuroQol 5-dimensions 3-levels (EQ-5D-3L) and visual analogue scale (VAS). Independent samples t-test was used to compare HRQoL between Crohn's disease (CD) and ulcerative colitis (UC). Determinants of HRQoL were identified through multiple linear regression.
RESULTS
A total of 195 IBD patients (103 UC, 92 CD) with a mean disease duration of 11.2 years were included. There was no significant difference in HRQoL between patients with UC and CD. Factors that significantly worsened HRQoL were presence of active disease (b=−6.293 [SIBDQ], −9.409 [PCS], −9.743 [MCS], −7.254 [VAS]), corticosteroids use (b=−7.392 [SIBDQ], −10.390 [PCS], −8.827 [MCS]), poor medication adherence (b=−4.049 [SIBDQ], −1.320 [MCS], −8.961 [VAS]), presence of extraintestinal manifestations (b=−13.381 [PCS]), comorbidities (b=−4.531 [PCS]), non-employment (b=−9.738 [MCS], −0.104 [EQ-5D-3L]) and public housing (b=−8.070 [PCS], −9.207 [VAS]).
CONCLUSIONS
The HRQoL is impaired in this Asian cohort of IBD. The magnitude of HRQoL impairment was similar in UC and CD. Clinical characteristics were better determinants of patients' HRQoL than socio-demographic factors. Recognizing the factors that impact patients' HRQoL would improve the holistic management of IBD patients.
Keyword
MeSH Terms
-
Adrenal Cortex Hormones
Asian Continental Ancestry Group
Cohort Studies
Colitis, Ulcerative
Comorbidity
Cross-Sectional Studies
Hospitals, General
Humans
Inflammatory Bowel Diseases*
Linear Models
Medication Adherence
Outpatients
Patient Care
Prospective Studies
Public Housing
Quality of Life*
Singapore*
Adrenal Cortex Hormones
Figure
Cited by 1 articles
-
Landscape of inflammatory bowel disease in Singapore
Daren Low, Nidhi Swarup, Toshiyuki Okada, Emiko Mizoguchi
Intest Res. 2022;20(3):291-296. doi: 10.5217/ir.2021.00089.
Reference
-
1. Elson CO, Cong Y. Host-microbiota interactions in inflammatory bowel disease. Gut Microbes. 2012; 3:332–344.
Article2. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asiapacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013; 145:158–165.
Article3. Gan E. Bowel disease sufferers at higher risk of anxiety. TODAY Web site. https://www.todayonline.com/daily-focus/bowel-disease-sufferers-higher-risk-anxiety. Accessed August 10, 2016.4. Colìa R, Corrado A, Cantatore FP. Rheumatologic and extraintestinal manifestations of inflammatory bowel diseases. Ann Med. 2016; 48:577–585.
Article5. Bernklev T, Jahnsen J, Henriksen M, et al. Relationship between sick leave, unemployment, disability, and health-related quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12:402–412.
Article6. Keeton RL, Mikocka-Walus A, Andrews JM. Concerns and worries in people living with inflammatory bowel disease (IBD): a mixed methods study. J Psychosom Res. 2015; 78:573–578.
Article7. Casellas F, López-Vivancos J, Casado A, Malagelada JR. Factors affecting health related quality of life of patients with inflammatory bowel disease. Qual Life Res. 2002; 11:775–781.8. Drossman DA, Patrick DL, Mitchell CM, Zagami EA, Appelbaum MI. Health-related quality of life in inflammatory bowel disease. Functional status and patient worries and concerns. Dig Dis Sci. 1989; 34:1379–1386.9. Larsson K, Lööf L, Rönnblom A, Nordin K. Quality of life for patients with exacerbation in inflammatory bowel disease and how they cope with disease activity. J Psychosom Res. 2008; 64:139–148.
Article10. Porter ME. What is value in health care? N Engl J Med. 2010; 363:2477–2481.
Article11. Bernklev T, Jahnsen J, Lygren I, Henriksen M, Vatn M, Moum B. Health-related quality of life in patients with inflammatory bowel disease measured with the short form-36: psychometric assessments and a comparison with general population norms. Inflamm Bowel Dis. 2005; 11:909–918.
Article12. Love JR, Irvine EJ, Fedorak RN. Quality of life in inflammatory bowel disease. J Clin Gastroenterol. 1992; 14:15–19.
Article13. Zhou Y, Ren W, Irvine EJ, Yang D. Assessing health-related quality of life in patients with inflammatory bowel disease in Zhejiang, China. J Clin Nurs. 2010; 19:79–88.
Article14. Nurmi E, Haapamäki J, Paavilainen E, Rantanen A, Hillilä M, Arkkila P. The burden of inflammatory bowel disease on health care utilization and quality of life. Scand J Gastroenterol. 2013; 48:51–57.
Article15. Pallis AG, Vlachonikolis IG, Mouzas IA. Assessing health-related quality of life in patients with inflammatory bowel disease, in Crete, Greece. BMC Gastroenterol. 2002; 2:1.
Article16. Haapamäki J, Turunen U, Roine RP, Färkkilä MA, Arkkila PE. Impact of demographic factors, medication and symptoms on disease-specific quality of life in inflammatory bowel disease. Qual Life Res. 2009; 18:961–969.
Article17. Casellas F, Arenas JI, Baudet JS, et al. Impairment of health-related quality of life in patients with inflammatory bowel disease: a Spanish multicenter study. Inflamm Bowel Dis. 2005; 11:488–496.
Article18. Levenstein S, Li Z, Almer S, et al. Cross-cultural variation in disease-related concerns among patients with inflammatory bowel disease. Am J Gastroenterol. 2001; 96:1822–1830.
Article19. Petrak F, Hardt J, Clement T, Börner N, Egle UT, Hoffmann SO. Impaired health-related quality of life in inflammatory bowel diseases: psychosocial impact and coping styles in a national German sample. Scand J Gastroenterol. 2001; 36:375–382.
Article20. Zheng K, Zhang S, Wang C, Zhao W, Shen H. Health-related quality of life in Chinese patients with mild and moderately active ulcerative colitis. PLoS One. 2015; 10:e0124211.
Article21. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.
Article22. Ediger JP, Walker JR, Graff L, et al. Predictors of medication adherence in inflammatory bowel disease. Am J Gastroenterol. 2007; 102:1417–1426.
Article23. Irvine EJ, Zhou Q, Thompson AK. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am J Gastroenterol. 1996; 91:1571–1578.24. Alrubaiy L, Rikaby I, Dodds P, Hutchings HA, Williams JG. Systematic review of health-related quality of life measures for inflammatory bowel disease. J Crohns Colitis. 2015; 9:284–292.
Article25. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992; 30:473–483.26. Coteur G, Feagan B, Keininger DL, Kosinski M. Evaluation of the meaningfulness of health-related quality of life improvements as assessed by the SF-36 and the EQ-5D VAS in patients with active Crohn’s disease. Aliment Pharmacol Ther. 2009; 29:1032–1041.
Article27. Thumboo J, Chan SP, Machin D, et al. Measuring health-related quality of life in Singapore: normal values for the English and Chinese SF-36 Health Survey. Ann Acad Med Singapore. 2002; 31:366–374.28. Luo N, Fones CS, Thumboo J, Li SC. Factors influencing healthrelated quality of life of Asians with anxiety disorders in Singapore. Qual Life Res. 2004; 13:557–565.
Article29. Stark RG, Reitmeir P, Leidl R, König HH. Validity, reliability, and responsiveness of the EQ-5D in inflammatory bowel disease in Germany. Inflamm Bowel Dis. 2010; 16:42–51.
Article30. Abdin E, Subramaniam M, Vaingankar JA, Luo N, Chong SA. Measuring health-related quality of life among adults in Singapore: population norms for the EQ-5D. Qual Life Res. 2013; 22:2983–2991.
Article31. Luo N, Chew LH, Fong KY, et al. Validity and reliability of the EQ-5D self-report questionnaire in English-speaking Asian patients with rheumatic diseases in Singapore. Qual Life Res. 2003; 12:87–92.32. EuroQol Group. EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990; 16:199–208.
Article33. Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008; 14:1660–1666.
Article34. Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980; 1:514.
Article35. Tabibian A, Tabibian JH, Beckman LJ, Raffals LL, Papadakis KA, Kane SV. Predictors of health-related quality of life and adherence in Crohn’s disease and ulcerative colitis: implications for clinical management. Dig Dis Sci. 2015; 60:1366–1374.
Article36. Velonias G, Conway G, Andrews E, et al. Older age- and healthrelated quality of life in inflammatory bowel diseases. Inflamm Bowel Dis. 2017; 23:283–288.
Article37. Burisch J, Weimers P, Pedersen N, et al. Health-related quality of life improves during one year of medical and surgical treatment in a European population-based inception cohort of patients with inflammatory bowel disease: an ECCO-EpiCom study. J Crohns Colitis. 2014; 8:1030–1042.
Article38. Graff LA, Walker JR, Lix L, et al. The relationship of inflammatory bowel disease type and activity to psychological functioning and quality of life. Clin Gastroenterol Hepatol. 2006; 4:1491–1501.
Article39. Cohen RD. The quality of life in patients with Crohn’s disease. Aliment Pharmacol Ther. 2002; 16:1603–1609.
Article40. Sainsbury A, Heatley RV. Review article: psychosocial factors in the quality of life of patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2005; 21:499–508.
Article41. Romberg-Camps MJ, Bol Y, Dagnelie PC, et al. Fatigue and health-related quality of life in inflammatory bowel disease: results from a population-based study in the Netherlands: the IBD-South Limburg cohort. Inflamm Bowel Dis. 2010; 16:2137–2147.
Article42. Han SW, McColl E, Barton JR, James P, Steen IN, Welfare MR. Predictors of quality of life in ulcerative colitis: the importance of symptoms and illness representations. Inflamm Bowel Dis. 2005; 11:24–34.43. Varni JW, Shulman RJ, Self MM, et al. Perceived medication adherence barriers mediating effects between gastrointestinal symptoms and health-related quality of life in pediatric inflammatory bowel disease. Qual Life Res. 2018; 27:195–204.
Article44. Hommel KA, Davis CM, Baldassano RN. Medication adherence and quality of life in pediatric inflammatory bowel disease. J Pediatr Psychol. 2008; 33:867–874.
Article45. Horváth G, Farkas K, Hollósi R, et al. Is there any association between impaired health-related quality of life and non-adherence to medical therapy in inflammatory bowel disease? Scand J Gastroenterol. 2012; 47:1298–1303.
Article46. Kane S, Huo D, Aikens J, Hanauer S. Medication nonadherence and the outcomes of patients with quiescent ulcerative colitis. Am J Med. 2003; 114:39–43.
Article47. van der Have M, Oldenburg B, Kaptein AA, et al. Non-adherence to Anti-TNF therapy is associated with illness perceptions and clinical outcomes in outpatients with inflammatory bowel disease: results from a prospective multicentre study. J Crohns Colitis. 2016; 10:549–555.
Article48. Kane S, Shaya F. Medication non-adherence is associated with increased medical health care costs. Dig Dis Sci. 2008; 53:1020–1024.
Article49. Haapamäki J, Roine RP, Turunen U, Färkkilä MA, Arkkila PE. Increased risk for coronary heart disease, asthma, and connective tissue diseases in inflammatory bowel disease. J Crohns Colitis. 2011; 5:41–47.
Article50. Hjortswang H, Ström M, Almer S. Health-related quality of life in Swedish patients with ulcerative colitis. Am J Gastroenterol. 1998; 93:2203–2211.
Article51. Netuveli G, Blane D. Quality of life in older ages. Br Med Bull. 2008; 85:113–126.
Article52. Webb E, Blane D, McMunn A, Netuveli G. Proximal predictors of change in quality of life at older ages. J Epidemiol Community Health. 2011; 65:542–547.
Article53. Swarup N, Nayak S, Lee J, et al. Forming a support group for people affected by inflammatory bowel disease. Patient Prefer Adherence. 2017; 11:277–281.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Landscape of inflammatory bowel disease in Singapore
- Anxiety, Depression, and Quality of Life in Parents of Adolescents with Inflammatory Bowel Disease: A Longitudinal Study
- Depressive Symptoms and Quality of Life in the Patients of Inflammatory Bowel Disease
- Clinical Implication of Sarcopenia in Patients with Inflammatory Bowel Disease
- Improving the quality of care for inflammatory bowel disease