Healthc Inform Res.
2019 Jan;25(1):12-26. 10.4258/hir.2019.25.1.12.
Effect of Mobile Health on Obese Adults: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1School of Nursing, Soonchunhyang University, Asan, Korea.
- 2Department of Health Administration, Hanyang Cyber University, Seoul, Korea. 1110006@hycu.ac.kr
- 3Department of Nursing, College of Natural Sciences, Korea National Open University, Seoul, Korea.
- KMID: 2434532
- DOI: http://doi.org/10.4258/hir.2019.25.1.12
Abstract
OBJECTIVES
This study was conducted to examine the effects of mobile health (mHealth), using mobile phones as an intervention for weight loss in obese adults.
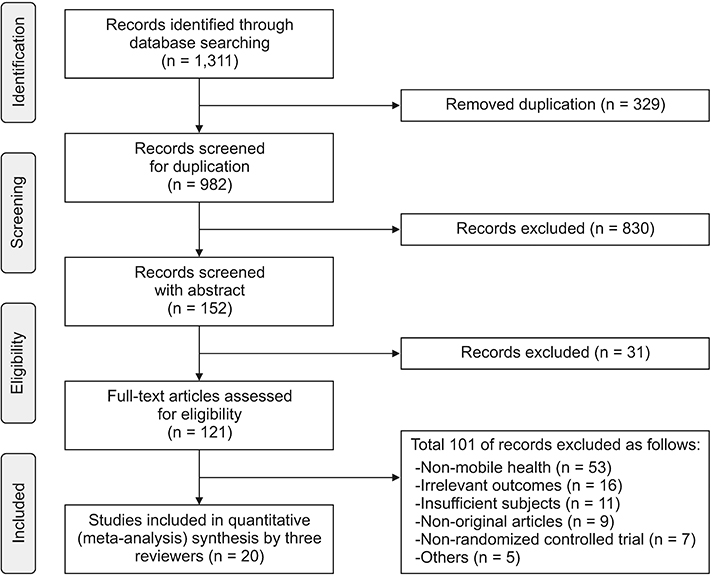
METHODS
An electronic search was carried out using multiple databases. A meta-analysis of selected studies was performed. The effects of mHealth were analyzed using changes in body weight and body mass index (BMI).
RESULTS
We identified 20 randomized controlled trials (RCTs) involving 2,318 participants who fit our inclusion criteria. The meta-analysis showed that body weight was reduced with a weighted mean difference (WMD) of −2.35 kg (95% confidence interval [CI], −2.84 to −1.87). An examination of the impact of duration of intervention showed that weight loss was greater after 6 months of mHealth (WMD = −2.66 kg) than between three and four months (WMD = −2.25 kg); it was maintained for up to 9 months (WMD = −2.62 kg). At 12 months, weight loss was reduced to a WMD of −1.23 kg. BMI decreased with a WMD of −0.77 kg/m2 (95% CI, −1.01 to −0.52). BMI changes were not statistically significant at 3 months (WMD = −1.10 kg/m2), but they were statistically significant at 6 months (WMD = −0.67 kg/m2).
CONCLUSIONS
The use of mHealth for obese adults showed a modest short-term effect on body weight and BMI. Although the weight loss associated with mHealth did not meet the recommendation of the Scottish Intercollegiate Guideline Network, which considers a reduction of approximately 5 to 10 kg of the initial body weight as a successful intervention. Well-designed RCTs are needed to reveal the effects of mHealth interventions.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. Obesity and overweight fact sheet [Internet]. Geneva, Switzerland: World Health Organization;2018. cited at 2019 Jan 10. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.2. World Health Organization. Global strategy on diet, physical activity and health [Internet]. Geneva, Switzerland: World Health Organization;2004. cited at 2019 Jan 10. Available from: http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf.3. NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016; 387(10026):1377–1396.4. Rosenbaum M, Leibel RL, Hirsch J. Obesity. N Engl J Med. 1997; 337(6):396–407.
Article5. Wadden TA, Foster GD. Behavioral assessment and treatment of markedly obese patients. In : Wadden TA, Van Itallie TB, editors. Treatment of the seriously obese patient. New York (NY): Guilford Press;1992. p. 290–330.6. National Institutes of Health. Methods for voluntary weight loss and control: National Institutes of Health Technology Assessment Conference statement Mar 30-Apr 1, 1992. Bethesda (MD): National Institutes of Health;1992.7. Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, et al. 2014 Clinical practice guidelines for overweight and obesity in Korea. Korean J Obes. 2014; 23(4):217–221.
Article8. Silva BM, Rodrigues JJ, de la Torre Diez I, Lopez-Coronado M, Saleem K. Mobile-health: a review of current state in 2015. J Biomed Inform. 2015; 56:265–272.
Article9. Vital Wave Consulting. mHealth for development: the opportunity of mobile technology for healthcare in the developing world. Washington (DC): Vodafone Foundation;2009.10. Woo HK, Sim EY, Cho YT. Big data and mobile health: public health values and future challenges. Statistical Research. 2016; (special issue):96–111.11. Boulos MN, Wheeler S, Tavares C, Jones R. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online. 2011; 10:24.
Article12. Lee MH, Kim J, Jee SH, Yoo SK. Integrated solution for physical activity monitoring based on mobile phone and PC. Healthc Inform Res. 2011; 17(1):76–86.
Article13. Ghorai K, Akter S, Khatun F, Ray P. mHealth for smoking cessation programs: a systematic review. J Pers Med. 2014; 4(3):412–423.14. Cajita MI, Gleason KT, Han HR. A systematic review of mHealth-based heart failure interventions. J Cardiovasc Nurs. 2016; 31(3):E10–E22.
Article15. Khokhar B, Jones J, Ronksley PE, Armstrong MJ, Caird J, Rabi D. Effectiveness of mobile electronic devices in weight loss among overweight and obese populations: a systematic review and meta-analysis. BMC Obes. 2014; 1:22.
Article16. Lyzwinski LN. A systematic review and meta-analysis of mobile devices and weight loss with an intervention content analysis. J Pers Med. 2014; 4(3):311–385.
Article17. Higgins JP, Green S. Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions. Chichester, UK: John Wiley & Sons;2011.18. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151(4):264–269. W64
Article19. Scottish Intercollegiate Guidelines Network. Search filters [Internet]. Edinburgh: Scottish Intercollegiate Guidelines Network;c2019. cited at 2019 Jan 10. Available from: https://www.sign.ac.uk/search-filters.html#diag.20. Pi-Sunyer FX. Obesity: criteria and classification. Proc Nutr Soc. 2000; 59(4):505–509.
Article21. Murfin M. Know your apps: an evidence-based approach to evaluation of mobile clinical applications. J Physician Assist Educ. 2013; 24(3):38–40.
Article22. Payne KB, Wharrad H, Watts K. Smartphone and medical related app use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012; 12:121.
Article23. Robinson R. App revolution: avoiding the app trap. PharmaVOICE. 2014; 14(2):24–28.24. Scottish Intercollegiate Guidelines Network. Management of obesity [Internet]. Edinburgh: Scottish Intercollegiate Guidelines Network;2010. cited at 2019 Jan 10. Available from: http://www.sign.ac.uk/sign-115-management-of-obesity.html.25. Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. P T. 2014; 39(5):356–364.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Mobile Health Applications in Older Adults with Dementia or Mild Cognitive Impairment: A Systematic Review and Meta-Analysis
- Website and Mobile Application-Based Interventions for Adolescents and Young Adults with Depression: A Systematic Review and Meta-Analysis
- An Introduction of the Systematic Review and Meta-Analysis
- Effect of Digital Health Interventions on Psychotic Symptoms among Persons with Severe Mental Illness in Community: A Systematic Review and Meta-Analysis
- Effects of medication adherence interventions for older adults with chronic illnesses: a systematic review and meta-analysis