Intest Res.
2018 Oct;16(4):509-521. 10.5217/ir.2018.00074.
Optimizing the multidimensional aspects of the patient-physician relationship in the management of inflammatory bowel disease
- Affiliations
-
- 1Gastroenterology Unit, Department of Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia. draffendi@ppukm.ukm.edu.my
- 2Health Psychology Programme, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia.
- KMID: 2434152
- DOI: http://doi.org/10.5217/ir.2018.00074
Abstract
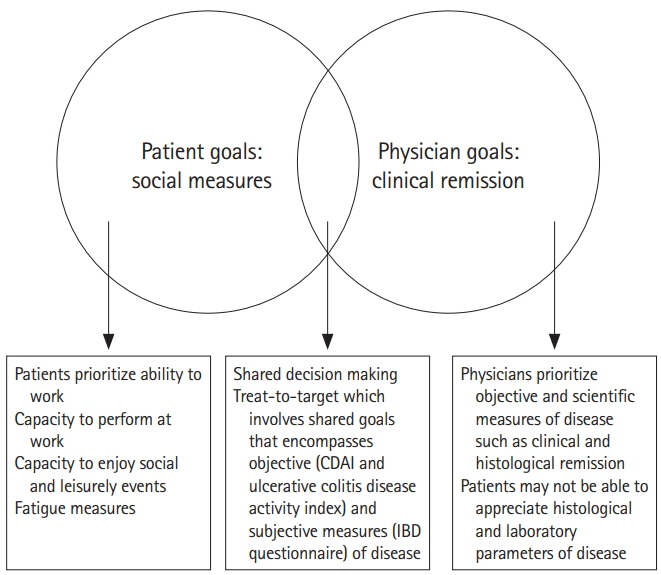
- The patient-physician relationship has a pivotal impact on the inflammatory bowel disease (IBD) outcomes. However, there are many challenges in the patient-physician relationship; lag time in diagnosis which results in frustration and an anchoring bias against the treating gastroenterologist, the widespread availability of medical information on the internet has resulted in patients having their own ideas of treatment, which may be incongruent from the treating physicians' goals resulting in patient physician discordance. Because IBD is an incurable disease, the goal of treatment is to sustain remission. To achieve this, patients may have to go through several lines of treatment. The period of receiving stepping up, top down or even accelerated stepping up medications may result in a lot of frustration and anxiety for the patient and may compromise the patient-physician relationship. IBD patients are also prone to psychological distress that further compromises the patient-physician relationship. Despite numerous published data regarding the medical and surgical treatment options available for IBD, there is a lack of data regarding methods to improve the therapeutic patient-physician relationship. In this review article, we aim to encapsulate the challenges faced in the patient-physician relationship and ways to overcome in for an improved outcome in IBD.
MeSH Terms
Figure
Reference
-
1. Kappelman MD, Moore KR, Allen JK, Cook SF. Recent trends in the prevalence of Crohn’s disease and ulcerative colitis in a commercially insured US population. Dig Dis Sci. 2013; 58:519–525.
Article2. Burisch J, Jess T, Martinato M, Lakatos PL; ECCO-EpiCom. The burden of inflammatory bowel disease in Europe. J Crohns Colitis. 2013; 7:322–337.
Article3. Ng SC. Emerging trends of inflammatory bowel disease in Asia. Gastroenterol Hepatol (N Y). 2016; 12:193–196.4. Allez M, Modigliani R. Clinical features of inflammatory bowel disease. Curr Opin Gastroenterol. 2000; 16:329–336.
Article5. Ghosh S, Mitchell R. Impact of inflammatory bowel disease on quality of life: results of the European Federation of Crohn’s and Ulcerative Colitis Associations (EFCCA) patient survey. J Crohns Colitis. 2007; 1:10–20.
Article6. Wilks S. Morbid appearances in the intestine of Miss Bankes. Med Times Gaz. 1859; 2:264–265.7. Sullivan AJ, Chandler CA. Ulcerative colitis of psychogenic origin: a report of six cases. Yale J Biol Med. 1932; 4:779–796.8. Sewitch MJ, Abrahamowicz M, Bitton A, et al. Psychological distress, social support, and disease activity in patients with inflammatory bowel disease. Am J Gastroenterol. 2001; 96:1470–1479.
Article9. Bonaz BL, Bernstein CN. Brain-gut interactions in inflammatory bowel disease. Gastroenterology. 2013; 144:36–49.
Article10. Murray C. Psychologenic factors in the etiology of ulcerative colitis and bloody diarrhea. Am J Med Sci. 1930; 180:239–248.11. Alexander F. The influence of psychological factors upon gastrointestinal disturbances: a symposium. I. General principles, objectives and preliminary results. Psychoanal Q. 1934; 3:501–539.
Article12. Banks BM, Korelitz BI, Zetzel L. The course of nonspecific ulcerative colitis: review of twenty years’ experience and late results. Gastroenterology. 1957; 32:983–1012.
Article13. Murray JB. Psychological factors in ulcerative colitis. J Gen Psychol. 1984; 110:201–221.
Article14. Goldring AB, Taylor SE, Kemeny ME, Anton PA. Impact of health beliefs, quality of life, and the physician-patient relationship on the treatment intentions of inflammatory bowel disease patients. Health Psychol. 2002; 21:219–228.
Article15. Siegel CA. Shared decision making in inflammatory bowel disease: helping patients understand the tradeoffs between treatment options. Gut. 2012; 61:459–465.
Article16. Bossuyt P, Vermeire S. Treat to target in inflammatory bowel disease. Curr Treat Options Gastroenterol. 2016; 14:61–72.
Article17. Moon CM, Jung SA, Kim SE, et al. Clinical factors and disease course related to diagnostic delay in Korean Crohn’s disease patients: results from the CONNECT study. PLoS One. 2015; 10:e0144390. doi: 10.1371/journal.pone.0144390.
Article18. Pittet V, Vaucher C, Maillard MH, et al. Information needs and concerns of patients with inflammatory bowel disease: what can we learn from participants in a bilingual clinical cohort? PLoS One. 2016; 11:e0150620. doi: 10.1371/journal.pone.0150620.
Article19. Husain A, Triadafilopoulos G. Communicating with patients with inflammatory bowel disease. Inflamm Bowel Dis. 2004; 10:444–450.
Article20. Fiandt K. The Chronic Care Model: description and application for practice. Top Adv Pract Nurs. 2006; 6(4):21. Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: practical and theoretical implications. J Soc Pers Relat. 1987; 4:497–510.
Article22. Rubin DT, Dubinsky MC, Panaccione R, et al. The impact of ulcerative colitis on patients’ lives compared to other chronic diseases: a patient survey. Dig Dis Sci. 2010; 55:1044–1052.
Article23. Riley SA, Mani V, Goodman MJ, Lucas S. Why do patients with ulcerative colitis relapse? Gut. 1990; 31:179–183.
Article24. Jelsness-Jørgensen LP, Moum B, Bernklev T. Worries and concerns among inflammatory bowel disease patients followed prospectively over one year. Gastroenterol Res Pract. 2011; 2011:492034. doi: 10.1155/2011/492034.
Article25. D’Incà R, Bertomoro P, Mazzocco K, Vettorato MG, Rumiati R, Sturniolo GC. Risk factors for non-adherence to medication in inflammatory bowel disease patients. Aliment Pharmacol Ther. 2008; 27:166–172.
Article26. Schreiber S, Panés J, Louis E, Holley D, Buch M, Paridaens K. National differences in ulcerative colitis experience and management among patients from five European countries and Canada: an online survey. J Crohns Colitis. 2013; 7:497–509.
Article27. Porcelli P, Leoci C, Guerra V. A prospective study of the relationship between disease activity and psychologic distress in patients with inflammatory bowel disease. Scand J Gastroenterol. 1996; 31:792–796.
Article28. Drossman DA, Leserman J, Li ZM, Mitchell CM, Zagami EA, Patrick DL. The rating form of IBD patient concerns: a new measure of health status. Psychosom Med. 1991; 53:701–712.
Article29. Vaucher C, Maillard MH, Froehlich F, Burnand B, Michetti P, Pittet V. Patients and gastroenterologists’ perceptions of treatments for inflammatory bowel diseases: do their perspectives match? Scand J Gastroenterol. 2016; 51:1056–1061.
Article30. Rubin DT, Dubinsky MC, Martino S, Hewett KA, Panés J. communication between physicians and patients with ulcerative colitis: reflections and insights from a qualitative study of in-office patient-physician visits. Inflamm Bowel Dis. 2017; 23:494–501.31. Baars JE, Markus T, Kuipers EJ, van der Woude CJ. Patients’ preferences regarding shared decision-making in the treatment of inflammatory bowel disease: results from a patient-empowerment study. Digestion. 2010; 81:113–119.
Article32. Loftus EV Jr, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Crohn’s disease in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gastroenterology. 1998; 114:1161–1168.
Article33. Fisher R, Ury W, Patton B. Getting to yes: negotiating agreement without giving in. New York: Penguin;2011.34. Bouguen G, Levesque BG, Feagan BG, et al. Treat to target: a proposed new paradigm for the management of Crohn’s disease. Clin Gastroenterol Hepatol. 2015; 13:1042–1050. e2.
Article35. Loftus EV, Feagan BG, Colombel JF, et al. Effects of adalimumab maintenance therapy on health-related quality of life of patients with Crohn’s disease: patient-reported outcomes of the CHARM trial. Am J Gastroenterol. 2008; 103:3132–3141.
Article36. Irvine EJ, Feagan B, Rochon J, et al. Quality of life: a valid and reliable measure of therapeutic efficacy in the treatment of inflammatory bowel disease. Canadian Crohn’s Relapse Prevention Trial Study Group. Gastroenterology. 1994; 106:287–296.
Article37. Higgins PD, Rubin DT, Kaulback K, Schoenfield PS, Kane SV. Systematic review: impact of non-adherence to 5-aminosalicylic acid products on the frequency and cost of ulcerative colitis flares. Aliment Pharmacol Ther. 2009; 29:247–257.
Article38. López San Román A, Bermejo F, Carrera E, Pérez-Abad M, Boixeda D. Adherence to treatment in inflammatory bowel disease. Rev Esp Enferm Dig. 2005; 97:249–257.
Article39. Jackson CA, Clatworthy J, Robinson A, Horne R. Factors associated with non-adherence to oral medication for inflammatory bowel disease: a systematic review. Am J Gastroenterol. 2010; 105:525–539.
Article40. Kane S, Huo D, Aikens J, Hanauer S. Medication nonadherence and the outcomes of patients with quiescent ulcerative colitis. Am J Med. 2003; 114:39–43.
Article41. Shale MJ, Riley SA. Studies of compliance with delayed-release mesalazine therapy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2003; 18:191–198.
Article42. Nigro G, Angelini G, Grosso SB, Caula G, Sategna-Guidetti C. Psychiatric predictors of noncompliance in inflammatory bowel disease: psychiatry and compliance. J Clin Gastroenterol. 2001; 32:66–68.43. Rotgers F. Motivational interviewing: preparing people to change addictive behavior. J Stud Alcohol. 1993; 54:507.
Article44. Martins RK, McNeil DW. Review of motivational interviewing in promoting health behaviors. Clin Psychol Rev. 2009; 29:283–293.
Article45. Mocciaro F, Di Mitri R, Russo G, Leone S, Quercia V. Motivational interviewing in inflammatory bowel disease patients: a useful tool for outpatient counselling. Dig Liver Dis. 2014; 46:893–897.
Article46. Mikocka-Walus A, Knowles SR, Keefer L, Graff L. Controversies revisited: a systematic review of the comorbidity of depression and anxiety with inflammatory bowel diseases. Inflamm Bowel Dis. 2016; 22:752–762.47. López-Sanromán A, Bermejo F. Review article: how to control and improve adherence to therapy in inflammatory bowel disease. Aliment Pharmacol Ther. 2006; 24 Suppl 3:45–49.
Article48. Martin-Subero M, Anderson G, Kanchanatawan B, Berk M, Maes M. Comorbidity between depression and inflammatory bowel disease explained by immune-inflammatory, oxidative, and nitrosative stress; tryptophan catabolite; and gut-brain pathways. CNS Spectr. 2016; 21:184–198.
Article49. Mikocka-Walus A, Pittet V, Rossel JB, von Känel R; Swiss IBD Cohort Study Group. Symptoms of depression and anxiety are independently associated with clinical recurrence of inflammatory bowel disease. Clin Gastroenterol Hepatol. 2016; 14:829–835. e1.50. Mikocka-Walus A, Bampton P, Hetzel D, Hughes P, Esterman A, Andrews JM. Cognitive-behavioural therapy for inflammatory bowel disease: 24-month data from a randomised controlled trial. Int J Behav Med. 2017; 24:127–135.
Article51. Yanartas O, Kani HT, Bicakci E, et al. The effects of psychiatric treatment on depression, anxiety, quality of life, and sexual dysfunction in patients with inflammatory bowel disease. Neuropsychiatr Dis Treat. 2016; 12:673–683.
Article52. Li Y, Qian JM. The challenge of inflammatory bowel disease diagnosis in Asia. Inflamm Intest Dis. 2017; 1:159–164.
Article53. Mountifield R, Andrews JM, Mikocka-Walus A, Bampton P. Doctor communication quality and Friends’ attitudes influence complementary medicine use in inflammatory bowel disease. World J Gastroenterol. 2015; 21:3663–3670.
Article54. Park DI, Cha JM, Kim HS, et al. Predictive factors of complementary and alternative medicine use for patients with inflammatory bowel disease in Korea. Complement Ther Med. 2014; 22:87–93.
Article55. Claramita M, Utarini A, Soebono H, Van Dalen J, Van der Vleuten C. Doctor-patient communication in a Southeast Asian setting: the conflict between ideal and reality. Adv Health Sci Educ Theory Pract. 2011; 16:69–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Artificial intelligence in inflammatory bowel disease: implications for clinical practice and future directions
- Nutritional concerns in pediatric inflammatory bowel disease
- Clinical aspects and treatments for pediatric inflammatory bowel diseases
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence
- First aid with color atlas for the use of intestinal ultrasound for inflammatory bowel disease in daily clinical practice