Investig Magn Reson Imaging.
2018 Dec;22(4):254-259. 10.13104/imri.2018.22.4.254.
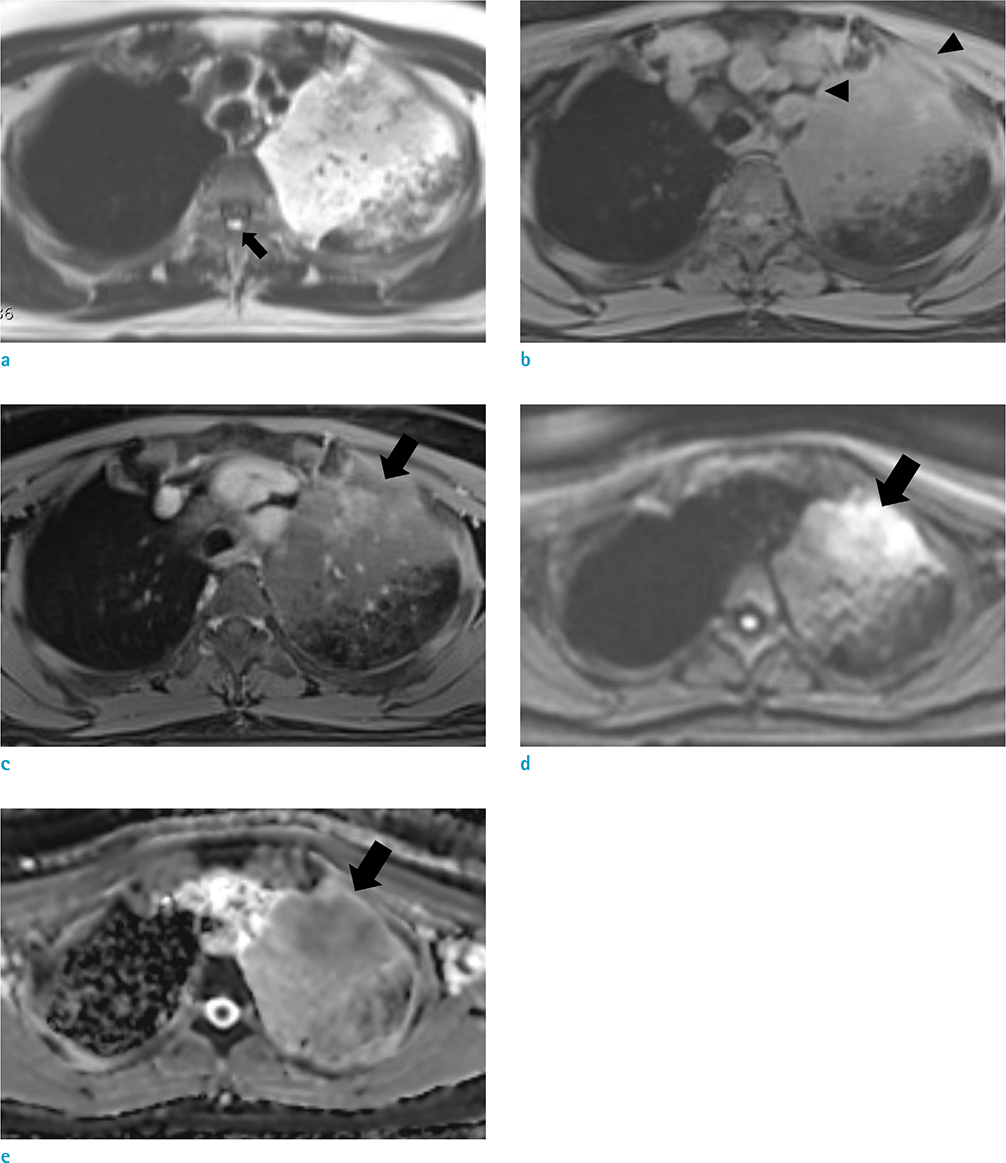
Utility of Magnetic Resonance Imaging in the Diagnosis of Lung Adenocarcinoma with Extensive Necrosis: a Case Report
- Affiliations
-
- 1Department of Radiology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea. asterism35@naver.com
- 2Department of Thoracic Surgery, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2431111
- DOI: http://doi.org/10.13104/imri.2018.22.4.254
Abstract
- Application of magnetic resonance imaging (MRI) for assessment of pulmonary disease has been limited, due to susceptibility to cardiac pulsation, respiratory motion, and inhomogeneity of the magnetic field of the lung. With technical advances of MRI and unmet clinical needs for more accurate diagnosis and assessment of the disease, however, the use of MRI for evaluation of the lung has broadened. Herein, we present a case of pneumonic-type lung adenocarcinoma in a patient with history of anaphylactic shock to iodinated contrast medium, in which MRI played a critical role for targeted lung biopsy and cancer staging. Through this paper, we would like to report potential value of MRI in assessment of lung cancer.
MeSH Terms
Figure
Reference
-
1. Khalil A, Majlath M, Gounant V, Hess A, Laissy JP, Debray MP. Contribution of magnetic resonance imaging in lung cancer imaging. Diagn Interv Imaging. 2016; 97:991–1002.
Article2. Hochhegger B, Marchiori E, Sedlaczek O, et al. MRI in lung cancer: a pictorial essay. Br J Radiol. 2011; 84:661–668.
Article3. Koyama H, Ohno Y, Seki S, et al. Magnetic resonance imaging for lung cancer. J Thorac Imaging. 2013; 28:138–150.
Article4. Kim HS, Lee KS, Ohno Y, van Beek EJ, Biederer J. PET/CT versus MRI for diagnosis, staging, and follow-up of lung cancer. J Magn Reson Imaging. 2015; 42:247–260.
Article5. Gaeta M, Ascenti G, Mazziotti S, Contiguglia R, Barone M, Mileto A. MRI differentiation of pneumonia-like mucinous adenocarcinoma and infectious pneumonia. Eur J Radiol. 2012; 81:3587–3591.
Article6. Gaeta M, Minutoli F, Ascenti G, et al. MR white lung sign: incidence and significance in pulmonary consolidations. J Comput Assist Tomogr. 2001; 25:890–896.
Article7. Liu Y, Zhang HL, Mei JZ, et al. Primary mucinous adenocarcinoma of the lung: a case report and review of the literature. Oncol Lett. 2017; 14:3701–3704.
Article8. Guimaraes MD, Marchiori E, Odisio BC, et al. Functional imaging with diffusion-weighted MRI for lung biopsy planning: initial experience. World J Surg Oncol. 2014; 12:203.
Article9. Natsume M, Sano H, Fukusada S, et al. Gadolinium as an alternative radiocontrast agent in patients with allergy to iodine-based contrast provide for useful diagnostic imagings and safely treatment of biliary tract diseases. Nihon Shokakibyo Gakkai Zasshi. 2013; 110:825–832.10. Fraioli F, Screaton NJ, Janes SM, et al. Non-small-cell lung cancer resectability: diagnostic value of PET/MR. Eur J Nucl Med Mol Imaging. 2015; 42:49–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thiemann's Disease: a Case Report
- Incidentally Detected Löffler’s Syndrome on Abdomen Magnetic Resonance Imaging: Case Report
- Collison Tumor of Adenocarcinoma and Diffuse Large B-Cell Lymphoma in the Rectum: a Case Report and Literature Review
- US and MRI Findings of Penile Metastasis from Rectal Adenocarcinoma: A Case Report
- Primary Uterine Lymphoma: A Case Report