Pediatr Gastroenterol Hepatol Nutr.
2019 Jan;22(1):86-89. 10.5223/pghn.2019.22.1.86.
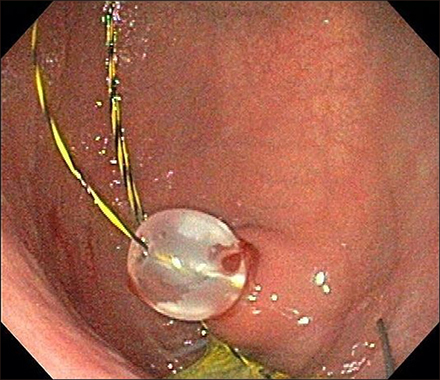
Wire Guided Cannulation Facilitates Endoscopic Management of Buried Bumper Syndrome: A Novel Technique
- Affiliations
-
- 1Department of Pediatric Anesthesia, Johns Hopkins All Children's Hospital, St. Petersburg, United States. jeepeck@gmail.com
- 2Department of Pediatrics, University of South Florida Morsani College of Medicine, Tampa, United States.
- 3Undergraduate Education, State University, Tallahassee, United States.
- 4Division of Pediatric Gastroenterology, Hepatology and Nutrition, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States.
- KMID: 2430920
- DOI: http://doi.org/10.5223/pghn.2019.22.1.86
Abstract
- Buried bumper syndrome is a rare but potentially severe complication of percutaneous endoscopic gastrostomy tube insertion. Though this complication is uncommon, it may lead to pressure necrosis, bleeding, perforation, peritonitis, sepsis, or death. Each case of buried bumper syndrome is unique in terms of patient comorbidities and anatomic positioning of the buried bumper. For this reason, many approaches have been described in the management of buried bumper syndrome. In this case report, we describe the case of an adolescent Caucasian female who developed buried bumper syndrome three years after undergoing percutaneous endoscopic gastrostomy insertion. We review diagnosis and management of buried bumper syndrome and describe a novel technique for bumper removal in which we use a guide wire in combination with external traction to maintain a patent gastrostomy lumen while removing the internal percutaneous endoscopic gastrostomy bumper.
Keyword
MeSH Terms
Figure
Reference
-
1. Cyrany J, Rejchrt S, Kopacova M, Bures J. Buried bumper syndrome: A complication of percutaneous endoscopic gastrostomy. World J Gastroenterol. 2016; 22:618–627.
Article2. Afifi I, Zarour A, Al-Hassani A, Peralta R, El-Menyar A, Al-Thani H. The challenging buried bumper syndrome after percutaneous endoscopic gastrostomy. Case Rep Gastroenterol. 2016; 10:224–232.
Article3. Stewart CE, Mutalib M, Pradhan A, Bassett C, Drake D, Upadhyaya M. Short article: Buried bumper syndrome in children: incidence and risk factors. Eur J Gastroenterol Hepatol. 2017; 29:181–184.4. Benatta MA. The buried bumper syndrome: external bumper extraction after radial mini incisions and replacement through an adjacent tract. Case Rep Med. 2016; 2016:5379291.
Article5. Mueller-Gerbes D, Hartmann B, Lima JP, de Lemos Bonotto M, Merbach C, Dormann A, et al. Comparison of removal techniques in the management of buried bumper syndrome: a retrospective cohort study of 82 patients. Endosc Int Open. 2017; 5:E603–E607.
Article6. Christiaens P, Bossuyt P, Cuyle PJ, Moons V, Van Olmen A. Buried bumper syndrome: single-step endoscopic management and replacement. Gastrointest Endosc. 2014; 80:336.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Buried Bumper Syndrome; A case report
- Two cases of buried bumper syndrome after percutaneous endoscopic gastrostomy
- Two Cases of Early Onset Acute Buried Bumper Syndrome after Percutaneous Endoscopic Gastrostomy
- A Case of Buried Bumper Syndrome
- A Case of Buried Bumper Syndrome Complicated by Abdominal Wall Abscess in an Elderly Patient