Left Ventricular End-Systolic Volume Can Predict 1-Year Hierarchical Clinical Composite End Point in Patients with Cardiac Resynchronization Therapy
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. smkang@yuhs.ac, cby6908@yuhs.ac
- 2Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2428277
- DOI: http://doi.org/10.3349/ymj.2019.60.1.48
Abstract
- PURPOSE
This study aimed to elucidate which echocardiographic criteria at three time points, for cardiac resynchronization therapy (CRT) response, are accurate in discriminating the hierarchical clinical composite end point (HCCEP).
MATERIALS AND METHODS
We included 120 patients (age, 66.1±12.6 years; men, 54.2%) who underwent CRT implantation for heart failure (HF). Echocardiography was performed before and at 3, 6, and 12 months after CRT implantation. The 1-year HCCEP included all-cause mortality, hospitalization for HF, and New York Heart Association functional class for 12 months. CRT response criteria were decrease in left ventricular (LV) end-systolic volume (LVESV) >15%, decrease in LV end-diastolic volume >15%, absolute increase in LV ejection fraction (LVEF) ≥5%, relative increase in LVEF ≥15%, and decrease in mitral regurgitation ≥1 grade. Temporal changes in CRT response rates, accuracy of CRT response criteria at each time and cutoff value for the discrimination of improvement in HCCEP, and agreements with improvement in HCCEP were analyzed.
RESULTS
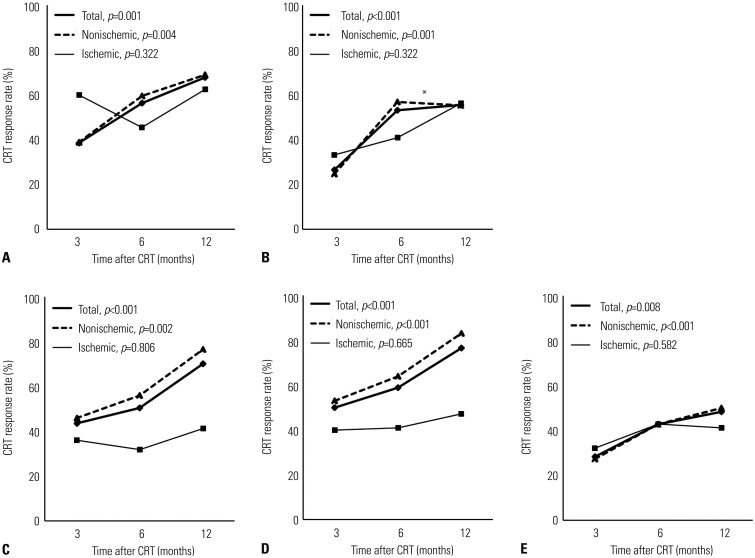
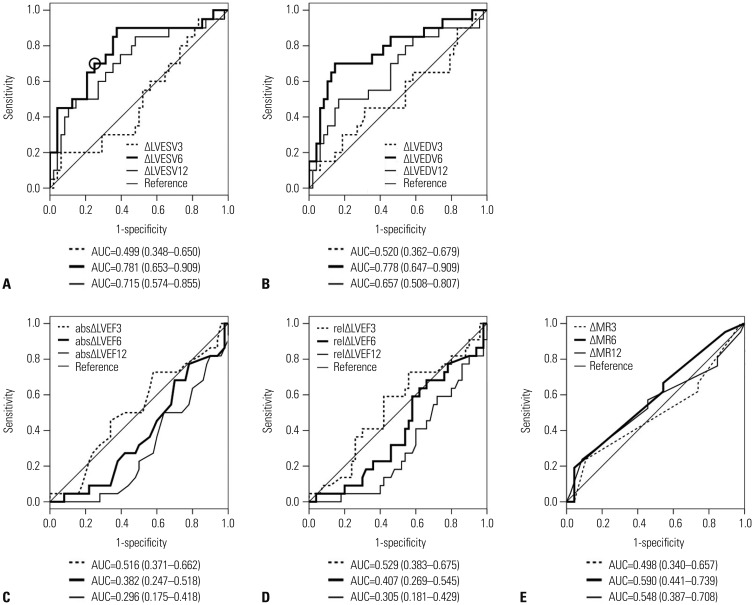
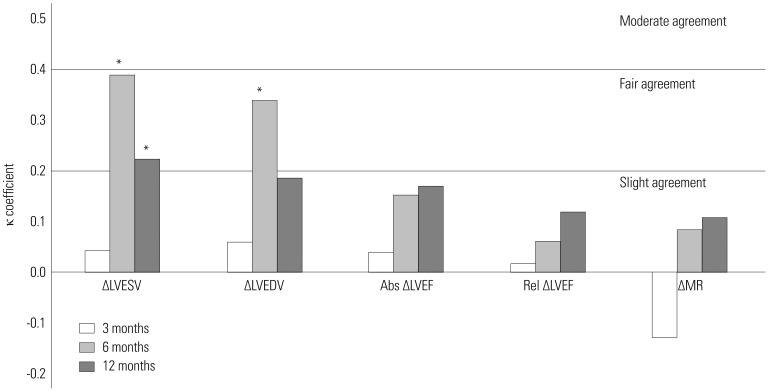
HCCEP improvement rates were 65.8% in total group. In nonischemic group, CRT response rates according to all echocardiographic criteria significantly increased with time. In ischemic group, CRT response rate did not significantly change with time. In total group, ΔLVESV at 6 months (ΔLVESV6) had the most significant accuracy for the discrimination of HCCEP (area under the curve=0.781). The optimal cutoff value of ΔLVESV6 was 13.5% (sensitivity=0.719, specificity=0.719). ΔLVESV6 had fair agreement with HCCEP (κ=0.391, p < 0.001).
CONCLUSION
ΔLVESV6 is the most useful echocardiographic CRT response criterion for the prediction of 1-year HCCEP.
MeSH Terms
Figure
Cited by 3 articles
-
The Past, Present and Future of Cardiac Resynchronization Therapy
Thomas O'Brien, Myung-Soo Park, Jong-Chan Youn, Eugene S. Chung
Korean Circ J. 2019;49(5):384-399. doi: 10.4070/kcj.2019.0114.Temporal Trends of Cardiac Implantable Electronic Device Implantations: a Nationwide Population-based Study
Ji Hyun Lee, So-Ryoung Lee, Eue-Keun Choi, Jaehan Jeong, Hyung-Deuk Park, So-Jeong You, Sang-Soo Lee, Seil Oh
Korean Circ J. 2019;49(9):841-852. doi: 10.4070/kcj.2018.0444.Korean Society of Heart Failure Guidelines for the Management of Heart Failure: Treatment
Jong-Chan Youn, Darae Kim, Jae Yeong Cho, Dong-Hyuk Cho, Sang Min Park, Mi-Hyang Jung, Junho Hyun, Hyun-Jai Cho, Seong-Mi Park, Jin-Oh Choi, Wook-Jin Chung, Byung-Su Yoo, Seok-Min Kang,
Korean Circ J. 2023;53(4):217-238. doi: 10.4070/kcj.2023.0047.
Reference
-
1. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37:2129–2200. PMID: 27206819.2. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017; 136:e137–e161. PMID: 28455343.
Article3. Packer M. Development and evolution of a hierarchical clinical composite end point for the evaluation of drugs and devices for acute and chronic heart failure: a 20-year perspective. Circulation. 2016; 134:1664–1678. PMID: 27881506.4. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802. PMID: 12835667.
Article5. Bleeker GB, Bax JJ, Fung JW, van der, Zhang Q, Schalij MJ, et al. Clinical versus echocardiographic parameters to assess response to cardiac resynchronization therapy. Am J Cardiol. 2006; 97:260–263. PMID: 16442375.
Article6. Chung ES, Leon AR, Tavazzi L, Sun JP, Nihoyannopoulos P, Merlino J, et al. Results of the predictors of response to CRT (PROSPECT) trial. Circulation. 2008; 117:2608–2616. PMID: 18458170.
Article7. Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009; 361:1329–1338. PMID: 19723701.
Article8. Bax JJ, Marwick TH, Molhoek SG, Bleeker GB, van Erven L, Boersma E, et al. Left ventricular dyssynchrony predicts benefit of cardiac resynchronization therapy in patients with end-stage heart failure before pacemaker implantation. Am J Cardiol. 2003; 92:1238–1240. PMID: 14609610.
Article9. Gorcsan J 3rd, Tanabe M, Bleeker GB, Suffoletto MS, Thomas NC, Saba S, et al. Combined longitudinal and radial dyssynchrony predicts ventricular response after resynchronization therapy. J Am Coll Cardiol. 2007; 50:1476–1483. PMID: 17919568.
Article10. Suffoletto MS, Dohi K, Cannesson M, Saba S, Gorcsan J 3rd. Novel speckle-tracking radial strain from routine black-and-white echocardiographic images to quantify dyssynchrony and predict response to cardiac resynchronization therapy. Circulation. 2006; 113:960–968. PMID: 16476850.
Article11. Achilli A, Peraldo C, Sassara M, Orazi S, Bianchi S, Laurenzi F, et al. Prediction of response to cardiac resynchronization therapy: the selection of candidates for CRT (SCART) study. Pacing Clin Electrophysiol. 2006; 29(Suppl 2):S11–S19. PMID: 17169127.
Article12. Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002; 346:1845–1853. PMID: 12063368.
Article13. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID: 843571.
Article14. Li K, Qian Z, Hou X, Wang Y, Qiu Y, Sheng Y, et al. The incidence and outcomes of delayed response to cardiac resynchronization therapy. Pacing Clin Electrophysiol. 2018; 41:73–80. PMID: 29222875.
Article15. Marsan NA, Bleeker GB, van Bommel RJ, Ypenburg C, Delgado V, Borleffs CJ, et al. Comparison of time course of response to cardiac resynchronization therapy in patients with ischemic versus nonischemic cardiomyopathy. Am J Cardiol. 2009; 103:690–694. PMID: 19231335.
Article16. Viveiros Monteiro A, Martins Oliveira M, Silva Cunha P, Nogueira da Silva M, Feliciano J, Branco L, et al. Time to left ventricular reverse remodeling after cardiac resynchronization therapy: Better late than never. Rev Port Cardiol. 2016; 35:161–167. PMID: 26923367.
Article17. Higgins SL, Hummel JD, Niazi IK, Giudici MC, Worley SJ, Saxon LA, et al. Cardiac resynchronization therapy for the treatment of heart failure in patients with intraventricular conduction delay and malignant ventricular tachyarrhythmias. J Am Coll Cardiol. 2003; 42:1454–1459. PMID: 14563591.
Article18. Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N Engl J Med. 2004; 350:2140–2150. PMID: 15152059.
Article19. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D, Kappenberger L, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005; 352:1539–1549. PMID: 15753115.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Left and Right Ventricular Volume and Cardiac Output by MRI and Echocardiography
- Comparison between Echocardiography and Cardiac Cine-MRI : Left Ventricular Volume and Cardiac Output
- Implantable Cardioverter-Defibrillator and Cardiac Resynchronization Therapy
- Rapid and Potent Antiarrhythmic Effect of Cardiac Resynchronization Therapy in a Patient with Advanced Dilated Cardiomyopathy and a Large Ventricular Arrhythmia Burden
- Successful Placement of a Left Ventricular Pacing Lead Despite Coronary Sinus Dissection During Cardiac Resynchronization Therapy