J Korean Neurosurg Soc.
2018 Nov;61(6):731-736. 10.3340/jkns.2016.1212.001.
Conus Medullaris Levels on Ultrasonography in Term Newborns : Normal Levels and Dermatological Findings
- Affiliations
-
- 1Departmant of Radiology, Sakarya University Training and Research Hospital, Sakarya, Turkey.
- 2Departmant of Dermatology, Sakarya University Training and Research Hospital, Sakarya, Turkey. drcanyaldiz@yahoo.com
- KMID: 2428115
- DOI: http://doi.org/10.3340/jkns.2016.1212.001
Abstract
OBJECTIVE
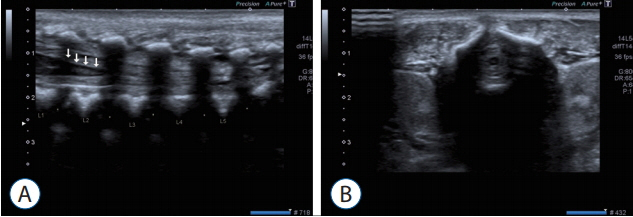
Ultrasonography (US) is the most non-invasive, safe, and, especially in the period of infancy, best method for visualizing and examining the spinal cord. Furthermore, US is the primary work-up for development of the spinal canal, and for follow-up on issues relating to subcutaneous tissues, bone development, and the spinal cord. Conus medullaris terminates at the second lumbar vertebra, according to a consensus in the literature.
METHODS
Healthy children under the age of 6 months who were admitted to the radiology clinic for routine USG follow-ups between the dates of March 2012 to December 2014 were included in this study.
RESULTS
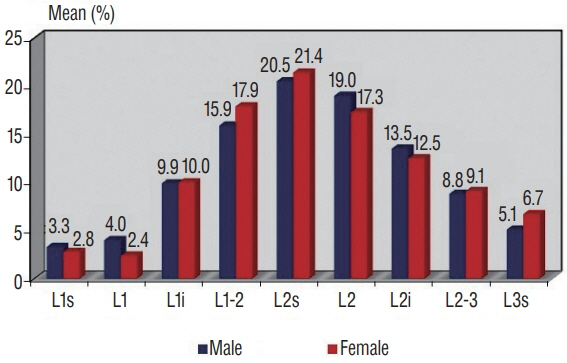
Our study includes data from 1125 lumbosacral ultrasounds. The terminal point of the conus level of the attended infants, superior, middle part, inferior of the vertebrae L1, L2, and L3. Furthermore, the termination of the discal distance ratio did not differ significantly between genders.
CONCLUSION
Therefore, according to our results, gender is not an influencing factor in the termination of the spinal cord. Based on the study we performed, as well as the previous literature, in infants without a recognized spinal pathology, the spinal cord is detected below the vertebra L3.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Arthurs OJ, Thayyil S, Wade A, Chong WK, Sebire NJ, Taylor AM; Magnetic Resonance Imaging Autopsy Study Collaborative Group. Normal ascent of the conus medullaris: a post-mortem foetal MRI study. J Matern Fetal Neonatal Med. 26:697–702. 2013.
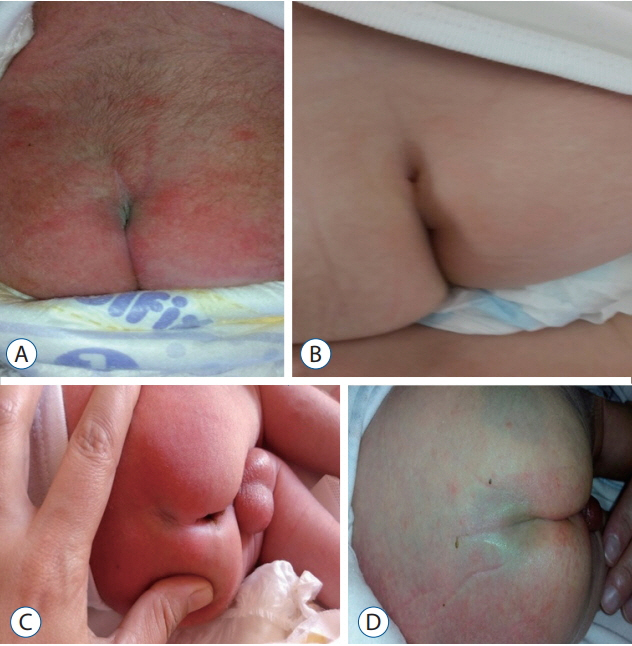
Article2. Değirmenci S, Güven F, Celayir A, Kılıç BD, Say A. Lumbosakral orta hat cilt lezyonlu yenidoğanlarda spinal kord anomalileri Orijinal Araştırma. Türk Pediatri Arşivi. 38:103–106. 2003.3. Ferahbas A, Utas S, Akcakus M, Gunes T, Mistik S. Prevalence of cutaneous findings in hospitalized neonates: a prospective observational study. Pediatr Dermatol. 26:139–142. 2009.
Article4. Gokdemir G, Erdogan HK, Köşlü A, Baksu B. Cutaneous lesions in Turkish neonates born in a teaching hospital. Indian J Dermatol Venereol Leprol. 75:638. 2009.
Article5. Henriques JG, Pianetti G, Henriques KS, Costa P, Gusmão S. Minor skin lesions as markers of occult spinal dysraphisms--prospective study. Surg Neurol. 63:8–12. 2005.
Article6. Hill CA, Gibson PJ. Ultrasound determination of the normal location of the conus medullaris in neonates. AJNR Am J Neuroradiol. 16:469–472. 1995.7. Monteagudo B, Labandeira J, León-Muiños E, Carballeira I, Cabanillas M, Suárez-Amor O. Frequency of birthmarks and transient skin lesions in newborns according to maternal factors (diseases, drugs, dietary supplements, and tobacco). Indian J Dermatol Venereol Leprol. 77:535. 2011.
Article8. Moosavi Z, Hosseini T. One-year survey of cutaneous lesions in 1000 consecutive Iranian newborns. Pediatr Dermatol. 23:61–63. 2006.
Article9. Perlitz Y, Izhaki I, Ben-Ami M. Sonographic evaluation of the fetal conus medullaris at 20 to 24 weeks' gestation. Prenat Diagn. 30:862–864. 2010.
Article10. Rozzelle CJ, Reed GT, Kirkman JL, Shannon CN, Chern JJ, Wellons JC 3rd, et al. Sonographic determination of normal Conus Medullaris level and ascent in early infancy. Childs Nerv Syst. 30:655–658. 2014.
Article11. Sahin F, Selçuki M, Ecin N, Zenciroğlu A, Unlü A, Yilmaz F, et al. Level of conus medullaris in term and preterm neonates. Arch Dis Child Fetal Neonatal Ed. 77:F67–F69. 1997.
Article12. Sarıkaya Solak S, Tükenmez Demirci G, Kıvanç Altunay I, Küçükünal A. The relationship of birthmarks observed in 1000 newborns with neonatal/maternal parameters: a prospective and cross-sectional study. Turkiye Klinikleri J Med Sci. 33:1388–1394. 2013.
Article13. Shih IH, Lin JY, Chen CH, Hong HS. A birthmark survey in 500 newborns: clinical observation in two northern Taiwan medical center nurseries. Chang Gung Med J. 30:220–225. 2007.14. Vettivel S. Vertebral level of termination of the spinal cord in human fetuses. J Anat. 179:149–161. 1991.15. Warder DE. Tethered cord syndrome and occult spinal dysraphism. Neurosurg Focus. 10:e1. 2001.
Article16. Warder DE, Oakes WJ. Tethered cord syndrome and the conus in a normal position. Neurosurgery. 33:374–378. 1993.
Article17. Warder DE, Oakes WJ. Tethered cord syndrome: the low-lying and normally positioned conus. Neurosurg. 34:597–600. discussion 600. 1994.18. Wilson DA, Prince JR. John Caffey award. MR ımaging determination of the location of the normal conus medullaris throughout childhood. AJR Am J Radiol. 152:1029–1032. 1989.
Article19. Yamada S, Zinke DE, Sanders D. Pathophysiology of “tethered cord syndrome”. J Neurosurg. 54:494–503. 1981.
Article20. Zalel Y, Lehavi O, Aizenstein O, Achiron R. Development of the fetal spinal cord: time of ascendance of the normal conus medullaris as detected bysonography. J Ultrasound Med. 25:1397–1401. 2006.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Conus Medullaris Hemangioblastoma
- Sonographic Determination of the Normal Location and Positional Change of the Conus Medullaris in Infants
- Magnetic Resonance Imaging Observations of the Conus Medullaris in a Korean Population
- Normal Variations of the Spinal Cord Termination
- Multiple Hemangioendotheliomas of the Spinal Cord and Cauda Equina: Case Report