J Pathol Transl Med.
2018 Nov;52(6):396-403. 10.4132/jptm.2018.10.03.
The Prognostic Impact of Synchronous Ipsilateral Multiple Breast Cancer: Survival Outcomes according to the Eighth American Joint Committee on Cancer Staging and Molecular Subtype
- Affiliations
-
- 1Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. eunyoon.cho@samsung.com, parmenides.kim@samsung.com
- KMID: 2427522
- DOI: http://doi.org/10.4132/jptm.2018.10.03
Abstract
- BACKGROUND
In the current American Joint Committee on Cancer staging system of breast cancer, only tumor size determines T-category regardless of whether the tumor is single or multiple. This study evaluated if tumor multiplicity has prognostic value and can be used to subclassify breast cancer.
METHODS
We included 5,758 patients with invasive breast cancer who underwent surgery at Samsung Medical Center, Seoul, Korea, from 1995 to 2012.
RESULTS
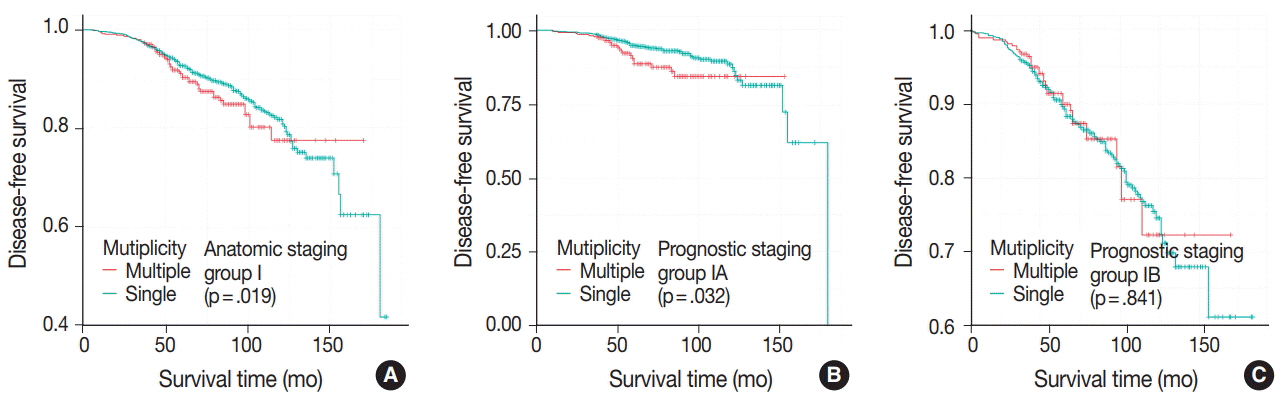
Patients were divided into two groups according to multiplicity (single, n = 4,744; multiple, n = 1,014). Statistically significant differences in lymph node involvement and lymphatic invasion were found between the two groups (p < .001). Patients with multiple masses tended to have luminal A molecular subtype (p < .001). On Kaplan-Meier survival analysis, patients with multiple masses had significantly poorer disease-free survival (DFS) (p = .016). The prognostic significance of multiplicity was seen in patients with anatomic staging group I and prognostic staging group IA (p = .019 and p = .032, respectively). When targeting patients with T1-2 N0 M0, hormone receptor-positive, and human epidermal growth factor receptor 2 (HER2)-negative cancer, Kaplan-Meier survival analysis also revealed significantly reduced DFS with multiple cancer (p = .031). The multivariate analysis indicated that multiplicity was independently correlated with worse DFS (hazard ratio, 1.23; 95% confidence interval, 1.03 to 1.47; p = .025). The results of this study indicate that tumor multiplicity is frequently found in luminal A subtype, is associated with frequent lymph node metastasis, and is correlated with worse DFS.
CONCLUSIONS
Tumor multiplicity has prognostic value and could be used to subclassify invasive breast cancer at early stages. Adjuvant chemotherapy would be necessary for multiple masses of T1-2 N0 M0, hormone-receptor-positive, and HER2-negative cancer.
MeSH Terms
Figure
Reference
-
1. Qualheim RE, Gall EA. Breast carcinoma with multiple sites of origin. Cancer. 1957; 10:460–8.
Article2. Bendifallah S, Werkoff G, Borie-Moutafoff C, et al. Multiple synchronous (multifocal and multicentric) breast cancer: clinical implications. Surg Oncol. 2010; 19:e115–23.
Article3. Yerushalmi R, Kennecke H, Woods R, Olivotto IA, Speers C, Gelmon KA. Does multicentric/multifocal breast cancer differ from unifocal breast cancer? An analysis of survival and contralateral breast cancer incidence. Breast Cancer Res Treat. 2009; 117:365–70.
Article4. Egan RL. Multicentric breast carcinomas: clinical-radiographicpathologic whole organ studies and 10-year survival. Cancer. 1982; 49:1123–30.5. Tot T. Axillary lymph node status in unifocal, multifocal, and diffuse breast carcinomas: differences are related to macrometastatic disease. Ann Surg Oncol. 2012; 19:3395–401.
Article6. Duraker N, Caynak ZC. Axillary lymph node status and prognosis in multifocal and multicentric breast carcinoma. Breast J. 2014; 20:61–8.
Article7. Cabioglu N, Ozmen V, Kaya H, et al. Increased lymph node positivity in multifocal and multicentric breast cancer. J Am Coll Surg. 2009; 208:67–74.
Article8. Andea AA, Bouwman D, Wallis T, Visscher DW. Correlation of tumor volume and surface area with lymph node status in patients with multifocal/multicentric breast carcinoma. Cancer. 2004; 100:20–7.
Article9. Joergensen LE, Gunnarsdottir KA, Lanng C, Moeller S, Rasmussen BB. Multifocality as a prognostic factor in breast cancer patients registered in Danish Breast Cancer Cooperative Group (DBCG) 1996-2001. Breast. 2008; 17:587–91.
Article10. Coombs NJ, Boyages J. Multifocal and multicentric breast cancer: does each focus matter? J Clin Oncol. 2005; 23:7497–502.
Article11. Vlastos G, Rubio IT, Mirza NQ, et al. Impact of multicentricity on clinical outcome in patients with T1-2, N0-1, M0 breast cancer. Ann Surg Oncol. 2000; 7:581–7.
Article12. Rezo A, Dahlstrom J, Shadbolt B, et al. Tumor size and survival in multicentric and multifocal breast cancer. Breast. 2011; 20:259–63.
Article13. Lynch SP, Lei X, Chavez-MacGregor M, et al. Multifocality and multicentricity in breast cancer and survival outcomes. Ann Oncol. 2012; 23:3063–9.
Article14. Pedersen L, Gunnarsdottir KA, Rasmussen BB, Moeller S, Lanng C. The prognostic influence of multifocality in breast cancer patients. Breast. 2004; 13:188–93.
Article15. Tot T, Gere M, Pekár G, et al. Breast cancer multifocality, disease extent, and survival. Hum Pathol. 2011; 42:1761–9.
Article16. Giuliano AE, Edge SB, Hortobagyi GN. Eighth edition of the AJCC cancer staging manual: breast cancer. Ann Surg Oncol. 2018; 25:1783–5.
Article17. Hammond ME, Hayes DF, Dowsett M, et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010; 28:2784–95.
Article18. Wolff AC, Hammond ME, Hicks DG, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. Arch Pathol Lab Med. 2014; 138:241–56.19. Goldhirsch A, Wood WC, Coates AS, et al. Strategies for subtypes: dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011; 22:1736–47.20. Litton JK, Eralp Y, Gonzalez-Angulo AM, et al. Multifocal breast cancer in women < or =35 years old. Cancer. 2007; 110:1445–50.21. Boyages J, Jayasinghe UW, Coombs N. Multifocal breast cancer and survival: each focus does matter particularly for larger tumours. Eur J Cancer. 2010; 46:1990–6.
Article22. Neri A, Marrelli D, Megha T, et al. “Clinical significance of multifocal and multicentric breast cancers and choice of surgical treatment: a retrospective study on a series of 1158 cases”. BMC Surg. 2015; 15:1.
Article23. O’Daly BJ, Sweeney KJ, Ridgway PF, et al. The accuracy of combined versus largest diameter in staging multifocal breast cancer. J Am Coll Surg. 2007; 204:282–5.
Article24. Weissenbacher TM, Zschage M, Janni W, et al. Multicentric and multifocal versus unifocal breast cancer: is the tumor-node-metastasis classification justified? Breast Cancer Res Treat. 2010; 122:27–34.
Article25. Ustaalioglu BO, Bilici A, Kefeli U, et al. The importance of multifocal/multicentric tumor on the disease-free survival of breast cancer patients: single center experience. Am J Clin Oncol. 2012; 35:580–6.26. Fish EB, Chapman JA, Link MA. Assessment of tumor size for multifocal primary breast cancer. Ann Surg Oncol. 1998; 5:442–6.
Article27. Moon HG, Han W, Kim JY, et al. Effect of multiple invasive foci on breast cancer outcomes according to the molecular subtypes: a report from the Korean Breast Cancer Society. Ann Oncol. 2013; 24:2298–304.
Article28. Sparano JA, Gray RJ, Makower DF, et al. Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med. 2015; 373:2005–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of an Excel Program for the Updated Eighth American Joint Committee on Cancer Breast Cancer Staging System
- Assessment of the Prognostic Staging System of American Joint Committee on Cancer 8th Edition for Breast Cancer: Comparisons with the Conventional Anatomic Staging System
- TNM Staging, Molecular Staging and Prognostic Factors of Rectal Cancer
- Prognostic Validation of the American Joint Committee on Cancer 8th Staging System in 24,014 Korean Patients with Breast Cancer
- Esophageal Cancer Staging