Korean J Radiol.
2017 Dec;18(6):946-956. 10.3348/kjr.2017.18.6.946.
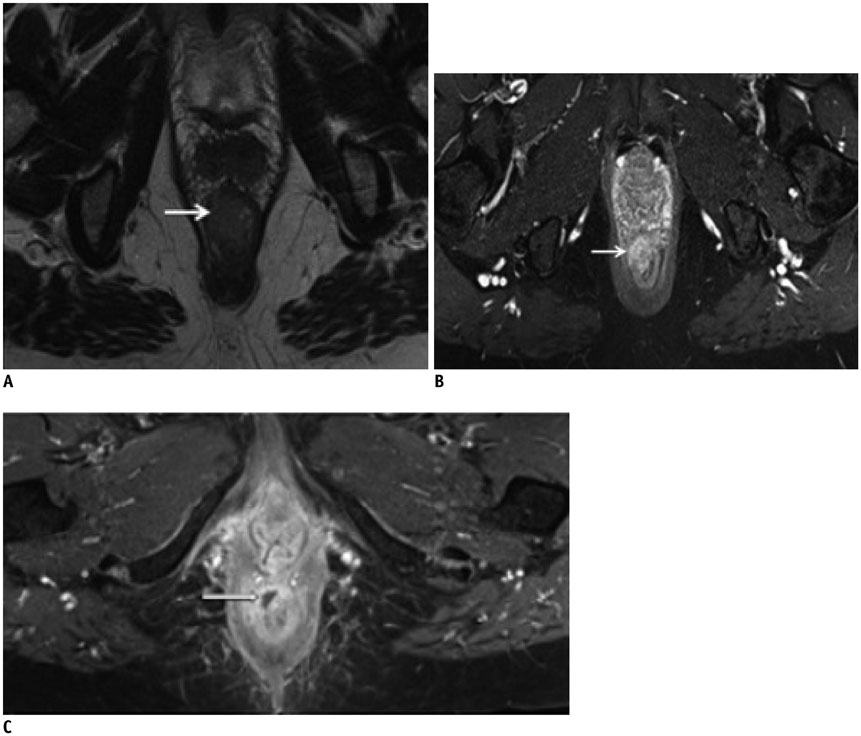
Cancer of the Anal Canal: Diagnosis, Staging and Follow-Up with MRI
- Affiliations
-
- 1Department of Radiology, Centre Hospitalo-Universitaire de Reims, Reims 51092, France. carole_durot@hotmail.fr
- 2Department of Abdominal Imaging, Hôpital Lariboisière-APHP, Paris 75010, France.
- 3Department of Radiology and Nuclear Medicine, Institut Curie, Paris 75005, France.
- 4CRESTIC, Reims Champagne-Ardenne University, Reims 51867, France.
- KMID: 2427204
- DOI: http://doi.org/10.3348/kjr.2017.18.6.946
Abstract
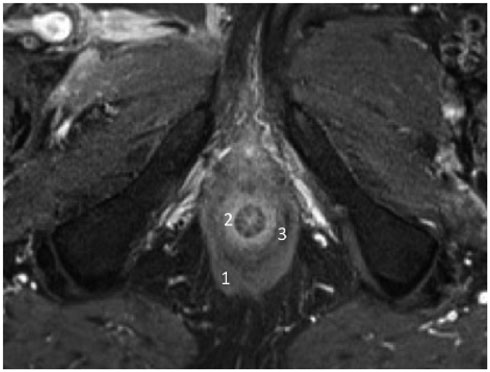
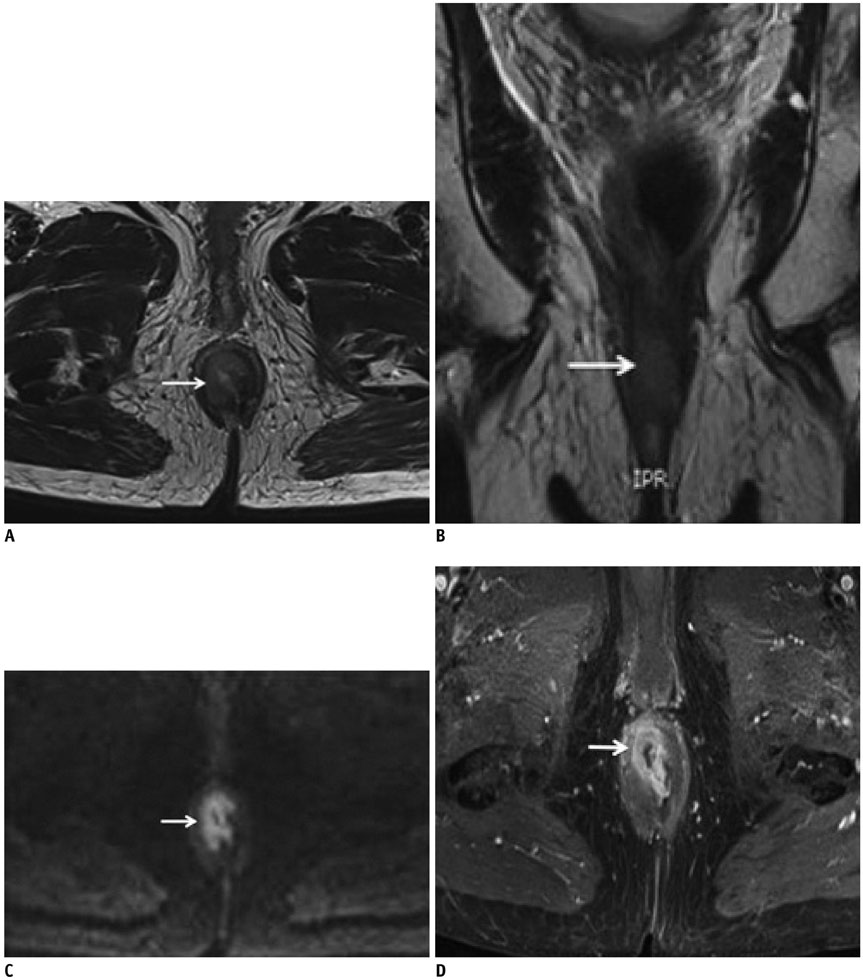
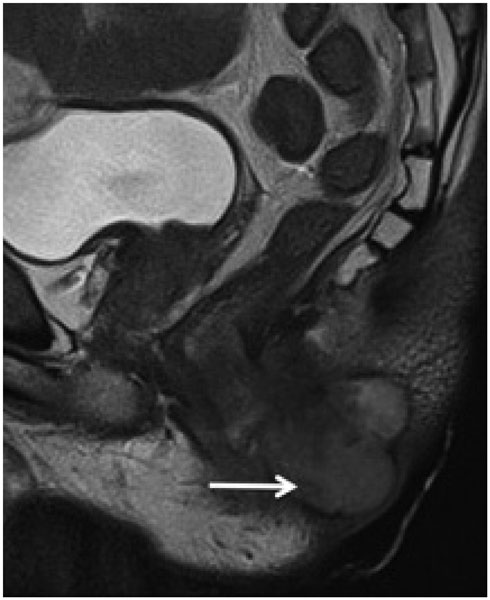
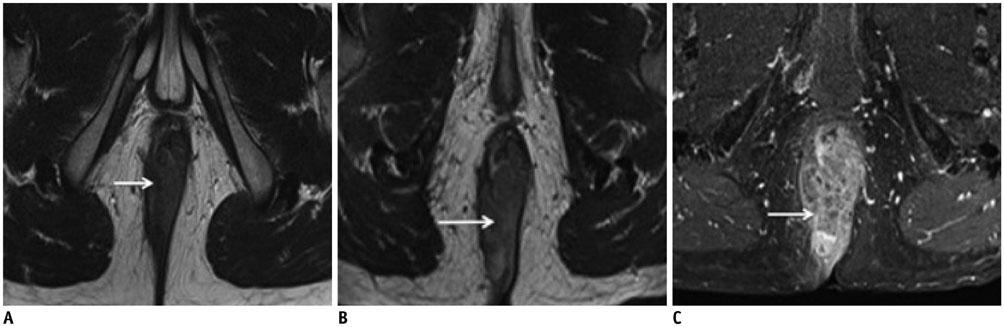
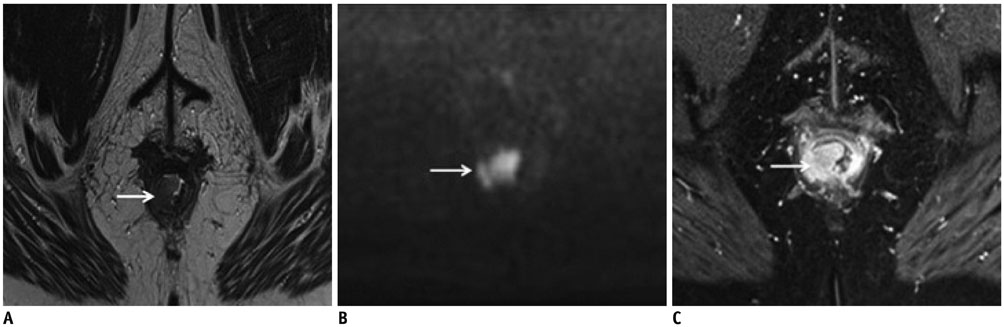
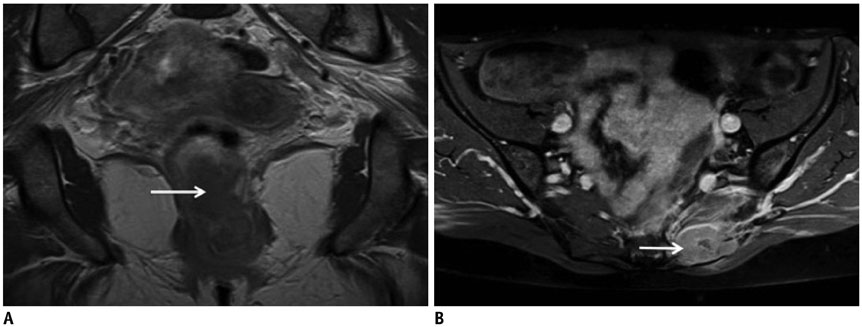
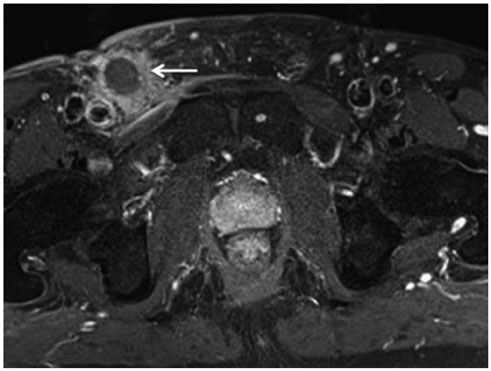
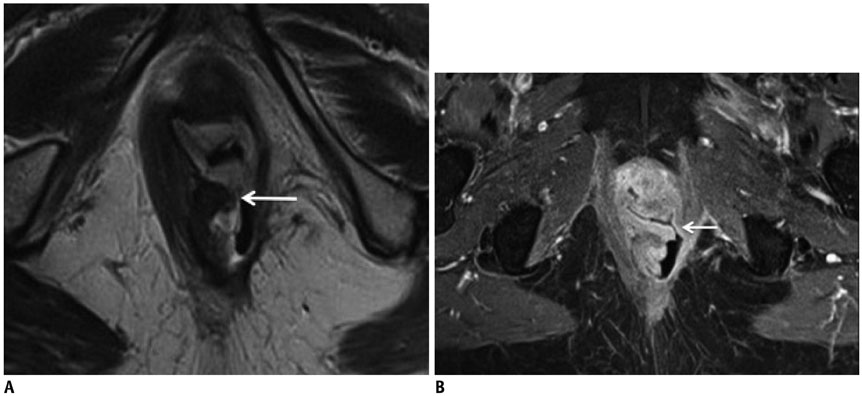
- Although a rare disease, anal cancer is increasingly being diagnosed in patients with risk factors, mainly anal infection with the human papilloma virus. Magnetic resonance imaging (MRI) with external phased-array coils is recommended as the imaging modality of choice to grade anal cancers and to evaluate the response assessment after chemoradiotherapy, with a high contrast and good anatomic resolution of the anal canal. MRI provides a performant evaluation of size, extent and signal characteristics of the anal tumor before and after treatment, as well as lymph node involvement and extension to the adjacent organs. MRI is also particularly helpful in the assessment of complications after treatment, and in the diagnosis for relapse of the diseases.
Keyword
MeSH Terms
-
Aged
Anal Canal/anatomy & histology/*diagnostic imaging/pathology
Antimetabolites, Antineoplastic/therapeutic use
Anus Neoplasms/*diagnosis/diagnostic imaging/pathology/therapy
Female
Fluorouracil/therapeutic use
Follow-Up Studies
Humans
*Magnetic Resonance Imaging
Male
Middle Aged
Neoplasm Recurrence, Local
Neoplasm Staging
Positron Emission Tomography Computed Tomography
Radiation, Ionizing
Tomography, X-Ray Computed
Antimetabolites, Antineoplastic
Fluorouracil
Figure
Reference
-
1. American Joint Committee on Cancer. AJCC cancer staging manual. 7th ed. New York: Springer;2010. p. 103–106.2. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010; 60:277–300.3. Johnson LG, Madeleine MM, Newcomer LM, Schwartz SM, Daling JR. Anal cancer incidence and survival: the surveillance, epidemiology, and end results experience, 1973-2000. Cancer. 2004; 101:281–288.4. Uronis HE, Bendell JC. Anal cancer: an overview. Oncologist. 2007; 12:524–534.5. Hoots BE, Palefsky JM, Pimenta JM, Smith JS. Human papillomavirus type distribution in anal cancer and anal intraepithelial lesions. Int J Cancer. 2009; 124:2375–2383.6. Barral M, Dohan A, Allez M, Boudiaf M, Camus M, Laurent V, et al. Gastrointestinal cancers in inflammatory bowel disease: an update with emphasis on imaging findings. Crit Rev Oncol Hematol. 2016; 97:30–46.7. Epidermoid anal cancer: results from the UKCCCR randomised trial of radiotherapy alone versus radiotherapy, 5-fluorouracil, and mitomycin. UKCCCR Anal Cancer Trial Working Party. UK Co-ordinating Committee on Cancer Research. Lancet. 1996; 348:1049–1054.8. Peiffert D, Tournier-Rangeard L, Gérard JP, Lemanski C, François E, Giovannini M, et al. Induction chemotherapy and dose intensification of the radiation boost in locally advanced anal canal carcinoma: final analysis of the randomized UNICANCER ACCORD 03 trial. J Clin Oncol. 2012; 30:1941–1948.9. Ajani JA, Winter KA, Gunderson LL, Pedersen J, Benson AB 3rd, Thomas CR Jr, et al. Fluorouracil, mitomycin, and radiotherapy vs fluorouracil, cisplatin, and radiotherapy for carcinoma of the anal canal: a randomized controlled trial. JAMA. 2008; 299:1914–1921.10. Flam M, John M, Pajak TF, Petrelli N, Myerson R, Doggett S, et al. Role of mitomycin in combination with fluorouracil and radiotherapy, and of salvage chemoradiation in the definitive nonsurgical treatment of epidermoid carcinoma of the anal canal: results of a phase III randomized intergroup study. J Clin Oncol. 1996; 14:2527–2539.11. Bartelink H, Roelofsen F, Eschwege F, Rougier P, Bosset JF, Gonzalez DG, et al. Concomitant radiotherapy and chemotherapy is superior to radiotherapy alone in the treatment of locally advanced anal cancer: results of a phase III randomized trial of the European Organization for Research and Treatment of Cancer Radiotherapy and Gastrointestinal Cooperative Groups. J Clin Oncol. 1997; 15:2040–2049.12. Sjödahl RI, Myrelid P, Söderholm JD. Anal and rectal cancer in Crohn's disease. Colorectal Dis. 2003; 5:490–495.13. Glynne-Jones R, Nilsson PJ, Aschele C, Goh V, Peiffert D, Cervantes A, et al. Anal cancer: ESMO-ESSO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014; 25:Suppl 3. iii10–iii20.14. Matalon SA, Mamon HJ, Fuchs CS, Doyle LA, Tirumani SH, Ramaiya NH, et al. Anorectal cancer: critical anatomic and staging distinctions that affect use of radiation therapy. Radiographics. 2015; 35:2090–2107.15. Jones M, Hruby G, Stanwell P, Gallagher S, Wong K, Arm J, et al. Multiparametric MRI as an outcome predictor for anal canal cancer managed with chemoradiotherapy. BMC Cancer. 2015; 15:281.16. Kochhar R, Renehan AG, Mullan D, Chakrabarty B, Saunders MP, Carrington BM. The assessment of local response using magnetic resonance imaging at 3- and 6-month post chemoradiotherapy in patients with anal cancer. Eur Radiol. 2017; 27:607–617.17. Goh V, Gollub FK, Liaw J, Wellsted D, Przybytniak I, Padhani AR, et al. Magnetic resonance imaging assessment of squamous cell carcinoma of the anal canal before and after chemoradiation: can MRI predict for eventual clinical outcome? Int J Radiat Oncol Biol Phys. 2010; 78:715–721.18. Koh DM, Dzik-Jurasz A, O’Neill B, Tait D, Husband JE, Brown G. Pelvic phased-array MR imaging of anal carcinoma before and after chemoradiation. Br J Radiol. 2008; 81:91–98.19. Jederán É, Lõvey J, Szentirmai Z, Hitre E, Léránt G, Horváth K, et al. The role of MRI in the assessment of the local status of anal carcinomas and in their management. Pathol Oncol Res. 2015; 21:571–579.20. Beets-Tan RG, Lambregts DM, Maas M, Bipat S, Barbaro B, Caseiro-Alves F, et al. Magnetic resonance imaging for the clinical management of rectal cancer patients: recommendations from the 2012 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol. 2013; 23:2522–2531.21. Roach SC, Hulse PA, Moulding FJ, Wilson R, Carrington BM. Magnetic resonance imaging of anal cancer. Clin Radiol. 2005; 60:1111–1119.22. Gourtsoyianni S, Goh V. MRI of anal cancer: assessing response to definitive chemoradiotherapy. Abdom Imaging. 2014; 39:2–17.23. Kochhar R, Plumb AA, Carrington BM, Saunders M. Imaging of anal carcinoma. AJR Am J Roentgenol. 2012; 199:W335–W344.24. Cotter SE, Grigsby PW, Siegel BA, Dehdashti F, Malyapa RS, Fleshman JW, et al. FDG-PET/CT in the evaluation of anal carcinoma. Int J Radiat Oncol Biol Phys. 2006; 65:720–725.25. Mistrangelo M, Pelosi E, Bellò M, Ricardi U, Milanesi E, Cassoni P, et al. Role of positron emission tomography-computed tomography in the management of anal cancer. Int J Radiat Oncol Biol Phys. 2012; 84:66–72.26. Winton Ed, Heriot AG, Ng M, Hicks RJ, Hogg A, Milner A, et al. The impact of 18-fluorodeoxyglucose positron emission tomography on the staging, management and outcome of anal cancer. Br J Cancer. 2009; 100:693–700.27. Brierley JD, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. 8th ed. Toronto: Wiley Blackwell;2016. p. 77.28. Otto SD, Lee L, Buhr HJ, Frericks B, Höcht S, Kroesen AJ. Staging anal cancer: prospective comparison of transanal endoscopic ultrasound and magnetic resonance imaging. J Gastrointest Surg. 2009; 13:1292–1298.29. Parikh J, Shaw A, Grant LA, Schizas AM, Datta V, Williams AB, et al. Anal carcinomas: the role of endoanal ultrasound and magnetic resonance imaging in staging, response evaluation and follow-up. Eur Radiol. 2011; 21:776–785.30. Hama Y, Makita K, Yamana T, Dodanuki K. Mucinous adenocarcinoma arising from fistula in ano: MRI findings. AJR Am J Roentgenol. 2006; 187:517–521.31. Singer M, Mutch MG. Anal melanoma. Clin Colon Rectal Surg. 2006; 19:78–87.32. Rousset P, Hoeffel C. [Tumors of the rectum: MRI and CT features]. J Radiol. 2007; 88(11 Pt 1):1679–1687.33. Benson AB 3rd, Arnoletti JP, Bekaii-Saab T, Chan E, Chen YJ, Choti MA, et al. Anal carcinoma, version 2.2012: featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2012; 10:449–454.34. Steele SR, Varma MG, Melton GB, Ross HM, Rafferty JF, Buie WD. Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for anal squamous neoplasms. Dis Colon Rectum. 2012; 55:735–749.35. Renehan AG, O’Dwyer ST. Management of local disease relapse. Colorectal Dis. 2011; 13:Suppl 1. 44–52.36. Borzomati D, Valeri S, Ripetti V, Vincenzi B, Rabitti C, Persichetti P, et al. Persisting perianal ulcer after radiotherapy for anal cancer: recurrence of disease or late radiation-related complication? Hepatogastroenterology. 2005; 52:780–784.37. Hoeffel C, Mulé S, Laurent V, Pierredon-Foulogne MA, Soyer P. Current imaging of rectal cancer. Clin Res Hepatol Gastroenterol. 2015; 39:168–173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Early-stage Squamous Cell Carcinoma of the Anal Canal Diagnosed by Endoscopic Mucosal Resection
- A Set of Monozygotic Female Twins With Anal Canal Duplication
- Transrectal ultrasonography of anorectal diseases: advantages and disadvantages
- Nonoperative chemoradiotherapy (FUMIR) for squamous cell carcinoma of the anal canal
- Anal Gland/Duct Cyst: A Case Report