Yonsei Med J.
2016 Nov;57(6):1339-1346. 10.3349/ymj.2016.57.6.1339.
Repolarization Heterogeneity of Magnetocardiography Predicts Long-Term Prognosis in Patients with Acute Myocardial Infarction
- Affiliations
-
- 1Cardiology Division, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- 2Department of Cardiology, University of Ulsan College of Medicine, Gangneung Asan Hospital, Gangneung, Korea.
- 3Bio-Signal Research Center, Korea Research Institute of Standards and Science, Daejeon, Korea.
- KMID: 2427150
- DOI: http://doi.org/10.3349/ymj.2016.57.6.1339
Abstract
- PURPOSE
Magnetocardiography (MCG) has been proposed as a noninvasive, diagnostic tool for risk-stratifying patients with acute myocardial infarction (AMI). This study evaluated whether MCG predicts long-term prognosis in AMI.
MATERIALS AND METHODS
In 124 AMI patients (95 males, mean age 60±11 years), including 39 with ST-elevation myocardial infarction, a 64-channel MCG was performed within 2 days after AMI. During a mean follow-up period of 6.1 years, major adverse cardiac events (MACE) were evaluated.
RESULTS
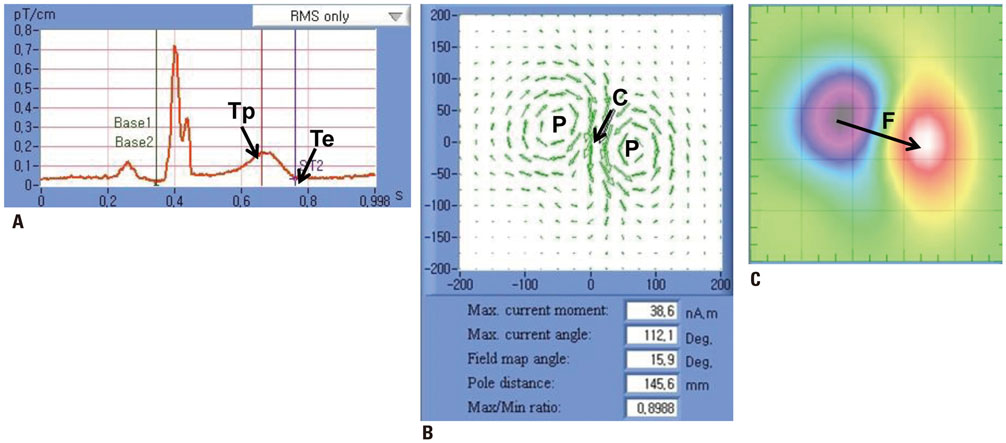
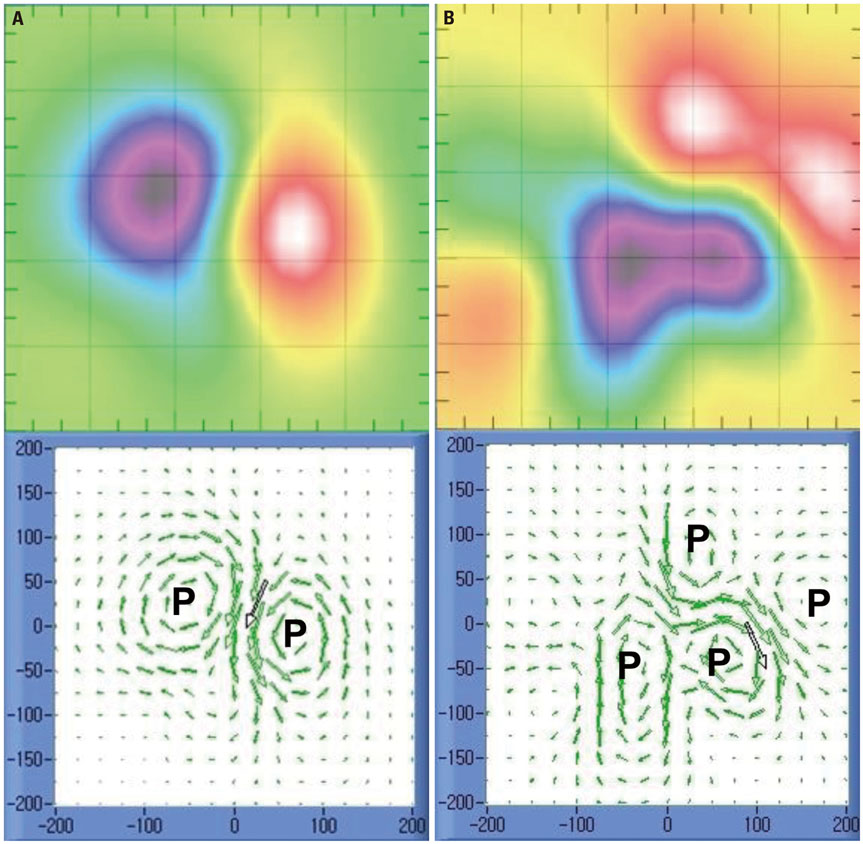
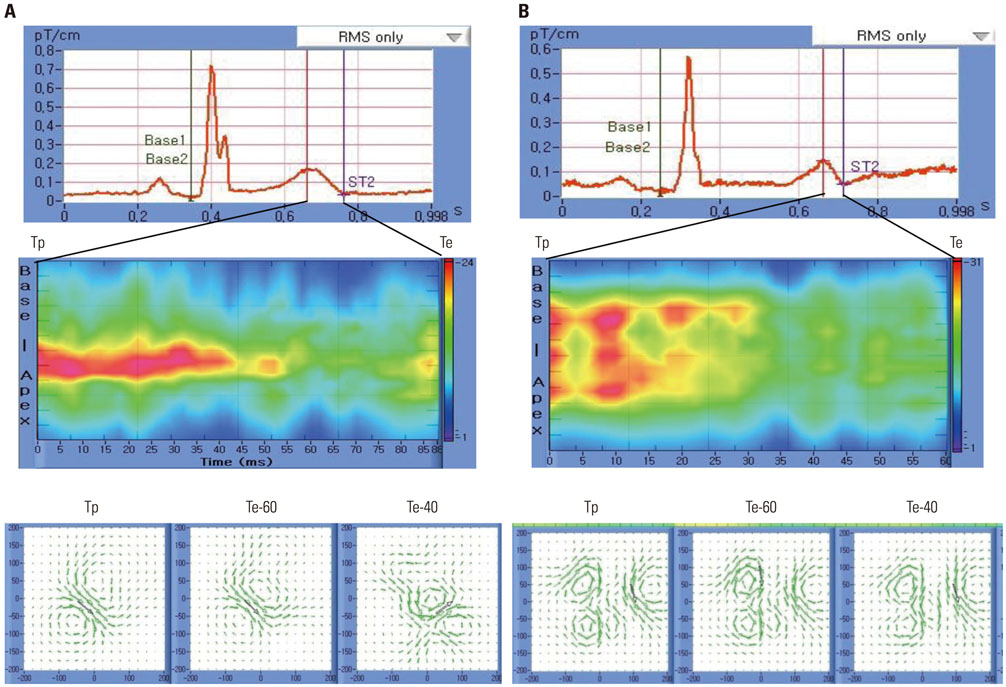
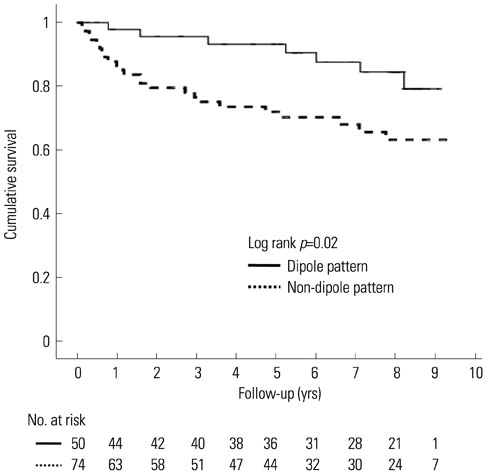
MACE occurred in 31 (25%) patients, including 20 revascularizations, 8 deaths, and 3 re-infarctions. Non-dipole patterns were observed at the end of the T wave in every patients. However, they were observed at T-peak in 77% (24/31) and 54% (50/93) of patients with and without MACE, respectively (p=0.03). Maximum current, field map angles, and distance dynamics were not different between groups. In the multivariate analysis, patients with non-dipole patterns at T-peak had increased age- and gender-adjusted hazard ratios for MACE (hazard ratio 2.89, 95% confidence interval 1.20-6.97, p=0.02) and lower cumulative MACE-free survival than those with dipole patterns (p=0.02).
CONCLUSION
Non-dipole patterns at T-peak were more frequently observed in patients with MACE and were related to poor long-term prognosis. Thus, repolarization heterogeneity measured by MCG may be a useful predictor for AMI prognosis.
MeSH Terms
Figure
Cited by 1 articles
-
Repolarization Heterogeneity of Magnetocardiography Predicts Long-Term Prognosis in Patients with Acute Myocardial Infarction
Ae-Young Her, Jai-Wun Park
Yonsei Med J. 2016;57(6):1305-1306. doi: 10.3349/ymj.2016.57.6.1305.
Reference
-
1. Cannon CP, McCabe CH, Stone PH, Rogers WJ, Schactman M, Thompson BW, et al. The electrocardiogram predicts one-year outcome of patients with unstable angina and non-Q wave myocardial infarction: results of the TIMI III Registry ECG Ancillary Study. Thrombolysis in Myocardial Ischemia. J Am Coll Cardiol. 1997; 30:133–140.
Article2. Kleiman NS, Lakkis N, Cannon CP, Murphy SA, DiBattiste PM, Demopoulos LA, et al. Prospective analysis of creatine kinase muscle-brain fraction and comparison with troponin T to predict cardiac risk and benefit of an invasive strategy in patients with non-ST-elevation acute coronary syndromes. J Am Coll Cardiol. 2002; 40:1044–1050.
Article3. Morrow DA, Rifai N, Antman EM, Weiner DL, McCabe CH, Cannon CP, et al. C-reactive protein is a potent predictor of mortality independently of and in combination with troponin T in acute coronary syndromes: a TIMI 11A substudy. Thrombolysis in Myocardial Infarction. J Am Coll Cardiol. 1998; 31:1460–1465.
Article4. Gibson CM, Pinto DS, Murphy SA, Morrow DA, Hobbach HP, Wiviott SD, et al. Association of creatinine and creatinine clearance on presentation in acute myocardial infarction with subsequent mortality. J Am Coll Cardiol. 2003; 42:1535–1543.
Article5. Breithardt G, Borggrefe M, Fetsch T, Böcker D, Mäkijärvi M, Reinhardt L. Prognosis and risk stratification after myocardial infarction. Eur Heart J. 1995; 16:Suppl G. 10–19.
Article6. Fenici R, Brisinda D, Meloni AM. Clinical application of magnetocardiography. Expert Rev Mol Diagn. 2005; 5:291–313.
Article7. Kwong JS, Leithäuser B, Park JW, Yu CM. Diagnostic value of magnetocardiography in coronary artery disease and cardiac arrhythmias: a review of clinical data. Int J Cardiol. 2013; 167:1835–1842.
Article8. Endt P, Montonen J, Mäkijärvi M, Nenonen J, Steinhoff U, Trahms L, et al. Identification of post-myocardial infarction patients with ventricular tachycardia by time-domain intra-QRS analysis of signal-averaged electrocardiogram and magnetocardiogram. Med Biol Eng Comput. 2000; 38:659–665.
Article9. Lim HK, Chung N, Kim K, Ko YG, Kwon H, Lee YH, et al. Can magnetocardiography detect patients with non-ST-segment elevation myocardial infarction? Ann Med. 2007; 39:617–627.
Article10. Lim HK, Kwon H, Chung N, Ko YG, Kim JM, Kim IS, et al. Usefulness of magnetocardiogram to detect unstable angina pectoris and non-ST elevation myocardial infarction. Am J Cardiol. 2009; 103:448–454.
Article11. Van Leeuwen P, Hailer B, Beck A, Eiling G, Grönemeyer D. Changes in dipolar structure of cardiac magnetic field maps after ST elevation myocardial infarction. Ann Noninvasive Electrocardiol. 2011; 16:379–387.
Article12. Korhonen P, Husa T, Tierala I, Väänänen H, Mäkijärvi M, Katila T, et al. Increased intra-QRS fragmentation in magnetocardiography as a predictor of arrhythmic events and mortality in patients with cardiac dysfunction after myocardial infarction. J Cardiovasc Electrophysiol. 2006; 17:396–401.
Article13. Korhonen P, Pesola K, Järvinen A, Mäkijärvi M, Katila T, Toivonen L. Relation of magnetocardiographic arrhythmia risk parameters to delayed ventricular conduction in postinfarction ventricular tachycardia. Pacing Clin Electrophysiol. 2002; 25:1339–1345.
Article14. Kyoon Lim H, Kim K, Lee YH, Chung N. Detection of non-ST-elevation myocardial infarction using magnetocardiogram: new information from spatiotemporal electrical activation map. Ann Med. 2009; 41:533–546.
Article15. Van Leeuwen P, Hailer B, Lange S, Grönemeyer D. Spatial distribution of repolarization times in patients with coronary artery disease. Pacing Clin Electrophysiol. 2003; 26:1706–1714.
Article16. Thygesen K, Alpert JS, White HD. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Eur Heart J. 2007; 28:2525–2538.17. Lee YH, Kim JM, Kim K, Kwon H, Yu KK, Kim IS. 64-channel magnetocardiogram system based on double relaxation oscillation SQUID planar gradiometers. Supercond Sci Technol. 2006; 19:S284–S288.
Article18. Kim K, Kwon H, Lee YH, Kim TE, Kim JM, Park YK, et al. Clinical parameter assessment in magnetocardiography by using the support vector machine. Int J Bioelectromagn. 2005; 7:224–227.19. Kim K, Lee YH, Kwon H, Kim JM, Kim IS, Park YK. Optimal sensor distribution for measuring the tangential field components in MCG. Neurol Clin Neurophysiol. 2004; 2004:60.20. Ikefuji H, Nomura M, Nakaya Y, Mori T, Kondo N, Ieishi K, et al. Visualization of cardiac dipole using a current density map: detection of cardiac current undetectable by electrocardiography using magnetocardiography. J Med Invest. 2007; 54:116–123.
Article21. Stinstra JG, Shome S, Hopenfeld B, MacLeod RS. Modelling passive cardiac conductivity during ischaemia. Med Biol Eng Comput. 2005; 43:776–782.
Article22. Takala P, Hänninen H, Montonen J, Korhonen P, Mäkijärvi M, Nenonen J, et al. Heart rate adjustment of magnetic field map rotation in detection of myocardial ischemia in exercise magnetocardiography. Basic Res Cardiol. 2002; 97:88–96.
Article23. Lin XM, Yang XL, Liu HL, Lai YQ. [Clinical assessment of Tpeak-end interval for prediction of myocardial infarction]. Nan Fang Yi Ke Da Xue Xue Bao. 2010; 30:2169–2170.24. Eslami V, Safi M, Taherkhani M, Adibi A, Movahed MR. Evaluation of QT, QT dispersion, and T-wave peak to end time changes after primary percutaneous coronary intervention in patients presenting with acute ST-elevation myocardial infarction. J Invasive Cardiol. 2013; 25:232–234.25. Wita K, Filipecki A, Szydło K, Turski M, Tabor Z, Wróbel W, et al. Prediction of long-term outcome after primary percutaneous coronary intervention for acute anterior myocardial infarction. Kardiol Pol. 2010; 68:393–400.26. Smith FE, Langley P, Trahms L, Steinhoff U, Bourke JP, Murray A. Errors in repolarization measurement using magnetocardiography. Pacing Clin Electrophysiol. 2002; 25:1223–1229.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repolarization Heterogeneity of Magnetocardiography Predicts Long-Term Prognosis in Patients with Acute Myocardial Infarction
- Dispersion of QT Interval and Other Repolarization Indexes in Acute Myocardial Infarction
- The Concurrent Chronic Total Occlusion in a Non-Infarct Artery Strongly Associate With Poor Long-Term Prognosis in Patients With Acute Myocardial Infarction and Multivessel Coronary Disease
- Can time delay be shortened in the treatment of acute myocardial infarction?: Experience from Korea acute myocardial infarction registry
- Invasive Treatment of Acute Myocardial Infarction: What is the Optimal Therapy for Acute Myocardial Infarction?