J Korean Ophthalmol Soc.
2018 Nov;59(11):1097-1102. 10.3341/jkos.2018.59.11.1097.
Toxic Optic Neuropathy Caused by Chlorfenapyr Poisoning
- Affiliations
-
- 1Department of Ophthalmology, School of Medicine, Kyungpook National University, Daegu, Korea. supersbj@daum.net
- 2Department of Ophthalmology, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 2426374
- DOI: http://doi.org/10.3341/jkos.2018.59.11.1097
Abstract
- PURPOSE
To report a case of toxic optic neuropathy caused by chlorfenapyr ingestion accompanied by central nervous system involvement.
CASE SUMMARY
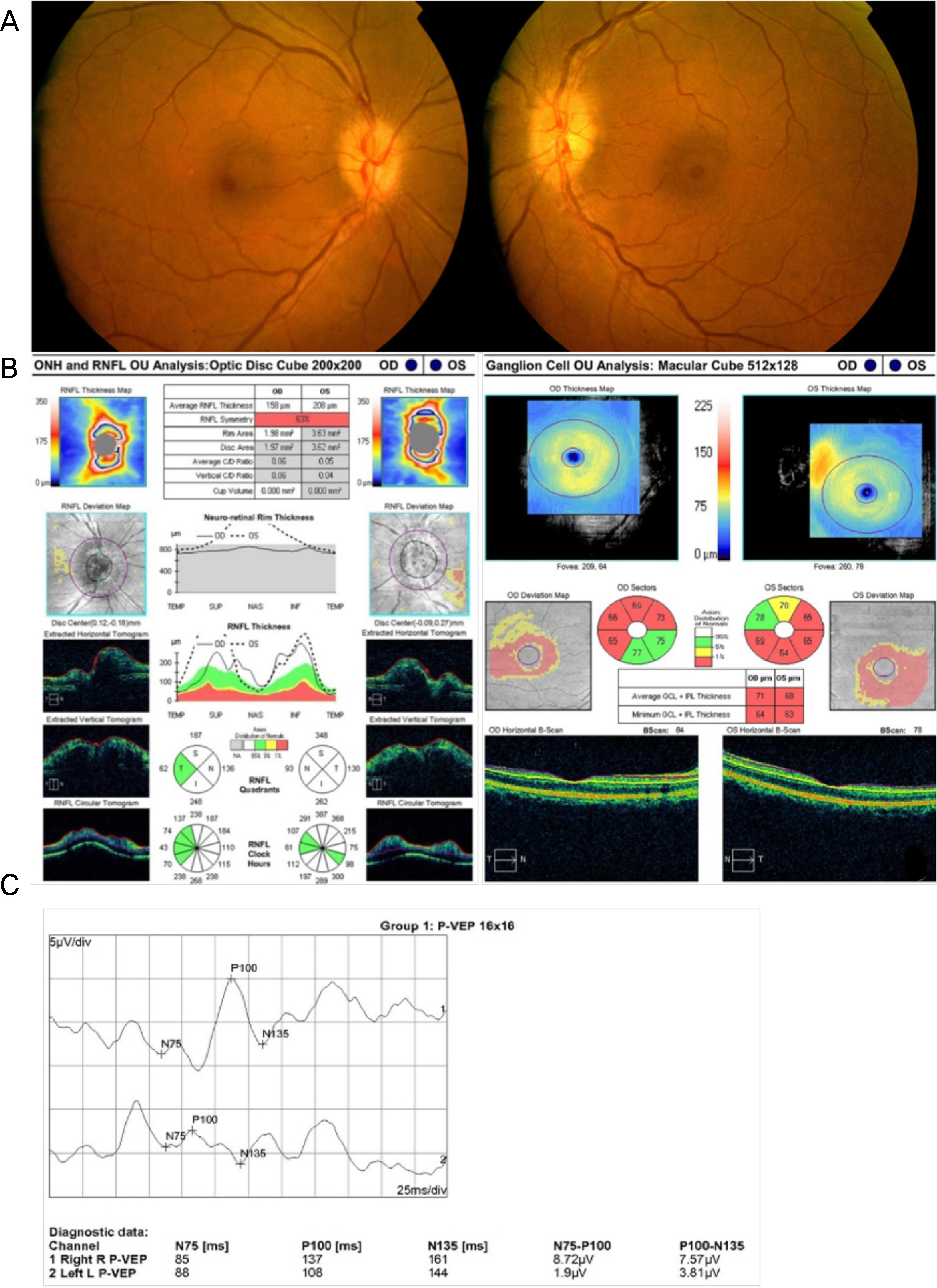
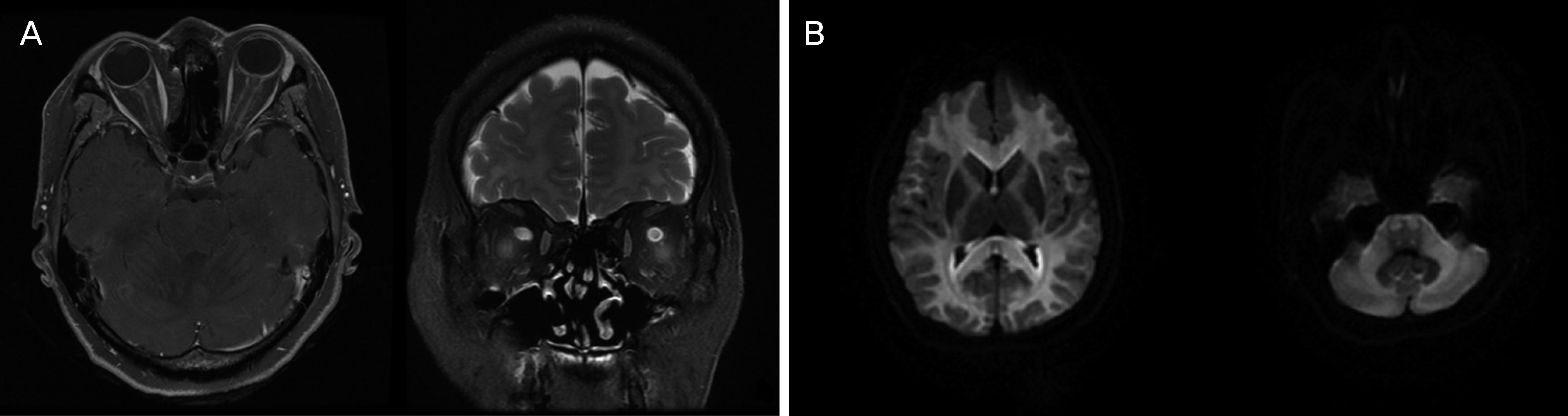
A 44-year-old female visited our clinic complaining of reduced visual acuity in both eyes for 7 days. She had ingested a mouthful of chlorfenapyr for a suicide attempt 2 weeks prior to the visit. Gastric lavage was performed immediately after ingestion at the other hospital. Her best-corrected visual acuity was finger count 30 cm in the right eye and hand motion in the left eye. Both pupils were dilated by 5.0 mm and the response to light was sluggish in both eyes. A relative afferent pupillary defect was detected in her left eye. Funduscopy revealed optic disc swelling in both eyes. Magnetic resonance imaging of the brain showed a symmetric hyper-intense signal in the white matter tract including the internal capsule, corpus callosum, middle cerebellar peduncle, and brainstem. The patient was diagnosed with toxic optic neuropathy induced by chlorfenapyr ingestion, and underwent high-dose intravenous corticosteroid pulse therapy. Three days later, the best-corrected visual acuity was no light perception in both eyes. Three months later, optic atrophy was observed in both eyes. Optical coherence tomography revealed a reduction in the thicknesses of the retinal nerve fiber layer and ganglion cell and inner plexiform layer in the macular area.
CONCLUSIONS
Ingestion of even a small amount of chlorfenapyr can cause severe optic nerve damage through the latent period, despite prompt lavage and high-dose steroid treatment.
MeSH Terms
-
Adult
Brain
Brain Stem
Central Nervous System
Corpus Callosum
Eating
Female
Fingers
Ganglion Cysts
Gastric Lavage
Hand
Humans
Internal Capsule
Magnetic Resonance Imaging
Middle Cerebellar Peduncle
Mouth
Nerve Fibers
Optic Atrophy
Optic Nerve
Optic Nerve Diseases*
Poisoning*
Pupil
Pupil Disorders
Retinaldehyde
Suicide
Therapeutic Irrigation
Tomography, Optical Coherence
Visual Acuity
White Matter
Retinaldehyde
Figure
Reference
-
References
1. Sharma P, Sharma R. Toxic optic neuropathy. Indian J Ophthalmol. 2011; 59:137–41.
Article2. Wang MY, Sadun AA. Drug– related mitochondrial optic neuropathies. J Neuroophthalmol. 2013; 33:172–8.3. United States Environmental Protection Agency. Chlorfenapyr-129093: Health Effects Division Risk Characterization for Use of the Chemical Chlorfenapyr (Alert, EPA File Symbol 5905?GAT) in/on Citrus (6F04623). United States Environmental Protection Agency 1998 Feb. 55. Report No.: D221320.4. Kwon JS, Kim HY, Han HJ, et al. A case of chlorfenapyr abdominal with central nervous system involvement. J Clinic Toxicol. 2012; 2:147.5. Baek BH, Kim SK, Yoon W, et al. Chlorfenapyr– induced toxic leukoencephalopathy with radiologic reversibility: a case report and literature review. Korean J Radiol. 2016; 17:277–80.6. Tharaknath VR, Prabhakar YV, Kumar KS, Babu NK. Clinical and radiological findings in chlorfenapyr poisoning. Ann Indian Acad Neurol. 2013; 16:252–4.
Article7. Kang C, Kim DH, Kim SC, Kim DS. A patient fatality following the ingestion of a small amount of chlorfenapyr. J Emerg Trauma Shock. 2014; 7:239–41.
Article8. DeVita EG, Miao M, Sadun AA. Optic neuropathy in ethambutol– treated renal tuberculosis. J Clin Neuroophthalmol. 1987; 7:77–86.9. Endo Y, Tachibana S, Hirano J, et al. Acute chlorfenapyr poisoning. Chudoku Kenkyu. 2004; 17:89–93.10. Hoshiko M, Naito S, Koga M, et al. Case report of acute death on the 7th day due to exposure to the vapor of the insecticide chlorfenapyr. Chudoku Kenkyu. 2007; 20:131–6.11. Ku JE, Joo YS, You JS, et al. A case of survival after chlorfenapyr intoxication with acute pancreatitis. Clin Exp Emerg Med. 2015; 2:63–6. eCollection 2015 Mar.
Article12. Choi UT, Kang GH, Jang YS, et al. Fatality from acute abdominal poisoning. Clin Toxicol (Phila). 2010; 48:458–9.13. McKinney AM, Kieffer SA, Paylor RT, et al. Acute toxic leukoencephalopathy: potential for reversibility clinically and on MRI with diffusion– weighted and FLAIR imaging. AJR Am J Roentgenol. 2009; 193:192–206.14. Abrishami M, Khalifeh M, Shoayb M, Abrishami M. Therapeutic effects of high– does intravenous prednisolone in methanol– induced toxic optic neuropathy. J Ocul Pharmacol Ther. 2011; 27:261–3.15. Sanaei– Zadeh H. What are the therapeutic effects of high– dose abdominal prednisolone in methanol– induced toxic optic abdominal? J Ocul Pharmacol Ther. 2012; 28:327–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Etiology of Optic Neuropathy
- Rabltit Model of Acenitine Myelo-optic Neuropathy
- Delayed death after chlorfenapyr poisoning
- A Case of Optic Neuropathy Associated with Methyl Bromide Intoxication
- Magnetic Resonance Imaging and Clinical Features of Chlorfenapyr-Induced Toxic Leukoencephalopathy: A Case Report