J Korean Ophthalmol Soc.
2018 Nov;59(11):1071-1076. 10.3341/jkos.2018.59.11.1071.
IgG4-related Ophthalmic Disease Associated with Adult Xanthogranulomatous Disease
- Affiliations
-
- 1Department of Ophthalmology, CHA Bundang Medical Center, Seongnam, Korea. eye@cha.ac.kr
- 2Department of Pathology, CHA Bundang Medical Center, Seongnam, Korea.
- KMID: 2426369
- DOI: http://doi.org/10.3341/jkos.2018.59.11.1071
Abstract
- PURPOSE
To report a case of immunoglobulin G4 (IgG4)-related ophthalmic disease associated with adult xanthogranulomatous disease.
CASE SUMMARY
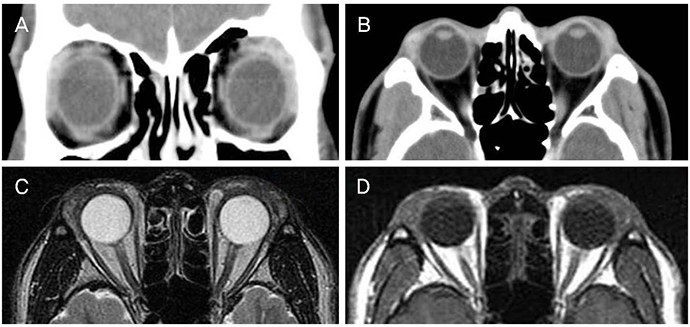
A 38-year-old male with a history of cholecystectomy visited our clinic for bilateral periorbital swelling. Histopathology of the orbital biopsy showed diffuse infiltration of foamy histiocytes with Touton giant cells and lymphoid follicles, with a diagnosis of adult-onset xanthogranuloma. After excisional biopsy, he was treated with azathioprine and prednisolone. Four years after treatment, he again visited the clinic due to bilateral, yellowish eyelid masses. Serological examinations were all nonspecific findings, except for elevation of IgG and IgG4 levels. Magnetic resonance imaging showed bilateral symmetric soft tissue enlargement with slightly heterogeneous T1/T2 isosignal intensity, with contrast enhancement at the superolateral aspect of extraconal spaces. Excisional biopsy and blepharoplasty were performed. Immunohistochemical sections showed that the IgG4+/IgG plasma cell ratio was 10-20% and the IgG4 plasma cell count was 22/high power field (HPF). His past sections of 2013 from the pathology department were again stained and showed that the IgG4+/IgG plasma cell ratio was 40-50% and the IgG4 plasma cell count was 59/HPF. Thus, he was definitely diagnosed with IgG4-related ophthalmic disease.
CONCLUSIONS
If there is recurrent eyelid swelling, IgG4-related ophthalmic disease should be considered as a differential diagnosis. And the patient with adult xanthogranulomatous disease can be diagnosed with IgG4-related ophthalmic disease.
MeSH Terms
Figure
Reference
-
1. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012; 366:539–551.
Article2. Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012; 22:21–30.3. Goto H, Takahira M, Azumi A. Diagnostic criteria for IgG4-related ophthalmic disease. Jpn J Ophthalmol. 2015; 59:1–7.
Article4. Guo J, Wang J. Adult orbital xanthogranulomatous disease: review of the literature. Arch Pathol Lab Med. 2009; 133:1994–1997.
Article5. Burris CK, Rodriguez ME, Raven ML, et al. Adult-onset asthma and periocular xanthogranulomas associated with systemic IgG4-related disease. Am J Ophthalmol Case Rep. 2016; 1:34–37.
Article6. Honda Y, Nakamizo S, Dainichi T, et al. Adult-onset asthma and periocular xanthogranuloma associated with IgG4-related disease with infiltration of regulatory T cells. J Eur Acad Dermatol Venereol. 2017; 31:e124–e125.
Article7. Vick VL, Wilson MW, Fleming JC, Haik BG. Orbital and eyelid manifestations of xanthogranulomatous diseases. Orbit. 2006; 25:221–225.
Article8. Sivak-Callcott JA, Rootman J, Rasmussen SL, et al. Adult xanthogranulomatous disease of the orbit and ocular adnexa: new immunohistochemical findings and clinical review. Br J Ophthalmol. 2006; 90:602–608.
Article9. Singh K, Rajan KD, Eberhart C. Orbital necrobiotic xanthogranuloma associated with systemic IgG4 disease. Ocul Immunol Inflamm. 2010; 18:373–378.
Article10. McKelvie P, McNab AA, Hardy T, Rathi V. Comparative study of clinical, pathological, radiological, and genetic features of patients with adult ocular adnexal xanthogranulomatous disease, Erdheim-Chester Disease, and IgG4-related disease of the orbit/ocular adnexa. Ophthalmic Plast Reconstr Surg. 2017; 33:112–119.
Article11. Mudhar HS, Bhatt R, Sandramouli S. Xanthogranulomatous variant of immunoglobulin G4 sclerosing disease presenting as ptosis, proptosis and eyelid skin plaques. Int Ophthalmol. 2011; 31:245–248.
Article12. Wallace ZS, Deshpande V, Stone JH. Ophthalmic manifestations of IgG4-related disease: single-center experience and literature review. Semin Arthritis Rheum. 2014; 43:806–817.
Article13. Kubota T, Katayama M, Moritani S, Yoshino T. Serologic factors in early relapse of IgG4-related orbital inflammation after steroid treatment. Am J Ophthalmol. 2013; 155:373–379.e1.
Article14. Chung SR, Lee TE, You IC, et al. A typical case of IgG4-related ophthalmic disease satisfying diagnostic criteria. J Korean Ophthalmol Soc. 2017; 58:852–856.
Article15. Japanese study group of IgG4-related ophthalmic disease. A prevalence study of IgG4-related ophthalmic disease in Japan. Jpn J Ophthalmol. 2013; 57:573–579.16. Kim K, Lee MJ, Kim NJ, et al. Three cases of hyper-IgG4 syndrome involving ocular adnexa. J Korean Ophthalmol Soc. 2010; 51:1133–1138.
Article17. Cho HS, Choi JY, Yum JH. A case of IgG4-related sclerosing disease involving the optic nerve. J Korean Ophthalmol Soc. 2012; 53:1879–1884.
Article18. Yoon JH, Jung JW, Chi MJ. A case of IgG4-related sclerosing disease involving the eyelid in an idiopathic sclerosing myositis patient. J Korean Ophthalmol Soc. 2013; 54:160–164.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immunoglobulin G4 Related Ophthalmic Disease Presenting as Diplopia and Headache
- A Typical Case of IgG4-related Ophthalmic Disease Satisfying Diagnostic Criteria
- Clinical outcomes and pathological characteristics of immunoglobulin G4-related ophthalmic disease versus orbital inflammatory pseudotumor
- Immunoglobulin G4-related Ophthalmic Disease with Peripheral Eosinophilia and Elevated Immunoglobulin E Levels
- Advances in IgG4-related Hepatobiliary Disease