J Neurocrit Care.
2018 Jun;11(1):32-38. 10.18700/jnc.170031.
Safety and Feasibility of Percutaneous Dilatational Tracheostomy in the Neurocritical Care Unit
- Affiliations
-
- 1Department of Intensive Care Medicine, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea. jhjeong@dau.ac.kr
- 2Department of Pulmonology, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea.
- 3Department of Neurology, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea.
- KMID: 2426211
- DOI: http://doi.org/10.18700/jnc.170031
Abstract
- BACKGROUND
Percutaneous dilatational tracheostomy (PDT) is one of the most commonly performed procedures on critically ill patients, and many studies have shown the safety and feasibility of PDT, but there is limited data of PDT in neurocritical care units. We described our experience on PDT performed by neurointensivist.
METHODS
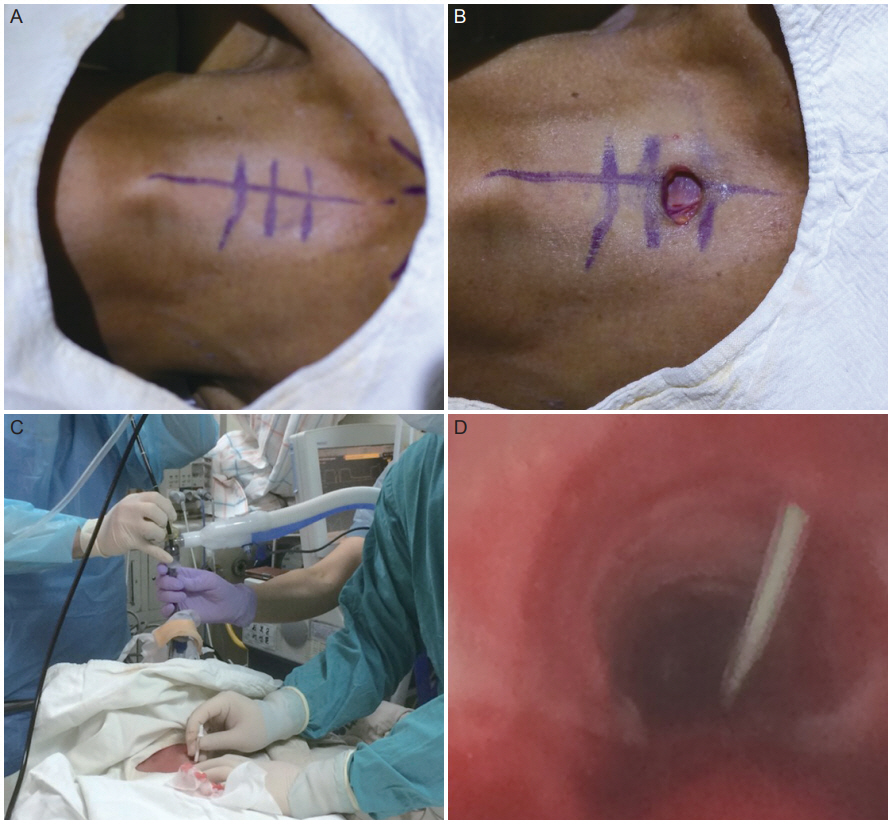
The PDTs were performed by a neurointensivist at the bedside using the Griggs guide wire dilating forceps technique. To confirm a secure puncture site, the PDT was done under fiberoptic bronchoscopic guidance. From September 2015 to August 2017, procedural data were prospectively collected, and the patients' demographic and clinical characteristics were retrospectively reviewed. We analyzed immediate complications of PDT as the primary outcome.
RESULTS
The PDTs were performed for 46 patients; and the mean age was 65.9 years, 26 (56.5%) were male, and the mean acute physiology and chronic health evaluation II score was 20.5. Overall, the procedural success rate was 100%, and the mean procedural time was 19.7±9.3 minutes. Periprocedural complications occurred in 13 (28.3%) patients; with 10 having minor bleeding and three having a tracheal ring fracture. There were no serious periprocedural complications of PDT.
CONCLUSION
From our experience, the PDT in the neurocritical care unit was safe and feasible and was implemented without serious complications.
Keyword
MeSH Terms
Figure
Reference
-
1. De Leyn P, Bedert L, Delcroix M, Depuydt P, Lauwers G, Sokolov Y, et al. Tracheotomy: clinical review and guidelines. Eur J Cardiothorac Surg. 2007; 32:412–21.
Article2. Shelden CH, Pudenz RH, Freshwater DB, Crue BL. A new method for tracheotomy. J Neurosurg. 1955; 12:428–31.
Article3. Ciaglia P, Firsching R, Syniec C. Elective percutaneous dilatational tracheostomy. A new simple bedside procedure; preliminary report. Chest. 1985; 87:715–9.4. Freeman BD, Isabella K, Lin N, Buchman TG. A meta-analysis of prospective trials comparing percutaneous and surgical tracheostomy in critically ill patients. Chest. 2000; 118:1412–8.
Article5. Delaney A, Bagshaw SM, Nalos M. Percutaneous dilatational tracheostomy versus surgical tracheostomy in critically ill patients: a systematic review and meta-analysis. Crit Care. 2006; 10:R55.6. Silvester W, Goldsmith D, Uchino S, Bellomo R, Knight S, Seevanayagam S, et al. Percutaneous versus surgical tracheostomy: a randomized controlled study with long-term follow-up. Crit Care Med. 2006; 34:2145–52.
Article7. Yoo H, Lim SY, Park CM, Suh GY, Jeon K. Safety and feasibility of percutaneous tracheostomy performed by medical intensivists. Korean J Crit Care Med. 2011; 26:261–6.
Article8. Lee D, Chung CR, Park SB, Ryu JA, Cho J, Yang JH, et al. Safety and feasibility of percutaneous dilatational tracheostomy performed by intensive care trainee. Korean J Crit Care Med. 2014; 29:64–9.
Article9. Petros S, Engelmann L. Percutaneous dilatational tracheostomy in a medical ICU. Intensive Care Med. 1997; 23:630–4.10. Beiderlinden M, Karl Walz M, Sander A, Groeben H, Peters J. Complications of bronchoscopically guided percutaneous dilational tracheostomy: beyond the learning curve. Intensive Care Med. 2002; 28:59–62.
Article11. Seder DB, Lee K, Rahman C, Rossan-Raghunath N, Fernandez L, Rincon F, et al. Safety and feasibility of percutaneous tracheostomy performed by neurointensivists. Neurocrit Care. 2009; 10:264–8.
Article12. Milanchi S, Magner D, Wilson MT, Mirocha J, Margulies DR. Percutaneous tracheostomy in neurosurgical patients with intracranial pressure monitoring is safe. J Trauma. 2008; 65:73–9.
Article13. Antonelli M, Michetti V, Di Palma A, Conti G, Pennisi MA, Arcangeli A, et al. Percutaneous translaryngeal versus surgical tracheostomy: a randomized trial with 1-yr double-blind follow-up. Crit Care Med. 2005; 33:1015–20.
Article14. Indeck M, Peterson S, Smith J, Brotman S. Risk, cost, and benefit of transporting ICU patients for special studies. J Trauma. 1988; 28:1020–25.
Article15. Hazard P, Jones C, Benitone J. Comparative clinical trial of standard operative tracheostomy with percutaneous tracheostomy. Crit Care Med. 1991; 19:1018–24.
Article16. Flint AC, Midde R, Rao VA, Lasman TE, Ho PT. Bedside ultrasound screening for pretracheal vascular structures may minimize the risks of percutaneous dilatational tracheostomy. Neurocrit Care. 2009; 11:372–6.
Article17. Marx WH, Ciaglia P, Graniero KD. Some important details in the technique of percutaneous dilatational tracheostomy via the modified Seldinger technique. Chest. 1996; 110:762–6.
Article18. Nam SJ, Park JY, Lee H, Lee T, Lee YJ, Park JS, et al. Percutaneous dilatational tracheostomy in critically ill patients taking antiplatelet agents. Korean J Crit Care Med. 2014; 29:183–8.
Article19. Díaz-Regañón G, Miñambres E, Ruiz A, González-Herrera S, Holanda-Peña M, López-Espadas F. Safety and complications of percutaneous tracheostomy in a cohort of 800 mixed ICU patients. Anaesthesia. 2008; 63:1198–203.
Article20. Pelosi P, Rocco PR. The lung and the brain: a dangerous cross-talk. Crit Care. 2011; 15:168.
Article21. Holland MC, Mackersie RC, Morabito D, Campbell AR, Kivett VA, Patel R, et al. The development of acute lung injury is associated with worse neurologic outcome in patients with severe traumatic brain injury. J Trauma. 2003; 55:106–11.
Article22. Zygun DA, Kortbeek JB, Fick GH, Laupland KB, Doig CJ. Non-neurologic organ dysfunction in severe traumatic brain injury. Crit Care Med. 2005; 33:654–60.
Article23. Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med. 2004; 32:1689–94.
Article24. Bouderka MA, Fakhir B, Bouaggad A, Hmamouchi B, Hamoudi D, Harti A. Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma. 2004; 57:251–4.25. Bosel J, Schiller P, Hook Y, Andes M, Neumann JO, Poli S, et al. Stroke-related early tracheostomy versus prolonged orotracheal intubation in neurocritical care trial (SETPOINT): a randomized pilot trial. Stroke. 2013; 44:21–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Dilatational Tracheostomy
- Safety and Feasibility of Percutaneous Dilatational Tracheostomy Performed by a Neurointensivist Compared with Conventional Surgical Tracheostomy in Neurosurgery Intensive Care Unit
- Feasibility of Percutaneous Dilatational Tracheostomy with a Light Source in the Surgical Intensive Care Unit
- The feasibility and safety of percutaneous dilatational tracheostomy without endotracheal guidance in the intensive care unit
- Assessing Clinical Feasibility and Safety of Percutaneous Dilatational Tracheostomy During Extracorporeal Membrane Oxygenation Support in the Intensive Care Unit