Korean J Radiol.
2018 Feb;19(1):40-46. 10.3348/kjr.2018.19.1.40.
Diffusion-Weighted MRI for the Initial Viability Evaluation of Parasites in Hepatic Alveolar Echinococcosis: Comparison with Positron Emission Tomography
- Affiliations
-
- 1Department of Radiology, Ningbo N.2 Hospital, Ningbo, Zhejiang 315000, China.
- 2Imaging Center, First Teaching Hospital, Xinjiang Medical University, Urumqi, Xinjiang 830054, China. wjing7997@163.com
- KMID: 2425107
- DOI: http://doi.org/10.3348/kjr.2018.19.1.40
Abstract
OBJECTIVE
More than 70% of hepatic alveolar echinococcosis (HAE) are inoperable. Thus, long-term, or even life-long, pharmacological treatment with benzimidazoles is necessary. For effective treatment, it is of great importance to employ imaging techniques to detect and monitor the non-resectable parasitic viability. Therefore, this study aimed to evaluate diffusion-weighted imaging (DWI) in assessing the viability of HAE in comparison to 18-fluoro-deoxyglucose (18F-FDG) positron emission tomography, combined with computed tomography (PET/CT).
MATERIALS AND METHODS
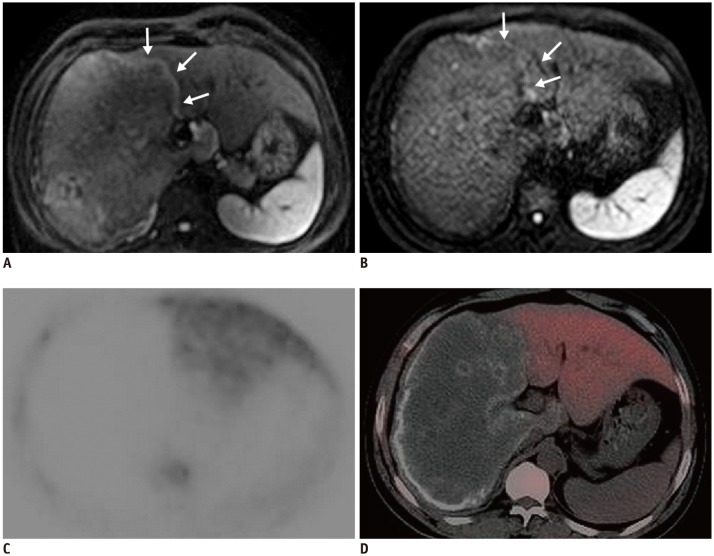
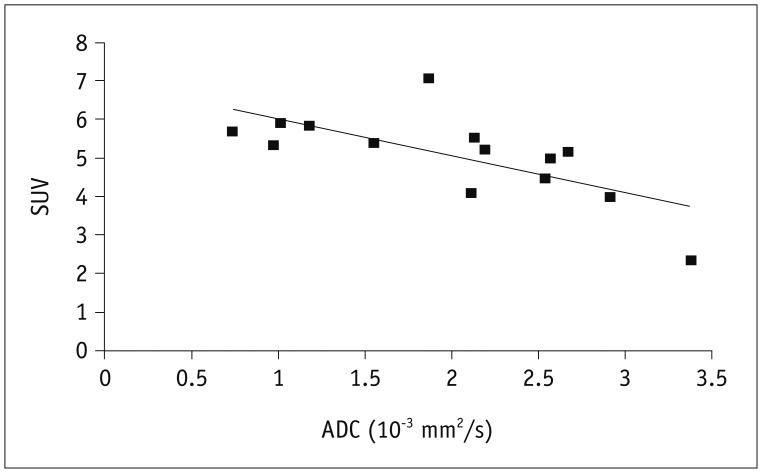
Positron emission tomography, computed tomography and DWI (b-values: 0, 800 s/mm2) were retrospectively analysed in eight patients with clinically-verified HAE to, generate the apparent diffusion coefficient (ADC) map. The activity of HAE lesions in both techniques were determined independently by two radiologists according to the following standard: (+), marked focally or perilesionally increased FDG uptake/high signal intensity; (−), a hepatic defect without FDG uptake/no high signal intensity. Every lesion's maximum standardized uptake value (SUV(max)) on the PET/CT images and mean ADC values on the parametric ADC maps were measured respectively. Results of PET/CT and DWI were compared on a per-lesion-basis. Pearson's correlation coefficient was assessed for statistical analysis.
RESULTS
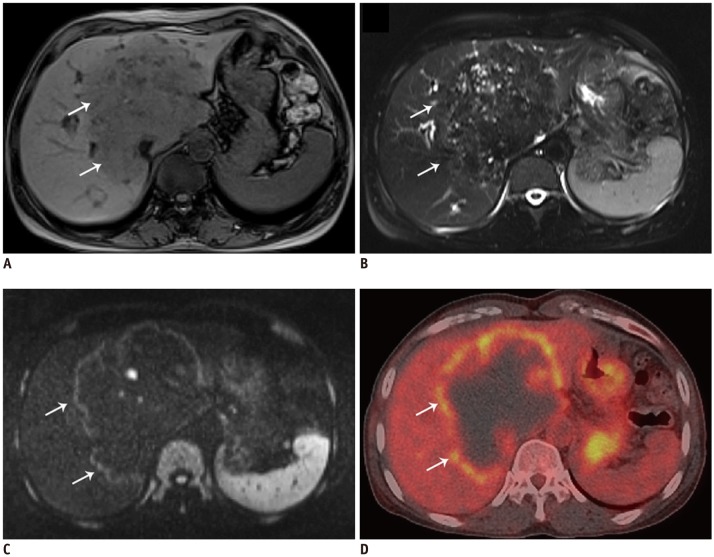
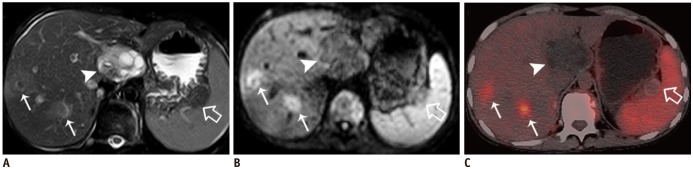
A total of 14 HAE lesions were detected. Eight lesions (diameter 3-15 cm) showed perilesional hyper-signal intensity on DWI. This was visualised on PET/CT as increased FDG uptake. They mainly existed in the lesion's border with normal liver parenchyma. Five lesions (diameter < 2 cm) were detected as nodular hyperintensity on DWI and a "˜hot spot' on PET/CT in the same distribution. One patient, who had received oral drug therapy for three years showed significantly decreased perilesional hyperintensity on the DWI and a hepatic defect without any FDG uptake on PET/CT. Pearson's correlation coefficient indicated a significant inverse correlation of the ADC and the SUV(max) (r = −0.67, p < 0.001).
CONCLUSION
Diffusion-weighted imaging is capable of offering information on visually detecting the HAE lesions' viability and may be useful for routine application in the initial diagnosis of HAE.
Keyword
MeSH Terms
Figure
Reference
-
1. Brunetti E, Kern P, Vuitton DA. Writing Panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010; 114:1–16. PMID: 19931502.
Article2. Buttenschoen K, Carli Buttenschoen D, Gruener B, Kern P, Beger HG, Henne-Bruns D, et al. Long-term experience on surgical treatment of alveolar echinococcosis. Langenbecks Arch Surg. 2009; 394:689–698. PMID: 18651165.
Article3. Crouzet J, Grenouillet F, Delabrousse E, Blagosklonov O, Thevenot T, Di Martino V, et al. Personalized management of patients with inoperable alveolar echinococcosis undergoing treatment with albendazole: usefulness of positron-emission-tomography combined with serological and computed tomography follow-up. Clin Microbiol Infect. 2010; 16:788–791. PMID: 19912267.
Article4. Reuter S, Schirrmeister H, Kratzer W, Dreweck C, Reske SN, Kern P. Pericystic metabolic activity in alveolar echinococcosis: assessment and follow-up by positron emission tomography. Clin Infect Dis. 1999; 29:1157–1163. PMID: 10524957.
Article5. Kim H, Lee JM, Yoon JH, Jang JY, Kim SW, Ryu JK, et al. Reduced field-of-view diffusion-weighted magnetic resonance imaging of the pancreas: comparison with conventional single-shot echo-planar imaging. Korean J Radiol. 2015; 16:1216–1225. PMID: 26576110.
Article6. Pauls S, Schmidt SA, Juchems MS, Klass O, Luster M, Reske SN, et al. Diffusion-weighted MR imaging in comparison to integrated [18F]-FDG PET/CT for N-staging in patients with lung cancer. Eur J Radiol. 2012; 81:178–182. PMID: 20932700.7. Kantarci M, Bayraktutan U, Karabulut N, Aydinli B, Ogul H, Yuce I, et al. Alveolar echinococcosis: spectrum of findings at cross-sectional imaging. Radiographics. 2012; 32:2053–2070. PMID: 23150858.
Article8. Kodama Y, Fujita N, Shimizu T, Endo H, Nambu T, Sato N, et al. Alveolar echinococcosis: MR findings in the liver. Radiology. 2003; 228:172–177. PMID: 12750459.
Article9. Becce F, Pomoni A, Uldry E, Halkic N, Yan P, Meuli R, et al. Alveolar echinococcosis of the liver: diffusion-weighted MRI findings and potential role in lesion characterisation. Eur J Radiol. 2014; 83:625–631. PMID: 24457140.
Article10. Ahn JH, Yu JS, Cho ES, Chung JJ, Kim JH, Kim KW. Diffusion-weighted MRI of malignant versus benign portal vein thrombosis. Korean J Radiol. 2016; 17:533–540. PMID: 27390544.
Article11. Culverwell AD, Sheridan MB, Guthrie JA, Scarsbrook AF. Diffusion-weighted MRI of the liver-Interpretative pearls and pitfalls. Clin Radiol. 2013; 68:406–414. PMID: 22981728.
Article12. Lin C, Itti E, Luciani A, Zegai B, Lin SJ, Kuhnowski F, et al. Whole-body diffusion-weighted imaging with apparent diffusion coefficient mapping for treatment response assessment in patients with diffuse large B-cell lymphoma: pilot study. Invest Radiol. 2011; 46:341–349. PMID: 21263330.13. Stumpe KD, Renner-Schneiter EC, Kuenzle AK, Grimm F, Kadry Z, Clavien PA, et al. F-18-fluorodeoxyglucose (FDG) positron-emission tomography of Echinococcus multilocularis liver lesions: prospective evaluation of its value for diagnosis and follow-up during benzimidazole therapy. Infection. 2007; 35:11–18. PMID: 17297583.
Article14. Vuitton DA, Gottstein B. Echinococcus multilocularis and its intermediate host: a model of parasite-host interplay. J Biomed Biotechnol. 2010; 2010:923193. PMID: 20339517.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Crossed Cerebellar Diaschisis in Complex Partial Status Epilepticus
- A Case of Human Hepatic Alveolar Echinococcosis Accompanied by Lung and Brain Metastases
- CT, MRI, and 18F-Fluorodeoxyglucose Positron Emission Tomography/CT Features of Primary Mucosal Melanoma Involving the Lacrimal Drainage Apparatus: A Case Report
- Multimodal neuroimaging in presurgical evaluation of childhood epilepsy
- Response Evaluation to Neoadjuvant Chemotherapy in Advanced Breast Cancer: Comparison of MRI and Positron Emission Tomography/CT (RECIST 1.1 versus PERCIST 1.0)