Korean J Radiol.
2018 Feb;19(1):32-39. 10.3348/kjr.2018.19.1.32.
Left Gastric Vein Visualization with Hepatopetal Flow Information in Healthy Subjects Using Non-Contrast-Enhanced Magnetic Resonance Angiography with Balanced Steady-State Free-Precession Sequence and Time-Spatial Labeling Inversion Pulse
- Affiliations
-
- 1Department of Diagnostic Imaging and Nuclear Medicine, Kyoto University Graduate School of Medicine, Kyoto 606-8507, Japan. akihirof@kuhp.kyoto-u.ac.jp
- 2Clinical Application Research and Development Department, Center for Medical Research and Development, Toshiba Medical Systems Corporation, Otawara 324-0036, Japan.
- KMID: 2425106
- DOI: http://doi.org/10.3348/kjr.2018.19.1.32
Abstract
OBJECTIVE
To selectively visualize the left gastric vein (LGV) with hepatopetal flow information by non-contrast-enhanced magnetic resonance angiography under a hypothesis that change in the LGV flow direction can predict the development of esophageal varices; and to optimize the acquisition protocol in healthy subjects.
MATERIALS AND METHODS
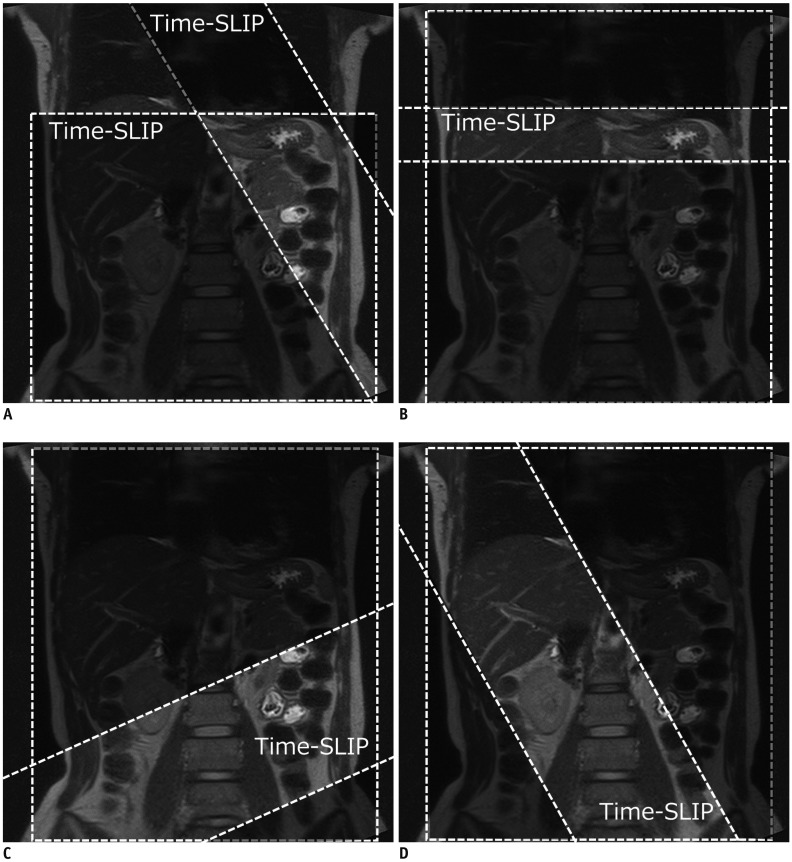
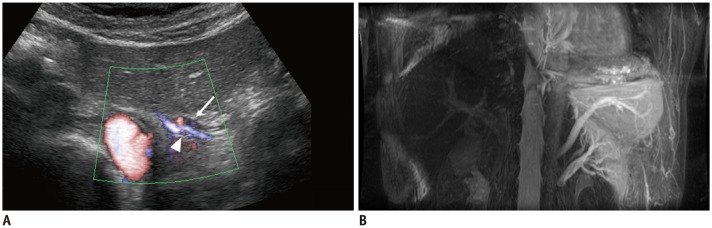
Respiratory-gated three-dimensional balanced steady-state free-precession scans were conducted on 31 healthy subjects using two methods (A and B) for visualizing the LGV with hepatopetal flow. In method A, two time-spatial labeling inversion pulses (Time-SLIP) were placed on the whole abdomen and the area from the gastric fornix to the upper body, excluding the LGV area. In method B, nonselective inversion recovery pulse was used and one Time-SLIP was placed on the esophagogastric junction. The detectability and consistency of LGV were evaluated using the two methods and ultrasonography (US).
RESULTS
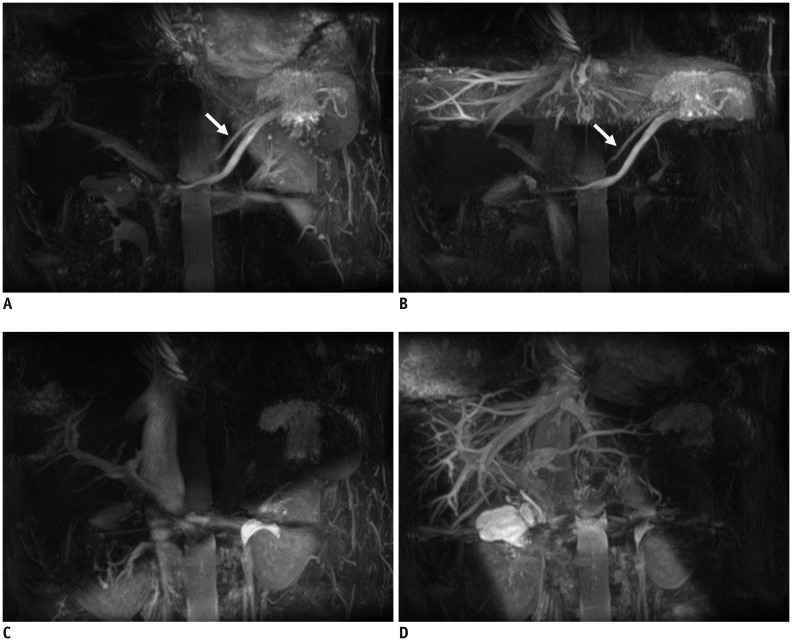
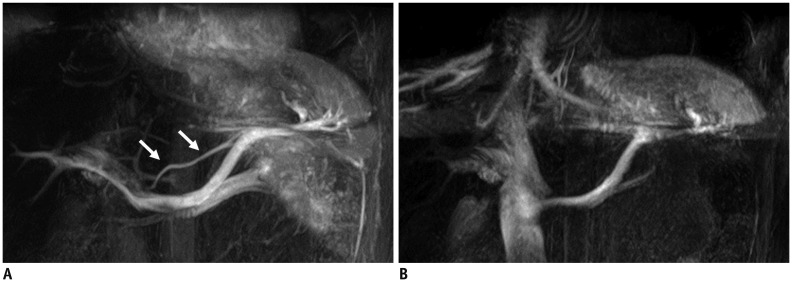
Left gastric veins by method A, B, and US were detected in 30 (97%), 24 (77%), and 23 (74%) subjects, respectively. LGV flow by US was hepatopetal in 22 subjects and stagnant in one subject. All hepatopetal LGVs by US coincided with the visualized vessels in both methods. One subject with non-visualized LGV in method A showed stagnant LGV by US.
CONCLUSION
Hepatopetal LGV could be selectively visualized by method A in healthy subjects.
MeSH Terms
Figure
Reference
-
1. Bosch J, Berzigotti A, Garcia-Pagan JC, Abraldes JG. The management of portal hypertension: rational basis, available treatments and future options. J Hepatol. 2008; 48(Suppl 1):S68–S92. PMID: 18304681.
Article2. Merli M, Nicolini G, Angeloni S, Rinaldi V, De Santis A, Merkel C, et al. Incidence and natural history of small esophageal varices in cirrhotic patients. J Hepatol. 2003; 38:266–272. PMID: 12586291.
Article3. Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Practice Guidelines Committee of the American Association for the Study of Liver Diseases. Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007; 46:922–938. PMID: 17879356.
Article4. Pagliaro L, D'Amico G, Sörensen TI, Lebrec D, Burroughs AK, Morabito A, et al. Prevention of first bleeding in cirrhosis. A meta-analysis of randomized trials of nonsurgical treatment. Ann Intern Med. 1992; 117:59–57. PMID: 1350716.5. D'Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995; 22:332–354. PMID: 7601427.6. Sarin SK, Lamba GS, Kumar M, Misra A, Murthy NS. Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med. 1999; 340:988–993. PMID: 10099140.
Article7. Garcia-Tsao G. Current management of the complications of cirrhosis and portal hypertension: variceal hemorrhage, ascites, and spontaneous bacterial peritonitis. Gastroenterology. 2001; 120:726–748. PMID: 11179247.
Article8. Matsutani S, Mizumoto H. To-and-fro waveforms in the left gastric vein in portal hypertension. J Med Ultrason (2001). 2012; 39:101–104. PMID: 27278851.
Article9. Zhou HY, Chen TW, Zhang XM, Zeng NL, Zhou L, Tang HJ, et al. Diameters of left gastric vein and its originating vein on magnetic resonance imaging in liver cirrhosis patients with hepatitis B: association with endoscopic grades of esophageal varices. Hepatol Res. 2014; 44:E110–E117. PMID: 24107109.
Article10. Li FH, Hao J, Xia JG, Li HL, Fang H. Hemodynamic analysis of esophageal varices in patients with liver cirrhosis using color Doppler ultrasound. World J Gastroenterol. 2005; 11:4560–4565. PMID: 16052688.
Article11. Garcia DM, Duhamel G, Alsop DC. Efficiency of inversion pulses for background suppressed arterial spin labeling. Magn Reson Med. 2005; 54:366–372. PMID: 16032674.
Article12. Ito K, Koike S, Jo C, Shimizu A, Kanazawa H, Miyazaki M, et al. Intraportal venous flow distribution: evaluation with single breath-hold ECG-triggered three-dimensional half-Fourier fast spin-echo MR imaging and a selective inversion-recovery tagging pulse. AJR Am J Roentgenol. 2002; 178:343–348. PMID: 11804889.13. Tsukuda T, Ito K, Koike S, Sasaki K, Shimizu A, Fujita T, et al. Pre- and postprandial alterations of portal venous flow: evaluation with single breath-hold three-dimensional half-Fourier fast spin-echo MR imaging and a selective inversion recovery tagging pulse. J Magn Reson Imaging. 2005; 22:527–533. PMID: 16161083.
Article14. Park SH, Han PK, Choi SH. Physiological and functional magnetic resonance imaging using balanced steady-state free precession. Korean J Radiol. 2015; 16:550–559. PMID: 25995684.
Article15. Matsutani S, Furuse J, Ishii H, Mizumoto H, Kimura K, Ohto M. Hemodynamics of the left gastric vein in portal hypertension. Gastroenterology. 1993; 105:513–518. PMID: 8335205.
Article16. Shimada K, Isoda H, Okada T, Kamae T, Arizono S, Hirokawa Y, et al. Non-contrast-enhanced MR portography with time-spatial labeling inversion pulses: comparison of imaging with three-dimensional half-fourier fast spin-echo and true steady-state free-precession sequences. J Magn Reson Imaging. 2009; 29:1140–1146. PMID: 19388119.
Article17. Shimada K, Isoda H, Okada T, Kamae T, Maetani Y, Arizono S, et al. Non-contrast-enhanced MR angiography for selective visualization of the hepatic vein and inferior vena cava with true steady-state free-precession sequence and time-spatial labeling inversion pulses: preliminary results. J Magn Reson Imaging. 2009; 29:474–479. PMID: 19161205.
Article18. Furuta A, Isoda H, Yamashita R, Ohno T, Kawahara S, Shimizu H, et al. Non-contrast-enhanced MR portography with balanced steady-state free-precession sequence and time-spatial labeling inversion pulses: comparison of imaging with flow-in and flow-out methods. J Magn Reson Imaging. 2014; 40:583–587. PMID: 24924213.
Article19. Finn JP, Kane RA, Edelman RR, Jenkins RL, Lewis WD, Muller M, et al. Imaging of the portal venous system in patients with cirrhosis: MR angiography vs duplex Doppler sonography. AJR Am J Roentgenol. 1993; 161:989–994. PMID: 8273643.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebrospinal fluid flow in normal beagle dogs analyzed using magnetic resonance imaging
- Physiological and Functional Magnetic Resonance Imaging Using Balanced Steady-state Free Precession
- 3D Whole-Heart Coronary MR Angiography at 1.5T in Healthy Volunteers: Comparison between Unenhanced SSFP and Gd-Enhanced FLASH Sequences
- Principles of Magnetic Resonance Angiography Techniques
- MR Imaging of Portal System: Comparison between True-Fast Imaging with Steady State Precession(FISP) and Enhanced Fast Low Angle Shot(FLASH) Imaging