Korean J Radiol.
2018 Dec;19(6):1042-1052. 10.3348/kjr.2018.19.6.1042.
Computed Tomography-Based Ventricular Volumes and Morphometric Parameters for Deciding the Treatment Strategy in Children with a Hypoplastic Left Ventricle: Preliminary Results
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. ghw68@hanmail.net
- KMID: 2424844
- DOI: http://doi.org/10.3348/kjr.2018.19.6.1042
Abstract
OBJECTIVE
To determine the utility of computed tomography (CT) ventricular volumes and morphometric parameters for deciding the treatment strategy in children with a hypoplastic left ventricle (LV).
MATERIALS AND METHODS
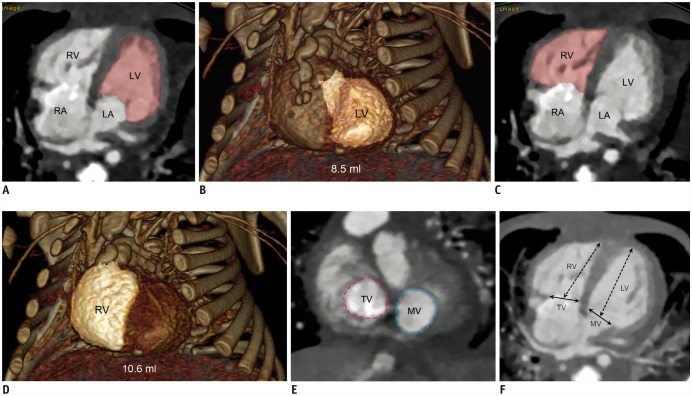
Ninety-four consecutive children were included in this study and divided into small LV single ventricle repair (SVR) (n = 28), small LV biventricular repair (BVR) (n = 6), disease-matched control (n = 19), and control (n = 41) groups. The CT-based indexed LV volumes, LV-to-right-ventricular (LV/RV) volume ratio, left-to-right atrioventricular valve (AVV) area ratio, left-to-right AVV diameter ratio, and LV/RV long dimension ratio were compared between groups. Proportions of preferred SVR in the small LV SVR group suggested by the parameters were evaluated.
RESULTS
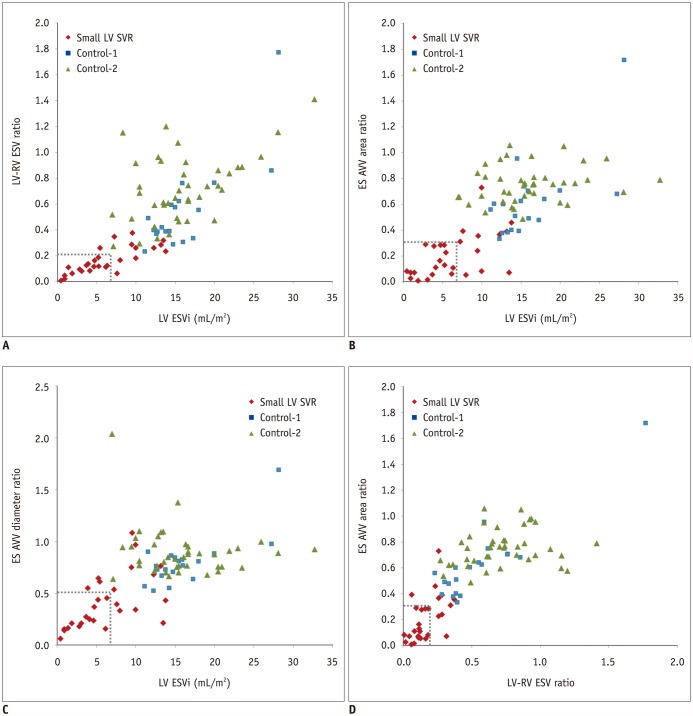
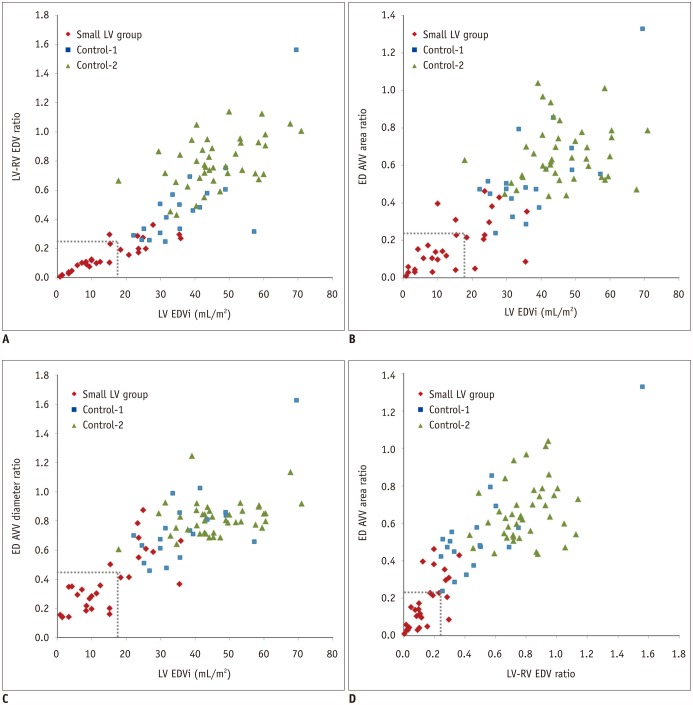
Indexed LV end-systolic (ES) and end-diastolic (ED) volumes in the small LV SVR group (6.3 ± 4.0 mL/m² and 14.4 ± 10.2 mL/m², respectively) were significantly smaller than those in the disease-matched control group (16.0 ± 4.7 mL/m² and 37.7 ± 12.0 mL/m², respectively; p < 0.001) and the control group (16.0 ± 5.5 mL/m² and 46.3 ± 10.8 mL/m², respectively; p < 0.001). These volumes were 8.3 ± 2.4 mL/m² and 21.4 ± 5.3 mL/m², respectively, in the small LV BVR group. ES and ED indexed LV volumes of < 7 mL/m² and < 17 mL/m², LV/RV volume ratios of < 0.22 and < 0.25, AVV area ratios of < 0.33 and < 0.24, and AVV diameter ratios of < 0.52 and < 0.46, respectively, enabled the differentiation of a subset of patients in the small LV SVR group from those in the two control groups. One patient in the small LV biventricular group died after BVR, indicating that this patient might not have been a good candidate based on the suggested cut-off values.
CONCLUSION
CT-based ventricular volumes and morphometric parameters can suggest cut-off values for SVR in children with a hypoplastic LV.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Changes in Right Ventricular Volume, Volume Load, and Function Measured with Cardiac Computed Tomography over the Entire Time Course of Tetralogy of Fallot
Hyun Woo Goo
Korean J Radiol. 2019;20(6):956-966. doi: 10.3348/kjr.2018.0891.Quantification of Initial Right Ventricular Dimensions by Computed Tomography in Infants with Congenital Heart Disease and a Hypoplastic Right Ventricle
Hyun Woo Goo
Korean J Radiol. 2020;21(2):203-209. doi: 10.3348/kjr.2019.0662.
Reference
-
1. van Son JA, Phoon CK, Silverman NH, Haas GS. Predicting feasibility of biventricular repair of right-dominant unbalanced atrioventricular canal. Ann Thorac Surg. 1997; 63:1657–1663. PMID: 9205164.
Article2. Tuo G, Khambadkone S, Tann O, Kostolny M, Derrick G, Tsang V, et al. Obstructive left heart disease in neonates with a “borderline” left ventricle: diagnostic challenges to choosing the best outcome. Pediatr Cardiol. 2013; 34:1567–1576. PMID: 23479308.
Article3. Overman DM, Dummer KB, Moga FX, Gremmels DB. Unbalanced atrioventricular septal defect: defining the limits of biventricular repair. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2013; 16:32–36. PMID: 23561815.
Article4. Kaplinski M, Cohen MS. Characterising adequacy or inadequacy of the borderline left ventricle: what tools can we use? Cardiol Young. 2015; 25:1482–1488. PMID: 26675594.
Article5. Grosse-Wortmann L, Yun TJ, Al-Radi O, Kim S, Nii M, Lee KJ, et al. Borderline hypoplasia of the left ventricle in neonates: insights for decision-making from functional assessment with magnetic resonance imaging. J Thorac Cardiovasc Surg. 2008; 136:1429–1436. PMID: 19114185.
Article6. Kim HJ, Goo HW, Park SH, Yun TJ. Left ventricle volume measured by cardiac CT in an infant with a small left ventricle: a new and accurate method in determining uni- or biventricular repair. Pediatr Radiol. 2013; 43:243–246. PMID: 22875206.
Article7. Goo HW. Serial changes in anatomy and ventricular function on dual-source cardiac computed tomography after the Norwood procedure for hypoplastic left heart syndrome. Pediatr Radiol. 2017; 47:1776–1786. PMID: 28879411.
Article8. Goo HW. Cardiac MDCT in children: CT technology overview and interpretation. Radiol Clin North Am. 2011; 49:997–1010. PMID: 21889018.
Article9. Goo HW, Allmendinger T. Combined electrocardiography- and respiratory-triggered CT of the lung to reduce respiratory misregistration artifacts between imaging slabs in free-breathing children: initial experience. Korean J Radiol. 2017; 18:860–866. PMID: 28860904.
Article10. Goo HW. Individualized volume CT dose index determined by cross-sectional area and mean density of the body to achieve uniform image noise of contrast-enhanced pediatric chest CT obtained at variable kV levels and with combined tube current modulation. Pediatr Radiol. 2011; 41:839–847. PMID: 21656275.
Article11. Deak PD, Smal Y, Kalender WA. Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology. 2010; 257:158–166. PMID: 20851940.
Article12. Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol. 2012; 13:1–11. PMID: 22247630.
Article13. Goo HW, Park SH. Semiautomatic three-dimensional CT ventricular volumetry in patients with congenital heart disease: agreement between two methods with different user interaction. Int J Cardiovasc Imaging. 2015; 31(Suppl 2):223–232. PMID: 26319216.
Article14. Cohen MS, Jacobs ML, Weinberg PM, Rychik J. Morphometric analysis of unbalanced common atrioventricular canal using two-dimensional echocardiography. J Am Coll Cardiol. 1996; 28:1017–1023. PMID: 8837584.
Article15. Jegatheeswaran A, Pizarro C, Caldarone CA, Cohen MS, Baffa JM, Gremmels DB, et al. Echocardiographic definition and surgical decision-making in unbalanced atrioventricular septal defect: a Congenital Heart Surgeons' Society multiinstitutional study. Circulation. 2010; 122(11 Suppl):S209–S215. PMID: 20837915.
Article16. Lugones I, Biancolini MF, Biancolini JC, Dios AMS, Lugones G. Feasibility of biventricular repair in right dominant unbalanced atrioventricular septal defect: a new echocardiographic metric to refine surgical decision-making. World J Pediatr Congenit Heart Surg. 2017; 8:460–467. PMID: 28696869.
Article17. Leung MP, McKay R, Smith A, Anderson RH, Arnold R. Critical aortic stenosis in early infancy. Anatomic and echocardiographic substrates of successful open valvotomy. J Thorac Cardiovasc Surg. 1991; 101:526–553. PMID: 1999947.18. Goo HW. Current trends in cardiac CT in children. Acta Radiol. 2013; 54:1055–1062. PMID: 23104372.
Article19. Mahle WT, Weinberg PM, Rychik J. Can echocardiography predict the presence or absence of endocardial fibroelastosis in infants < 1 year of age with left ventricular outflow obstruction? Am J Cardiol. 1998; 82:122–124. PMID: 9671021.20. Stranzinger E, Ensing GJ, Hernandez RJ. MR findings of endocardial fibroelastosis in children. Pediatr Radiol. 2008; 38:292–296. PMID: 18172637.
Article21. Goo HW. Myocardial delayed-enhancement CT: initial experience in children and young adults. Pediatr Radiol. 2017; 47:1452–1462. PMID: 28534155.
Article22. Rhodes LA, Colan SD, Perry SB, Jonas RA, Sanders SP. Predictors of survival in neonates with critical aortic stenosis. Circulation. 1991; 84:2325–2335. PMID: 1959189.
Article23. Lofland GK, McCrindle BW, Williams WG, Blackstone EH, Tchervenkov CI, Sittiwangkul R, et al. Critical aortic stenosis in the neonate: a multi-institutional study of management, outcomes, and risk factors. Congenital Heart Surgeons Society. J Thorac Cardiovasc Surg. 2001; 121:10–27. PMID: 11135156.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quantification of Initial Right Ventricular Dimensions by Computed Tomography in Infants with Congenital Heart Disease and a Hypoplastic Right Ventricle
- Decision of Surgical Treatment Strategy for Hypoplastic Left Ventricle with Coarctation of Aorta
- Semiautomatic Three-Dimensional Threshold-Based Cardiac Computed Tomography Ventricular Volumetry in Repaired Tetralogy of Fallot: Comparison with Cardiac Magnetic Resonance Imaging
- Three-Dimensional Endo-Cardiovascular Volume-Rendered Cine Computed Tomography of Isolated Left Ventricular Apical Hypoplasia: A Case Report and Literature Review
- Pattern Analysis of Left Ventricular Remodeling Using Cardiac Computed Tomography in Children with Congenital Heart Disease: Preliminary Results