Cancer Res Treat.
2018 Oct;50(4):1096-1105. 10.4143/crt.2017.393.
Beliefs and Intentions to Undergo Lung Cancer Screening among Korean Males
- Affiliations
-
- 1Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea. kschoi@ncc.re.kr
- 2National Cancer Control Institute, National Cancer Center, Goyang, Korea.
- KMID: 2424782
- DOI: http://doi.org/10.4143/crt.2017.393
Abstract
- PURPOSE
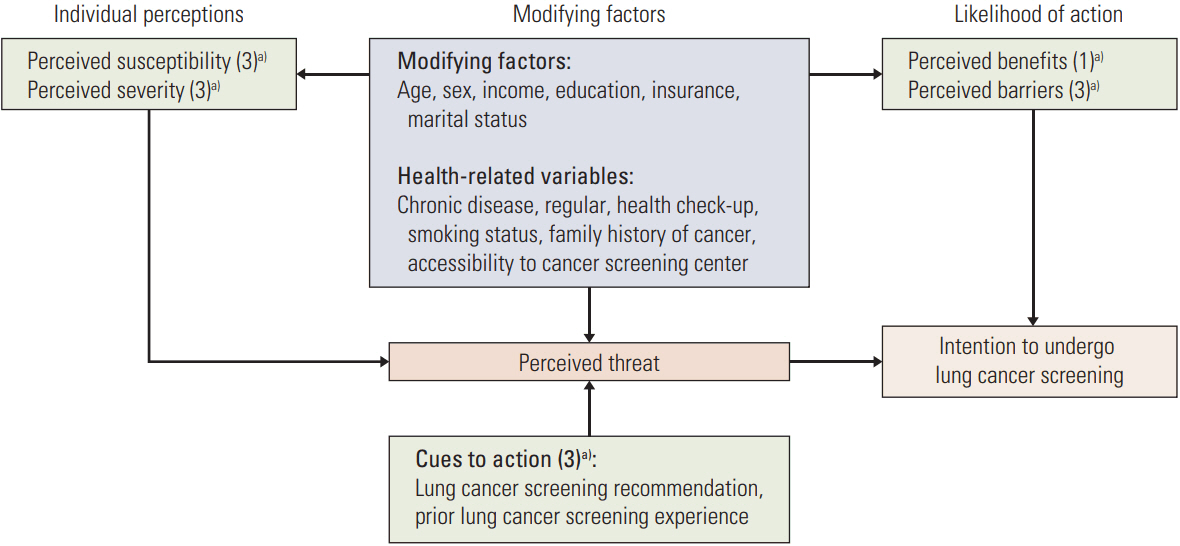
Low-dose computed tomography (LDCT) has been reported as an effective screening method for lung cancer in high-risk populations. We aimed to examine willingness to be screened among Korean males using LDCT and to determine factors associated with lung cancer screening intentions (LCS) based on the Health Belief Model (HBM).
MATERIALS AND METHODS
Data were obtained from the 2015 Korean National Cancer Screening Survey, a cross-sectional survey that utilized nationally representative random sampling. The survey included 1,730 male participants 40-74-year-old. Respondents were questioned regarding their willingness to undergo LCS and components of HBM. Factors associated with intentions to undergo screening were explored using logistic regression.
RESULTS
Among participants, 65.2% were current smokers. Among high-risk subjects, 60.6% of men reported intentions to undergo LCS, compared to 49.9% of average-risk males. Men with higher perceived susceptibility in the average- and high-risk groups were, respectively, 1.63 (95% confidence interval [CI], 1.39 to 1.91) and 2.30 (95% CI, 1.14 to 4.63) times more likely to intend to undergo LCS compared to those with lower perceived barriers. Also, men in the average- and high-risk groups with higher perceived barriers to screening were, respectively, 0.79 (95% CI, 0.68 to 0.91) and 0.52 (95% CI, 0.29 to 0.92) times less likely to intend to undergo LCS compared to those with lower perceived barriers.
CONCLUSION
Tailored interventions designed to promote accurate perceptions of susceptibility and risk, as well as to reduce perceived barriers to screening, may effectively increase adherence to recommendations for LCS among high-risk Korean men.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0. Cancer incidence and mortality worldwide: IARC CancerBase No. 11. Lyon: International Agency for Research on Cancer;2013.2. National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395–409.
Article3. Jang SH, Sheen S, Kim HY, Yim HW, Park BY, Kim JW, et al. The Korean guideline for lung cancer screening. J Korean Med Assoc. 2015; 58:291–301.
Article4. Bach PB, Mirkin JN, Oliver TK, Azzoli CG, Berry DA, Brawley OW, et al. Benefits and harms of CT screening for lung cancer: a systematic review. JAMA. 2012; 307:2418–29.5. Gohagan JK, Marcus PM, Fagerstrom RM, Pinsky PF, Kramer BS, Prorok PC, et al. Final results of the Lung Screening Study, a randomized feasibility study of spiral CT versus chest X-ray screening for lung cancer. Lung Cancer. 2005; 47:9–15.
Article6. Mettler FA Jr, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008; 248:254–63.
Article7. National Lung Screening Trial Research Team, Aberle DR, Berg CD, Black WC, Church TR, Fagerstrom RM, et al. The National Lung Screening Trial: overview and study design. Radiology. 2011; 258:243–53.
Article8. Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009; 169:2078–86.
Article9. Nhung BC, Lee YY, Yoon H, Suh M, Park B, Jun JK, et al. Intentions to undergo lung cancer screening among Korean men. Asian Pac J Cancer Prev. 2015; 16:6293–8.10. Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974; 2:354–86.
Article11. Suh M, Choi KS, Park B, Lee YY, Jun JK, Lee DH, et al. Trends in cancer screening rates among Korean men and women: results of the Korean National Cancer Screening Survey, 2004-2013. Cancer Res Treat. 2016; 48:1–10.
Article12. Centers for Disease Control and Prevention (CDC). State-specific secondhand smoke exposure and current cigarette smoking among adults: United States, 2008. MMWR Morb Mortal Wkly Rep. 2009; 58:1232–5.13. O’Rourke N, Hatcher L. A step-by-step approach to using SAS for factor analysis and structural equation modeling. 2nd ed. Cary, NC: SAS Institute Inc.;2013.14. Silvestri GA, Nietert PJ, Zoller J, Carter C, Bradford D. Attitudes towards screening for lung cancer among smokers and their non-smoking counterparts. Thorax. 2007; 62:126–30.
Article15. Tanner NT, Egede LE, Shamblin C, Gebregziabher M, Silvestri GA. Attitudes and beliefs toward lung cancer screening among US Veterans. Chest. 2013; 144:1783–7.
Article16. Cataldo JK. High-risk older smokers' perceptions, attitudes, and beliefs about lung cancer screening. Cancer Med. 2016; 5:753–9.
Article17. Schnoll RA, Bradley P, Miller SM, Unger M, Babb J, Cornfeld M. Psychological issues related to the use of spiral CT for lung cancer early detection. Lung Cancer. 2003; 39:315–25.
Article18. Jonnalagadda S, Bergamo C, Lin JJ, Lurslurchachai L, Diefenbach M, Smith C, et al. Beliefs and attitudes about lung cancer screening among smokers. Lung Cancer. 2012; 77:526–31.
Article19. Flynn AE, Peters MJ, Morgan LC. Attitudes towards lung cancer screening in an Australian high-risk population. Lung Cancer Int. 2013; 2013:789057.
Article20. Patel D, Akporobaro A, Chinyanganya N, Hackshaw A, Seale C, Spiro SG, et al. Attitudes to participation in a lung cancer screening trial: a qualitative study. Thorax. 2012; 67:418–25.
Article21. Ali N, Lifford KJ, Carter B, McRonald F, Yadegarfar G, Baldwin DR, et al. Barriers to uptake among high-risk individuals declining participation in lung cancer screening: a mixed methods analysis of the UK Lung Cancer Screening (UKLS) trial. BMJ Open. 2015; 5:e008254.
Article22. Young RP, Hopkins RJ. Increasing smokers' risk perception improves CT screening participation. Thorax. 2012; 67:834–5.
Article23. Manning WG, Marquis MS. Health insurance: the tradeoff between risk pooling and moral hazard. J Health Econ. 1996; 15:609–39.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Screening for Lung Cancer
- Impact of Awareness of Breast Density on Perceived Risk, Worry, and Intentions for Future Breast Cancer Screening among Korean Women
- Korean Americans' Beliefs about Colorectal Cancer Screening
- Responses to Overdiagnosis in Thyroid Cancer Screening among Korean Women
- The Related Factors on Cervical Cancer Screening Intention among Married Immigrant Women based on the Health Belief Model