Endovascular Treatment in Acute Ischemic Stroke: A Nationwide Survey in Korea
- Affiliations
-
- 1Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 2Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. suhsh11@yuhs.ac
- 3Severance Institute of Vascular and Metabolic Research, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2424056
- DOI: http://doi.org/10.5469/neuroint.2018.01053
Abstract
- PURPOSE
As endovascular therapy (EVT) has been approved as a treatment guideline for acute ischemic stroke (AIS), it has been increasing in Korea. We conducted a nationwide survey to evaluate the current status of EVT for patients with AIS in Korea.
MATERIALS AND METHODS
An electronic survey was sent to a representative clinician at each hospital where EVT was available in Korea. A Google survey was used to distribute the questionnaires and receive responses from October 2017 to December 2017.
RESULTS
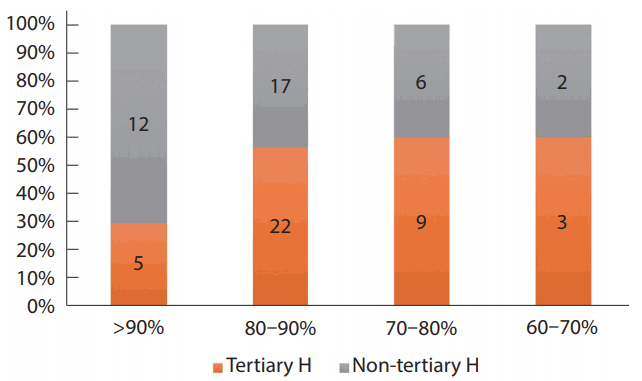
Among 120 hospitals in our society, 76 participated in this survey. In 26% of the hospitals, more than 50 annual cases of EVT were performed, and 25-50 annual cases in 37%. Fifty-six hospitals (73.7%) achieved successful recanalization (thrombolysis in cerebral infarction ≥2b) in more than 80% of patients. Computed tomography (CT) angiography was the most common imaging modality for AIS treatment, and magnetic resonance (MR) diffusion, MR-perfusion/diffusion, and perfusion CT were frequently used in order. Non-eligibility criteria for EVT included a National Institutes of Health Stroke Scale < 4 (64.5%), the absence of MR perfusion/diffusion mismatch (52.6%), and a low Alberta Stroke Program Early CT Score (42.1%). For anterior circulation stroke, 60% of Korean hospitals adopted a wider time range of "8 hours" from symptom onset, while 70% of hospitals had a time limitation of 12-24 hours for posterior circulation stroke. The most preferred EVT device was a stentriever (89.4%). In the failed cases due to underlying stenosis, 79% of Korean hospitals performed angioplasty or stenting for revascularization.
CONCLUSION
This first nationwide survey showed that most Korean hospitals conducted EVT for AIS patients according to the present guideline in the era of mechanical thrombectomy by integrating the clinical experiences of many medical institutions and specialists.
MeSH Terms
Figure
Cited by 4 articles
-
Effect of Transport Time on the Use of Reperfusion Therapy for Patients with Acute Ischemic Stroke in Korea
Jay Chol Choi, Joong-Goo Kim, Chul-Hoo Kang, Hee-Joon Bae, Jihoon Kang, Soo-Joo Lee, Jong-Moo Park, Tai Hwan Park, Yong-Jin Cho, Kyung Bok Lee, Jun Lee, Dong-Eog Kim, Jae-Kwan Cha, Joon-Tae Kim, Byung-Chul Lee, Ji-Sung Lee, Anthony S. Kim
J Korean Med Sci. 2021;36(11):e77. doi: 10.3346/jkms.2021.36.e77.A Multicenter Survey of Acute Stroke Imaging Protocols for Endovascular Thrombectomy
Byungjun Kim, Sung-Hye You, Seung Chai Jung
Neurointervention. 2021;16(1):20-28. doi: 10.5469/neuroint.2020.00199.National Trends in Medical Costs and Prognosis of Acute Ischemic Stroke Patients in Endovascular Thrombectomy Era: Analysis Using Medical Claim Data in Korea
Woo Sang Jung, Kwon-Duk Seo, Sang Hyun Suh
Neurointervention. 2022;17(3):152-160. doi: 10.5469/neuroint.2022.00234.Proposed Protocols for Artificial Intelligence Imaging Database in Acute Stroke Imaging
Minjae Kim, Seung Chai Jung, Soo Chin Kim, Bum Joon Kim, Woo-Keun Seo, Byungjun Kim
Neurointervention. 2023;18(3):149-158. doi: 10.5469/neuroint.2023.00339.
Reference
-
1. Kim JS. Stroke becomes the 3rd important cause of death in Korea; is it a time to toast? J Stroke. 2014; 16:55–56.
Article2. Hong KS, Bang OY, Kang DW, Yu KH, Bae HJ, Lee JS, et al. Stroke statistics in Korea: Part I. Epidemiology and risk factors: a report from the Korean Stroke Society and clinical research center for stroke. J Stroke. 2013; 15:2–20.
Article3. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 333:1581–1587.4. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke. The proact II study: a randomized controlled trial. Prolyse in acute cerebral thromboembolism. JAMA. 1999; 282:2003–2011.5. Smith WS, Sung G, Saver J, Budzik R, Duckwiler G, Liebeskind DS, et al. Mechanical thrombectomy for acute ischemic stroke: final results of the multi merci trial. Stroke. 2008; 39:1205–1212.6. Penumbra Pivotal Stroke Trial Investigators. The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009; 40:2761–2768.7. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.
Article8. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.9. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.
Article10. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.11. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.12. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.
Article13. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035.
Article14. Hong KS, Ko SB, Yu KH, Jung C, Park SQ, Kim BM, et al. Update of the Korean clinical practice guidelines for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2016; 18:102–113.
Article15. Suh SH. The annual trends between neurointerventional and neurosurgical procedures in Korea: analysis using hira data from 2010 to 2016. Neurointervention. 2017; 12:77–82.
Article16. Lee YM, Hwang SM, Kim EH, Lee DG, Shim JH, Suh DC. Current status of neurointerventional activities in Korea. Neurointervention. 2013; 8:65–67.
Article17. Chun CB, Kim SY, Lee JY, Lee SY. Republic of Korea. Health system review. Health Syst Transit. 2009; 11:1–184.18. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110.
Article19. Brinjikji W, Starke RM, Murad MH, Fiorella D, Pereira VM, Goyal M, et al. Impact of balloon guide catheter on technical and clinical outcomes: a systematic review and meta-analysis. J Neurointerv Surg. 2018; 10:335–339.
Article20. Holmstedt CA, Turan TN, Chimowitz MI. Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment. Lancet Neurol. 2013; 12:1106–1114.
Article21. Kim JS, Nah HW, Park SM, Kim SK, Cho KH, Lee J, et al. Risk factors and stroke mechanisms in atherosclerotic stroke: intracranial compared with extracranial and anterior compared with posterior circulation disease. Stroke. 2012; 43:3313–3318.22. Kang DH, Kim YW, Hwang YH, Park SP, Kim YS, Baik SK. Instant reocclusion following mechanical thrombectomy of in situ thromboocclusion and the role of low-dose intra-arterial tirofiban. Cerebrovasc Dis. 2014; 37:350–355.
Article23. Ernst M, Butscheid F, Fiehler J, Wittkugel O, Alfke K, Jansen O, et al. Glycoprotein IIb/IIIa inhibitor bridging and subsequent endovascular therapy in vertebrobasilar occlusion in 120 patients. Clin Neuroradiol. 2016; 26:169–175.
Article24. Yoon W, Kim SK, Park MS, Kim BC, Kang HK. Endovascular treatment and the outcomes of atherosclerotic intracranial stenosis in patients with hyperacute stroke. Neurosurgery. 2015; 76:680–686. discussion 686.
Article25. Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Yoo J. Stenting as a rescue treatment after failure of mechanical thrombectomy for anterior circulation large artery occlusion. Stroke. 2016; 47:2360–2363.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Acute Ischemic Stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Epidemiology and Functional Outcome of Acute Stroke Patients in Korea Using Nationwide data
- Rescue Endovascular Treatment to Prevent Neurological Deterioration in Acute Symptomatic Bilateral Vertebral Artery Occlusion
- Reperfusion therapy in acute ischemic stroke