J Korean Orthop Assoc.
2017 Dec;52(6):529-536. 10.4055/jkoa.2017.52.6.529.
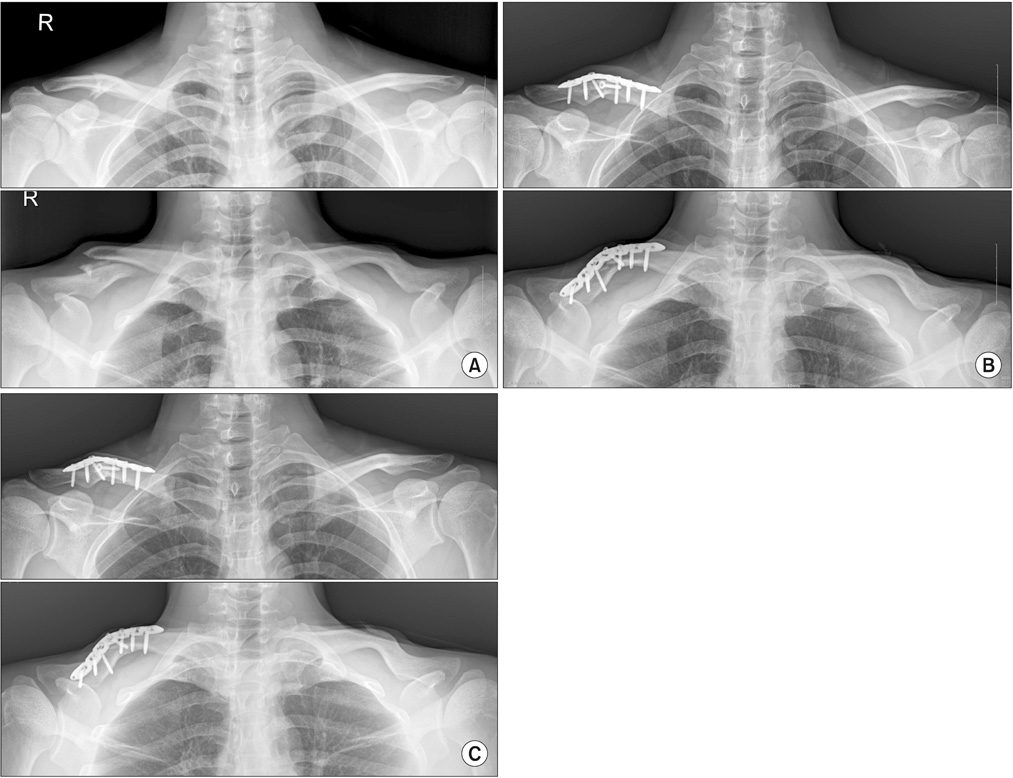
Surgical Treatment of Clavicle Midshaft Fractures Using a Locking Compression Plate: Conventional Open Reduction and Plating with Internal Fixation versus Minimal Invasive Plate Osteosynthesis
- Affiliations
-
- 1Department of Orthopaedic Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. bakpaker@hanmail.net
- KMID: 2421346
- DOI: http://doi.org/10.4055/jkoa.2017.52.6.529
Abstract
- PURPOSE
The purpose of this study was to make a comparison between minimally invasive plate osteosynthesis (MIPO) and conventional open reduction and plating (COP) to treat displaced clavicle shaft fractures.
MATERIALS AND METHODS
We retrospectively reviewed patients with clavicle shaft fractures, who underwent surgery by using a locking plate between May 2011 and August 2016. The inclusion criteria were: 1) displaced ≥20 mm, 2) acute fracture of less than 2 weeks from injury, 3) skeletally mature patients, and 4) follow-up of at least 6 months. The demographic data and clinical outcomes, including operation time, fracture union rate, union time, shortening of clavicle, shoulder functional score (University of California at Los Angeles score), and complications, were evaluated. The clavicle length ratio was measured to evaluate shortening. We compared the clinical outcomes between two groups: the COP group that included 21 patients treated with COP (group 1) and the MIPO group that included 19 patients treated with MIPO (group 2).
RESULTS
In all cases, union of fractures was successfully achieved. The mean union time was 14.9 weeks in group 1 and 14.2 weeks in group 2 (p=0.713). Both groups had good functional scores (34.0 vs. 33.7, p=0.658). Group 2 had shorter operation time and less bleeding. There were no secondary interventions or infections. The clavicle length ratio was similar between the two groups; and all patients in both groups showed no shortening (less than 3%). There were no implant failures in either group.
CONCLUSION
The clinical and radiologic outcomes were satisfactory in both groups. We suggest that MIPO may be a safe and effective method for displaced clavicle shaft fractures.
Figure
Cited by 1 articles
-
Surgical Results of Minimally Invasive Percutaneous Plate Fixation in the Treatment of Clavicle Shaft Fracture
Seong-Ho Yoo, Suk-Woong Kang, Jae-Seung Seo
J Korean Fract Soc. 2019;32(1):21-26. doi: 10.12671/jkfs.2019.32.1.21.
Reference
-
1. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997; 79:537–539.
Article2. Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: a prospective study of 222 patients. Acta Orthop. 2005; 76:496–502.3. Ferran NA, Hodgson P, Vannet N, Williams R, Evans RO. Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial. J Shoulder Elbow Surg. 2010; 19:783–789.
Article4. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013; 95:1576–1584.5. Chu CM, Wang SJ, Lin LC. Fixation of mid-third clavicular fractures with knowles pins: 78 patients followed for 2-7 years. Acta Orthop Scand. 2002; 73:134–139.
Article6. Chuang TY, Ho WP, Hsieh PH, Lee PC, Chen CH, Chen YJ. Closed reduction and internal fixation for acute midshaft clavicular fractures using cannulated screws. J Trauma. 2006; 60:1315–1320. discussion 1320-1.
Article7. Shen WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury. 1999; 30:497–500.
Article8. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004; 86:1359–1365.
Article9. Evidence-Based Orthopaedic Trauma Working Group. Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005; 19:504–507.10. Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007; 89:1–10.11. Böstman O, Manninen M, Pihlajamäki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma. 1997; 43:778–783.12. Wijdicks FJ, Van der Meijden OA, Millett PJ, Verleisdonk EJ, Houwert RM. Systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg. 2012; 132:617–625.
Article13. Der Tavitian J, Davison JN, Dias JJ. Clavicular fracture non-union surgical outcome and complications. Injury. 2002; 33:135–143.
Article14. Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005; 36:530–538.15. Röderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2010; 24:400–406.
Article16. Kim JW, Oh CW, Byun YS, Kim JJ, Park KC. A prospective randomized study of operative treatment for noncomminuted humeral shaft fractures: conventional open plating versus minimal invasive plate osteosynthesis. J Orthop Trauma. 2015; 29:189–194.17. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007; 21:S1–S133.18. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986; 68:1136–1144.
Article19. Kadakia AP, Rambani R, Qamar F, McCoy S, Koch L, Venkateswaran B. Titanium elastic stable intramedullary nailing of displaced midshaft clavicle fractures: a review of 38 cases. Int J Shoulder Surg. 2012; 6:82–85.
Article20. Kim JW, Kim JJ. Radiation exposure to the orthopaedic surgeon during fracture surgery. J Korean Orthop Assoc. 2010; 45:107–113.
Article21. Jiang H, Qu W. Operative treatment of clavicle midshaft fractures using a locking compression plate: comparison between mini-invasive plate osteosynthesis (MIPPO) technique and conventional open reduction. Orthop Traumatol Surg Res. 2012; 98:666–671.
Article22. Sohn HS, Kim WJ, Shon MS. Comparison between open plating versus minimally invasive plate osteosynthesis for acute displaced clavicular shaft fractures. Injury. 2015; 46:1577–1584.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Outcomes of Locking Compression Plate Fixation through Minimally Invasive Percutaneous Plate Osteosynthesis in the Treatment of Distal Tibia Fracture
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Treatment of Femur Supracondylar Fracture with Locking Compression Plate
- Operative Treatment of Clavicle Midshaft Fractures: Comparison between Reconstruction Plate and Reconstruction Locking Compression Plate
- Comparison between Accurate Anatomical Reduction and Unsuccessful Reduction with a Remaining Gap after Open Reduction and Plate Fixation of Midshaft Clavicle Fracture