J Korean Fract Soc.
2012 Apr;25(2):117-122. 10.12671/jkfs.2012.25.2.117.
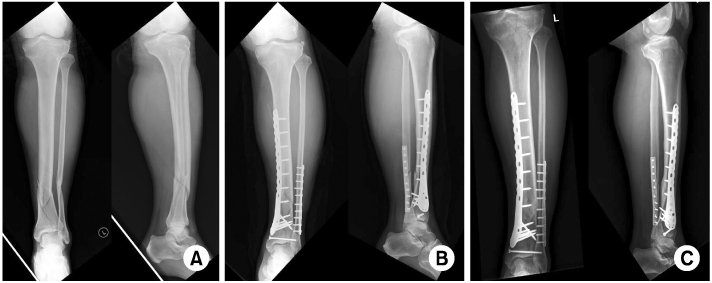
Clinical Outcomes of Locking Compression Plate Fixation through Minimally Invasive Percutaneous Plate Osteosynthesis in the Treatment of Distal Tibia Fracture
- Affiliations
-
- 1Department of Orthopedic Surgery, Dankook University Medical College, Cheonan, Korea. m3artist@hanmail.net
- KMID: 2015454
- DOI: http://doi.org/10.12671/jkfs.2012.25.2.117
Abstract
- PURPOSE
To analyze the clinical results of operative treatment of distal tibia fracture with locking compression plate fixation through a minimally invasive percutaneous plate osteosynthesis technique.
MATERIALS AND METHODS
The subjects were 46 patients (conventional open surgery: 22 patients, minimally invasive percutaneous plate osteosynthesis: 24 patients) with fracture of the distal tibia who were treated with plating between November 2006 and June 2010. The time of bony union, complications, range of motion, and clinical functional outcome (according to American Orthopedic Foot and Ankle Society, AOFAS) were investigated.
RESULTS
In the minimally invasive percutaneous plate osteosynthesis group, the average union time was 14.3 weeks, postoperative range of motion was an average of 55.2, average AOFAS was 96.9, and incidence of complications was 20.8%. In the open surgery group, the average union time was 18.9 weeks, postoperative range of motion was an average of 49.1, average AOFAS was 83.8, and incidence of complications was 32.6%. There were statistically significant differences (p<0.05).
CONCLUSION
Surgical treatment with locking compression plate fixation through the minimally invasive percutaneous plate osteosynthesis technique showed favorable results regarding its union time, postoperative functional outcome, and incidence of complications. The locking compression plate fixation through minimally invasive percutaneous plate osteosynthesis technique can be an effective treatment option.
Figure
Cited by 1 articles
-
Minimally Invasive Plate Osteosynthesis for Fractures of Distal Tibia
Tae Hun Kim, So Hak Chung
Kosin Med J. 2014;29(1):23-29. doi: 10.7180/kmj.2014.29.1.23.
Reference
-
1. Baumgaertel F, Buhl M, Rahn BA. Fracture healing in biological plate osteosynthesis. Injury. 1998. 29:Suppl 3. C3–C6.
Article2. Chang SA, Ahn HS, Byun YS, Kim JH, Bang HH, Kwon DY. Minimally invasive plate osteosynthesis in unstable fractures of the distal tibia. J Korean Fract Soc. 2005. 18:155–159.
Article3. Chrisovitsinos JP, Xenakis T, Papakostides KG, Skaltsoyannis N, Grestas A, Soucacos PN. Bridge plating osteosynthesis of 20 comminuted fractures of the femur. Acta Orthop Scand Suppl. 1997. 275:72–76.
Article4. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000. (375):69–77.
Article5. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004. 18:488–493.
Article6. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury. 1997. 28:Suppl 1. A7–A12.
Article7. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999. 13:401–406.
Article8. Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003. 34:Suppl 2. B63–B76.
Article9. Ha SH, Lee JY, Sohn HM, Shin MK. Minimally Invasive Percutaneous Plate Fixation for Distal Tibia Shaft Fractures. J Korean Orthop Assoc. 2004. 39:386–390.
Article10. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007. 38:365–370.
Article11. Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia--results in 20 patients. Injury. 2006. 37:877–887.
Article12. Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997. 28:Suppl 1. A42–A47.
Article13. Helfet DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect. 2004. 53:471–475.14. Ibrahim T, Beiri A, Azzabi M, Best AJ, Taylor GJ, Menon DK. Reliability and validity of the subjective component of the American Orthopaedic Foot and Ankle Society clinical rating scales. J Foot Ankle Surg. 2007. 46:65–74.
Article15. Kellam JF, Waddell JP. Fractures of the distal tibial metaphysis with intra-articular extension--the distal tibial explosion fracture. J Trauma. 1979. 19:593–601.
Article16. Lee HS, Kim JJ, Oh SK, Ahn HS. Treatment of distal tibial metaphyseal fracture using MIPPO technique. J Korean Foot Ankle Soc. 2004. 8:166–170.17. Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004. 28:159–162.
Article18. Mast JW, Spiegel PG, Pappas JN. Fractures of the tibial pilon. Clin Orthop Relat Res. 1988. (230):68–82.
Article19. Melis GC, Sotgiu F, Lepori M, Guido P. Intramedullary nailing in segmental tibial fractures. J Bone Joint Surg Am. 1981. 63:1310–1318.
Article20. Moore TJ, Watson T, Green SA, Garland DE, Chandler RW. Complications of surgically treated supracondylar fractures of the femur. J Trauma. 1987. 27:402–406.
Article21. Oh CW, Oh JK, Jeon IH, et al. Minimally invasive percutaneous plate stabilization of proximal tibial fractures. J Korean Fract Soc. 2004. 17:224–229.
Article22. Park KC, Park YS. Minimally invasive plate osteosynthesis for distal tibial metaphyseal fracture. J Korean Fract Soc. 2005. 18:264–268.
Article23. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002. 84:1093–1110.24. Rüedi TP, Sommer C, Leutenegger A. New techniques in indirect reduction of long bone fractures. Clin Orthop Relat Res. 1998. (347):27–34.25. Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993. (292):108–117.26. Tong GO, Bavonratanavech S. AO manual of fracture management. Minimally invasive plate osteosynthesis (MIPO). 2007. 1st ed. Stuttgart: Thieme;3–45. 66–118. 305–325.27. Whiteside LA, Lesker PA. The effects of extraperiosteal and subperiosteal dissection. II. On fracture healing. J Bone Joint Surg Am. 1978. 60:26–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of the Result Treated with Locking Compression Plate-Distal Tibia and Zimmer Periarticular Locking Plate in Distal Tibia Fracture
- Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures
- Minimally Invasive Osteosynthesis with Locking Compression Plate for Distal Tibia Fractures
- Treatment of Distal Femur Fracture with Minimally Invasive Locking Compression Plate Osteosynthesis
- Minimally Invasive Percutaneous Plate Osteosynthesis Using Periarticular Plate for Distal Tibial Fractures