J Korean Acad Oral Health.
2018 Sep;42(3):67-76. 10.11149/jkaoh.2018.42.3.67.
Dental neglect and related factors in mothers
- Affiliations
-
- 1Department of Preventive and Public Health Dentistry, College of Dentistry, Wonkwang University, Iksan, Korea. smagn@wonkwang
- KMID: 2421267
- DOI: http://doi.org/10.11149/jkaoh.2018.42.3.67
Abstract
OBJECTIVES
The purpose of this study was to determine the level of dental neglect in mothers and their children and to analyze the factors that were associated with it.
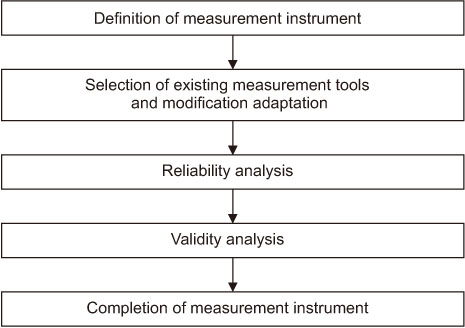
METHODS
The subjects included in this study were 431 mothers with preschool children. The participants were given a self-report questionnaire for the study. The survey collected data on sociodemographic characteristics and dental neglect. For dental neglect, the Adelaide dental neglect scale was used for measurement.
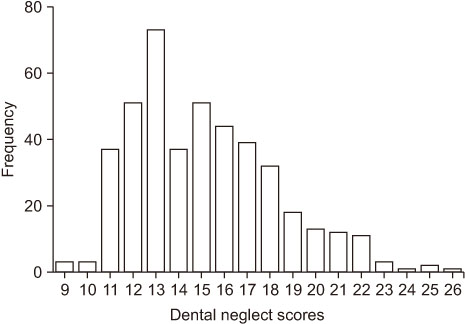
RESULTS
The percentage of mothers with a high level (≥15 points) of dental neglect was 52.7%. In terms of dental neglect in mothers and their children, 37.1% showed feeding of snacks before and after meals, followed by postponement of dental treatment for mothers at 22.8%, and dental treatment postponed due to children 21.7%. The demographic factors affecting the mother's dental neglect were found to be age of the mother, whether the mother was employed or not, and household income. The lower was the age of the mother, the higher was the level of dental neglect. In addition, when mothers had jobs, dental neglect was high, and the lower was the household income, the higher was the level of dental neglect.
CONCLUSIONS
The level of dental neglect for mothers and their children was found to be high. Thus, this should be considered in the design of national oral health promotion strategies for children. In addition, the importance of dental neglect should be emphasized.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
어머니의 구강건강문해력: I. 인구사회학적 특성의 영향
Hyun-Jeong Ju, Hyo-Won Oh, Heung-Soo Lee
J Korean Acad Oral Health. 2021;45(3):111-118. doi: 10.11149/jkaoh.2021.45.3.111.
Reference
-
1. Hong EJ. The effects of childhood maltreatment experiences on children's phychosocial development. J Korean Counc Child Rights. 1998; 1:97–111.2. Kim KH. Effects of child abuse and neglect on child development. J Soc Sci. 2009; 24:27–45.3. Kang SW. A study on the actual condition of athletes medical neglect and medically neglected athletes' social-psychological, behavioral characteristics. Korean J Phys Educ. 2011; 50:71–86.4. Song HA, Sun GY. A study on elder mistreatment 2: empirical investigation of elder abuse and neglect among the elderly. J Korean Home Econ Assoc. 1998; 36:145–159.5. Bae HO, Kang JY. Repeat of neglect and correlates. Health Soc Welf Rev. 2015; 35:455–474.6. Welbury R. Dental neglect, child maltreatment, and role of the dental profession. Contemp Clin Dent. 2016; 7:285–286.
Article7. Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R. World Health Organization (WHO): In World report on violence and health. Geneva: World Health Organization;2002. p. 1–54.8. American Academy of Pediatrics Committee on Child Abuse and Neglect. American Academy of Pediatric Dentistry. American Academy of Pediatric Dentistry Council on Clinical Affairs. Guideline on oral and dental aspects of child abuse and neglect. Pediatr Dent. 2008-2009; 30:86–89.9. Massoni AC, Ferreria AM, Aragão AK, de Menezes VA, Colares V. Orofacial aspects of childhood abuse and dental negligence. Cien Saude Colet. 2010; 15:403–410.10. Lourenco CB, Saintrain MV, Vieira AP. Child, neglect and oral health. BMC Pediatr. 2013; 11. 18. [Epub]. DOI: 10.1186/1471-2431-13-188.
Article11. Thomson WM, Spencer AJ, Gaughwin A. Testing a child dental neglect scale in South Australia. Community Dent Oral Epidemiol. 1996; 24:351–356.
Article12. Joyce M. Dental neglect and professional responsibilities. Dental Nursing. 2013; 346–349.
Article13. Thomson WM, Locker D. Dental neglect and dental health among 26-year-olds in the Dunedin multidisciplinary health and development study. Community Dent Oral Epidemiol. 2000; 28:414–418.
Article14. Skaret E, Astrøm AN, Haugejordon O, Klock KS, Trovik TA. Assessment of the reliability and validity of dental neglect scale in Norwegian adults. Community Dent Health. 2007; 24:247–252.15. Kvist T, Zedrén-Sunemo J, Graca E, Dahllöf G. Is treatment general anaesthesia associated with dental neglect and dental disability among caries active preschool children? Eur Arch Paediatr Dent. 2014; 15:327–332.
Article16. Coolidge T, Heima M, Johnson EK, Weinstein P. The dental neglect scale in adolescents. BMC Oral Health. 2009; 01. 5. [Epub]. DOI: 10.1186/1472-6831-9-2.
Article17. Sarri G, Evans P, Stansfeld S, Marcences W. A school-based epidemiological study of dental neglect among adolescents in a deprived area of the UK. Br Dent J. 2012; 11. [Epub]. DOI: 10.1038/sj.bdj.2012.1042.
Article18. McGrath C, Sham AS, Ho DK, Wong JH. The impact of dental neglect on oral health: a population based study in Hong Kong. Int Dent J. 2007; 57:3–8.
Article19. Harris J. Dental neglect in children. Paediatr Child Health. 2012; 22:476–482.
Article20. Nasseh K, Vujicic M. The effect of growing income disparities on U.S. adults' dental care utilization. J Am Dent Assoc. 2014; 145:435–442.
Article21. Friedman PK, Kaufman LB, Karpas SL. Oral health disparity in older adults: dental decay and tooth loss. Dent Clin North Am. 2014; 58:757–770.22. Luchi CA, Peres KG, Bastos JL, Peres MA. Inequalities in self-rated oral health in adults. Rev Saude Publica. 2013; 47:740–751.23. Lee HS. Association between dental health belief and dental healthrelated behavior in mothers and childrens. J Korean Acad Oral Health. 1996; 20:11–30.24. Sim SJ, Kim JB, Baeg DI, Mun HS. The influence of mothers' oral health knowledge on incidence and treatment of deciduous dental caries among their children. J Korean Acad Oral Health. 2003; 27:415–434.25. You RK, Lee KH, Ra JY, Lee DJ. Prevalence of severe early childhood caries and feeding practices in preschool children in Iksan city. J Korean Acad Pediatr Dent. 2007; 34:383–389.26. Guimarães AO, Costa ICC, Oliveira ALS. As origens, objetivos e razões de ser da odontologia para bebês. JBP J Bras Odontopediatr Odontol Bebê. 2003; 6:83–86.27. Bhatia SK, Maguire SA, Chadwick BL, Hunter ML, Harris JC, Tempest V, et al. Characteristics of child dental neglect: a systematic review. J Dent. 2014; 42:229–239.
Article28. Bennett DS, Sullivan MW, Thompson SM. Early child neglect: does it predict obesity or underweight in later childhood? Child Maltreat. 2010; 15:250–254.
Article29. Noble F, Dickie J, Conway DI. Systematic review highlights difficulty in clearly identifying dental neglect in children. Evid Based Dent. 2014; 15:3–4.
Article30. Gurunathan D, Shanmuaavel AK. Dental neglect among children in Chennai. J Indian Soc Pedod Prev Dent. 2016; 34:364–369.
Article31. Monse B, Heinrich-Weltzien R, Benzian H, Homlgren C, van Palenstein Helderman W. PUFA—an index of clinical consequences of untreated dental caries. Community Dent Oral Epidemiol. 2010; 38:77–82.32. Loochtan RM, Bross DC, Domoto PK. Dental neglect in children: definition, legal aspects, and challenges. Pediatr Dent. 1986; 8:113–116.33. Sarri G, Marcenes W. Child dental neglect: is it a neglected area in the UK? Br Dent J. 2012; 213:103–104.
Article34. Statistics Korea. Korea Statistics Information System (KOSIS), Statistics DB [internet]. cited 2017 July 21. http://kostat.go.kr/portal/korea/kor_nw/2/3/1/index.board?bmode=read&bSeq=&aSeq=361185&pageNo=1&rowNum=10&navCount=10&currPg=&starget=title&sTxt=.35. Ministry of Health and Welfare. Korean national oral health survey 2012. Summary Report. Seoul: Ministry of Health and Welfare;2012. p. 61.