J Korean Soc Radiol.
2018 Oct;79(4):204-207. 10.3348/jksr.2018.79.4.204.
A Case Report of Male Occult Breast Cancer Manifested as Superior Vena Cava Syndrome
- Affiliations
-
- 1Department of Radiology, Chung-Ang University Medical Center, Seoul, Korea.
- 2Department of Radiology and Thyroid Center, Chung-Ang University Medical Center, Seoul, Korea. su3ha5@hanmail.net
- 3Department of Pathology, Chung-Ang University Medical Center, Seoul, Korea.
- 4Department of Internal Medicine, Chung-Ang University Medical Center, Seoul, Korea.
- KMID: 2421223
- DOI: http://doi.org/10.3348/jksr.2018.79.4.204
Abstract
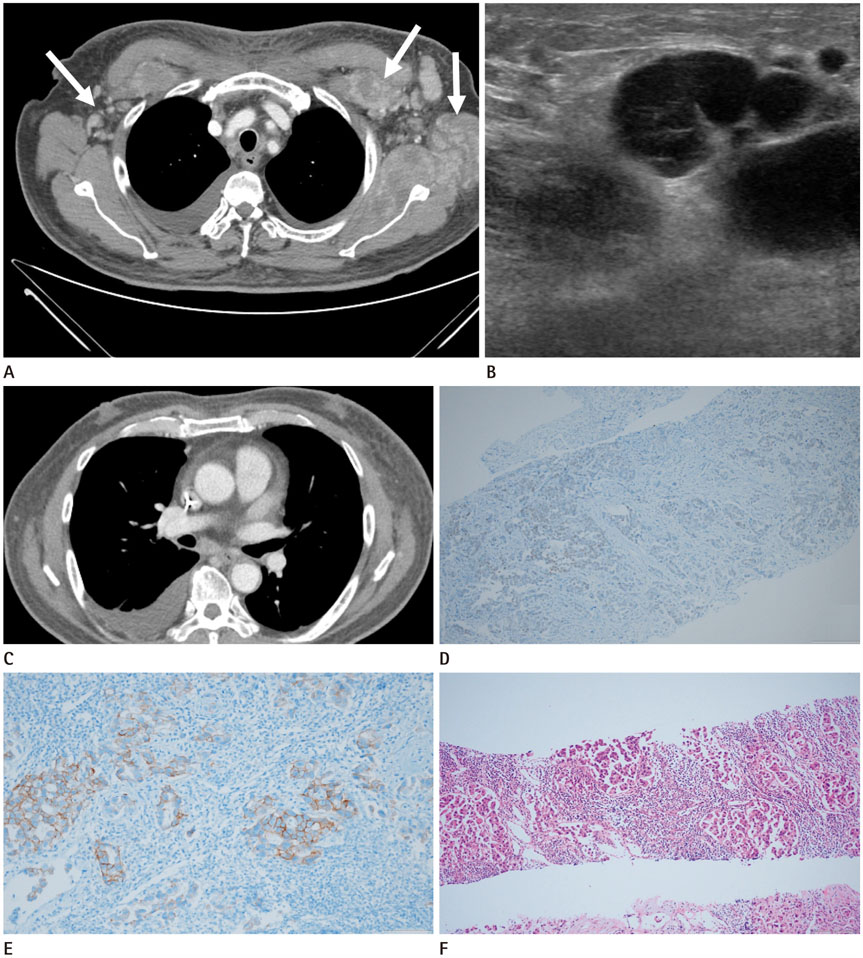
- Occult breast cancer (OBC) is an asymptomatic condition. We report a case of OBC in a 72-year-old male patient who presented with severe dyspnea and upper extremity swelling. Computed tomography scan showed multiple lymph node enlargements in the supraclavicular and infraclavicular areas, and ultrasound scan showed multiple axillary lymph node enlargements. Based on the radiological findings, clinicians suspected lymphoma or disseminated metastasis from unknown primary malignancies. However, the axillary biopsy specimen revealed invasive breast cancer with hormonal receptor positivity.
MeSH Terms
Figure
Reference
-
1. Sasco AJ, Lowenfels AB, Pasker-de Jong P. Review article: epidemiology of male breast cancer. A meta-analysis of published case-control studies and discussion of selected aetiological factors. Int J Cancer. 1993; 53:538–549.
Article2. Chen L, Chantra PK, Larsen LH, Barton P, Rohitopakarn M, Zhu EQ, et al. Imaging characteristics of malignant lesions of the male breast. Radiographics. 2006; 26:993–1006.
Article3. Baron PL, Moore MP, Kinne DW, Candela FC, Osborne MP, Petrek JA. Occult breast cancer presenting with axillary metastases. Updated management. Arch Surg. 1990; 125:210–214.4. Weiss JR, Moysich KB, Swede H. Epidemiology of male breast cancer. Cancer Epidemiol Biomarkers Prev. 2005; 14:20–26.5. Burga AM, Fadare O, Lininger RA, Tavassoli FA. Invasive carcinomas of the male breast: a morphologic study of the distribution of histologic subtypes and metastatic patterns in 778 cases. Virchows Arch. 2006; 449:507–512.
Article6. Giordano SH. A review of the diagnosis and management of male breast cancer. Oncologist. 2005; 10:471–479.
Article7. He M, Liu H, Jiang Y. A Case report of male occult breast cancer first manifesting as axillary lymph node metastasis with part of metastatic mucinous carcinoma. Medicine (Baltimore). 2015; 94:e1038.
Article8. Sohn G, Son BH, Lee SJ, Kang EY, Jung SH, Cho SH, et al. Treatment and survival of patients with occult breast cancer with axillary lymph node metastasis: a nationwide retrospective study. J Surg Oncol. 2014; 110:270–274.
Article9. Leonard RC, Mansi JL, Keerie C, Yellowlees A, Crawford S, Benstead K, et al. A randomised trial of secondary prophylaxis using granulocyte colony-stimulating factor ('sprog' trial) for maintaining dose intensity of standard adjuvant chemotherapy for breast cancer by the anglo-celtic cooperative group and ncrn. Ann Oncol. 2015; 26:2437–2441.
Article10. Hur SM, Cho DH, Lee SK, Choi MY, Bae SY, Koo MY, et al. Occult breast cancers manifesting as axillary lymph node metastasis in men: a two-case report. J Breast Cancer. 2012; 15:359–363.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Superior Vena Cava Syndrome
- Superior vena cava syndrome secondary to hickman catheter in the advanced cervical cancer patient treated with concurrent chemoradiotherapy: A case report
- A case of Behcet's syndrome with superior vena cava syndrome
- One Case of Intrathoracic Goiter Associated with Superior Vena Cava Syndrome
- A Case of Behcet's Disease with Superior Vena Cava Syndrome