Chonnam Med J.
2018 Sep;54(3):167-172. 10.4068/cmj.2018.54.3.167.
Effects of Ivabradine on Left Ventricular Systolic Function and Cardiac Fibrosis in Rat Myocardial Ischemia-Reperfusion Model
- Affiliations
-
- 1Division of Cardiology, Chonnam National University Hospital, Cardiovascular Convergence Research Center Nominated by Korea Ministry of Health and Welfare, Gwangju, Korea. hyj200@hanmail.net
- KMID: 2420884
- DOI: http://doi.org/10.4068/cmj.2018.54.3.167
Abstract
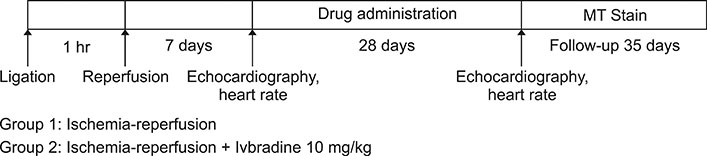
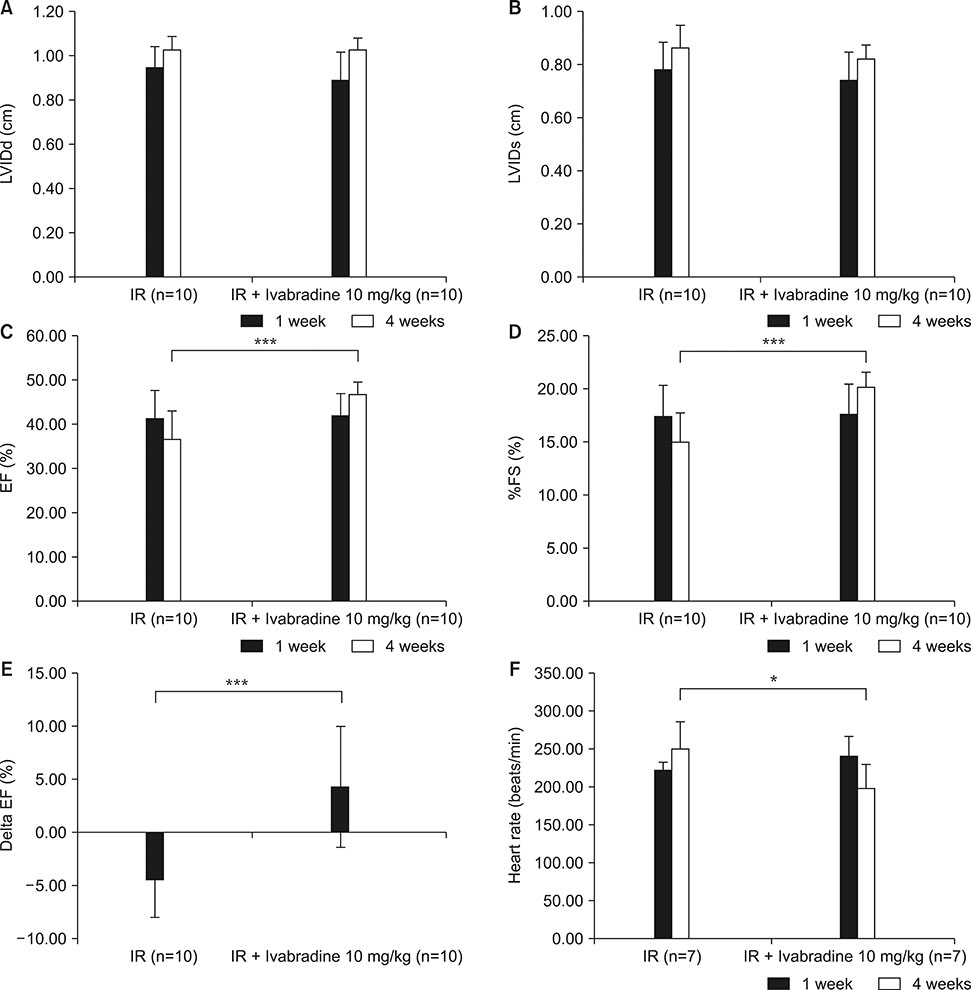
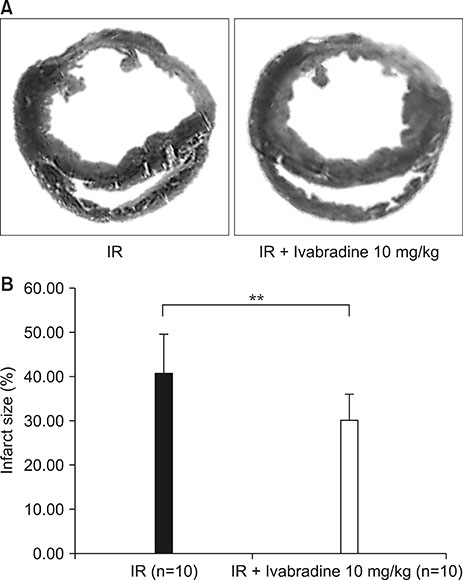
- We evaluated the effects of Ivabradine on left ventricle (LV) ejection fraction (EF) and LV infarcted tissue in the rat myocardial ischemia-reperfusion model. Twenty rats were randomly assigned to group 1 (ischemia-reperfusion, no treatment, n=10) and group 2 (ischemia-reperfusion + Ivabradine 10 mg/kg, n=10). Ivabradine was administered for 28 days. Echocardiography was performed at 7 days and at 28 days after the induction of ischemia-reperfusion injury. Cardiac fibrosis induced by ischemia-reperfusion injury was evaluated by Masson's trichrome staining. The infarct size was quantified using the Image J program. At the 28-day follow-up, LVEF was significantly higher (36.02±6.16% vs. 45.72±2.62%, p<0.001) and fractional shortening was significantly higher (15.23±2.84% vs. 20.13±1.38%, p<0.001) in group 2 than group 1. Delta (28 day minus 7 day) EF was significantly higher in group 2 than group 1 (−4.36±3.49% vs. 4.31±5.63%, p<0.001). Also, heart rate (beats/min) was significantly lower in group 2 than group 1 (251.67±25.19 vs. 199.29±31.33, p=0.025). Group 2 had a smaller infarct size (40.70±8.94% vs. 30.19±5.89%, p<0.01) than group 1 at 28-day follow-up. Oral administration of Ivabradine could improve LV systolic function and reduce infarcted tissue area in rat myocardial ischemia-reperfusion model.
MeSH Terms
Figure
Reference
-
1. Anderson JL, Morrow DA. Actue myocardial infarction. N Engl J Med. 2017; 376:2053–2064.2. Davies MJ, Thomas AC. Plaque fissuring–the cause of acute myocardial infarction, sudden ischaemic death, and crescendo angina. Br Heart J. 1985; 53:363–373.
Article3. Roe MT, Messenger JC, Weintraub WS, Cannon CP, Fonarow GC, Dai D, et al. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol. 2010; 56:254–263.
Article4. Kim JH, Chae SC, Oh DJ, Kim HS, Kim YJ, Ahn Y, et al. Korea Acute Myocardial Infarction-National Institutes of Health Registry Investigators. Multicenter cohort study of acute myocardial infarction in Korea: interim analysis of the Korea acute myocardial infarction registry-National Institutes of Health Registry. Circ J. 2016; 80:1427–1436.
Article5. Teo KK, Yusuf S, Furberg CD. Effects of prophylactic antiarrhythmic drug therapy in acute myocardial infarction. An overview of results from randomized controlled trials. JAMA. 1993; 270:1589–1595.
Article6. Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001; 357:1385–1390.
Article7. Verma S, Strauss M. Angiotensin receptor blockers and myocardial infarction. BMJ. 2004; 329:1248–1249.
Article8. Tardif JC, O'Meara E, Komajda M, Böhm M, Borer JS, Ford I, et al. SHIFT Investigators. Effects of selective heart rate reduction with ivabradine on left ventricular remodelling and function: results from the SHIFT echocardiography substudy. Eur Heart J. 2011; 32:2507–2515.
Article9. Borer JS, Böhm M, Ford I, Robertson M, Komajda M, Tavazzi L, et al. SHIFT Investigators. Efficacy and safety of ivabradine in patients with severe chronic systolic heart failure (from the SHIFT study). Am J Cardiol. 2014; 113:497–503.
Article10. Mehta RH, Harjai KJ, Grines L, Stone GW, Boura J, Cox D, et al. Primary Angioplasty in Myocardial Infarction (PAMI) Investigators. Sustained ventricular tachycardia or fibrillation in the cardiac catheterization laboratory among patients receiving primary percutaneous coronary intervention: incidence, predictors, and outcomes. J Am Coll Cardiol. 2004; 43:1765–1772.
Article11. Ng FS, Shadi IT, Peters NS, Lyon AR. Selective heart rate reduction with ivabradine slows ischaemia-induced electrophysiological changes and reduces ischaemia-reperfusion-induced ventricular arrhythmias. J Mol Cell Cardiol. 2013; 59:67–75.
Article12. Fliss H, Gattinger D. Apoptosis in ischemic and reperfused rat myocardium. Circ Res. 1996; 79:949–956.
Article13. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978; 58:1072–1083.
Article14. Yue TL, Wang C, Gu JL, Ma XL, Kumar S, Lee JC, et al. Inhibition of extracellular signal-regulated kinase enhances Ischemia/Reoxygenation-induced apoptosis in cultured cardiac myocytes and exaggerates reperfusion injury in isolated perfused heart. Circ Res. 2000; 86:692–699.
Article15. Ferrari R, Balla C, Malagù M, Guardigli G, Morciano G, Bertini M, et al. Reperfusion damage: a story of success, failure, and hope. Circ J. 2017; 81:131–141.
Article16. Piper HM, Meuter K, Schäfer C. Cellular mechanisms of ischemia-reperfusion injury. Ann Thorac Surg. 2003; 75:S644–S648.
Article17. Witt BJ, Jacobsen SJ, Weston SA, Killian JM, Meverden RA, Allison TG, et al. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004; 44:988–996.
Article18. Beltrami AP, Barlucchi L, Torella D, Baker M, Limana F, Chimenti S, et al. Adult cardiac stem cells are multipotent and support myocardial regeneration. Cell. 2003; 114:763–776.
Article19. Segers VF, Lee RT. Stem-cell therapy for cardiac disease. Nature. 2008; 451:937–942.
Article20. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2016; 68:1476–1488.21. Yusuf S, Camm AJ. Sinus tachyarrhythmias and the specific bradycardic agents: a marriage made in heaven? J Cardiovasc Pharmacol Ther. 2003; 8:89–105.
Article22. Thollon C, Cambarrat C, Vian J, Prost JF, Peglion JL, Vilaine JP. Electrophysiological effects of S 16257, a novel sino-atrial node modulator, on rabbit and guinea-pig cardiac preparations: comparison with UL-FS 49. Br J Pharmacol. 1994; 112:37–42.
Article23. Sulfi S, Timmis AD. Ivabradine–the first selective sinus node I(f) channel inhibitor in the treatment of stable angina. Int J Clin Pract. 2006; 60:222–228.
Article24. Albaladejo P, Carusi A, Apartian A, Lacolley P, Safar ME, Bénétos A. Effect of chronic heart rate reduction with ivabradine on carotid and aortic structure and function in normotensive and hypertensive rats. J Vasc Res. 2003; 40:320–328.
Article25. Mulder P, Barbier S, Chagraoui A, Richard V, Henry JP, Lallemand F, et al. Long-term heart rate reduction induced by the selective I(f) current inhibitor ivabradine improves left ventricular function and intrinsic myocardial structure in congestive heart failure. Circulation. 2004; 109:1674–1679.
Article26. Tsutsui H, Momomura S, Yamashina A, Ogawa H, Shimokawa H, Kihara Y, et al. study investigators. Heart rate control with if inhibitor, ivabradine, in Japanese patients with chronic heart failure: a randomized, double-blind, placebo-controlled phase II study. Circ J. 2016; 80:668–676.
Article27. Fox K, Ford I, Steg PG, Tendera M, Ferrari R. BEAUTIFUL Investigators. Ivabradine for patients with stable coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a randomised, double-blind, placebo-controlled trial. Lancet. 2008; 372:807–816.
Article28. Swedberg K, Komajda M, Böhm M, Borer JS, Ford I, Dubost-Brama A, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010; 376:875–885.
Article29. Tardif JC, Ponikowski P, Kahan T. ASSOCIATE Study Investigators. Efficacy of the I(f) current inhibitor ivabradine in patients with chronic stable angina receiving beta-blocker therapy: a 4-month, randomized, placebo-controlled trial. Eur Heart J. 2009; 30:540–548.
Article30. Colin P, Ghaleh B, Monnet X, Su J, Hittinger L, Giudicelli JF, et al. Contributions of heart rate and contractility to myocardial oxygen balance during exercise. Am J Physiol Heart Circ Physiol. 2003; 284:H676–H682.31. Simon L, Ghaleh B, Puybasset L, Giudicelli JF, Berdeaux A. Coronary and hemodynamic effects of S 16257, a new bradycardic agent, in resting and exercising conscious dogs. J Pharmacol Exp Ther. 1995; 275:659–666.32. Monnet X, Ghaleh B, Colin P, de Curzon OP, Giudicelli JF, Berdeaux A. Effects of heart rate reduction with ivabradine on exercise-induced myocardial ischemia and stunning. J Pharmacol Exp Ther. 2001; 299:1133–1139.33. Monnet X, Colin P, Ghaleh B, Hittinger L, Giudicelli JF, Berdeaux A. Heart rate reduction during exercise-induced myocardial ischaemia and stunning. Eur Heart J. 2004; 25:579–586.
Article34. Lucats L, Ghaleh B, Monnet X, Colin P, Bizé A, Berdeaux A. Conversion of post-systolic wall thickening into ejectional thickening by selective heart rate reduction during myocardial stunning. Eur Heart J. 2007; 28:872–879.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peiminine inhibits myocardial injury and fibrosis after myocardial infarction in rats by regulating mitogen-activated protein kinase pathway
- Comparisons of Myocardial Protective Effects of Sevoflurane at Different Concentrations against Ischemia in Isolated Rat Heart
- The Effect of Sufentanil on Myocardial Function and Coronary Flow in an Isolated-Heart Rat Model
- Effects of Pretreated-Fentanyl on the Myocardial Function in Isolated Stunned Rat Heart
- Effects of Halothane, Fentanyl, and Propofol-Fentanyl Anesthesia on Functional Recovery of Stunned Myocardium in Dogs