Ann Dermatol.
2018 Oct;30(5):592-596. 10.5021/ad.2018.30.5.592.
Pretibial Myxedema Presenting as Severe Elephantiasis
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Kyung Hee University, Seoul, Korea.
- 2Department of Dermatology, College of Medicine, Kyung Hee University, Seoul, Korea. bellotte@hanmail.net
- KMID: 2419751
- DOI: http://doi.org/10.5021/ad.2018.30.5.592
Abstract
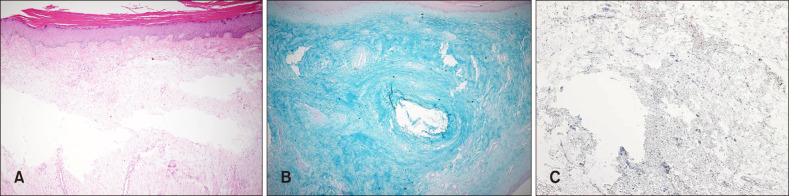
- Elephantiasis is a symptom characterized by the thickening of the skin and underlying tissues in the legs. Pretibial myxedema (PTM) is a non-frequent manifestation of autoimmune thyroiditis, particularly Graves' disease. Lesions of myxedema occur most commonly on the pretibial surfaces, also develop at sites of previous injury or scars and other areas. A 49-year-old male presented with severe elephantiasis on the both pretibial areas, dorsum of the feet, ankles and toes. Twenty years previously, he had received radioactive iodine treatment for thyrotoxicosis. Laboratory tests showed that the patient's thyroid function was normal, but the level of thyroid stimulating hormone (TSH) receptor antibodies was very high (>40 IU/L). The biopsy confirmed PTM. Interestingly, the connective tissue was stained with the TSH receptor antibodies in the deep dermis. Elephantiasic PTM is a severe form of the myxedema and there is few reported case. We report a rare case of PTM with appearance of severe elephantiasis.
Keyword
MeSH Terms
Figure
Reference
-
1. Yimer M, Hailu T, Mulu W, Abera B. Epidemiology of elephantiasis with special emphasis on podoconiosis in Ethiopia: a literature review. J Vector Borne Dis. 2015; 52:111–115. PMID: 26119541.2. Davies TF. Trauma and pressure explain the clinical presentation of the Graves' disease triad. Thyroid. 2000; 10:629–630. PMID: 11014305.
Article3. Fatourechi V. Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol. 2005; 6:295–309. PMID: 16252929.4. Schwartz KM, Fatourechi V, Ahmed DD. Dermopathy of graves' disease (pretibial myxedema): long-term outcome. J Clin Endocrinol Metab. 2002; 87:438–446. PMID: 11836263.
Article5. Rapoport B, Alsabeh R, Aftergood D, McLachlan SM. Elephantiasic pretibial myxedema: insight into and a hypothesis regarding the pathogenesis of the extrathyroidal manifestations of Graves' disease. Thyroid. 2000; 10:685–692. PMID: 11014313.
Article6. Pritchard J, Han R, Horst N, Cruikshank WW, Smith TJ. Immunoglobulin activation of T cell chemoattractant expression in fibroblasts from patients with Graves' disease is mediated through the insulin-like growth factor I receptor pathway. J Immunol. 2003; 170:6348–6354. PMID: 12794168.
Article7. di Meo N, Nan K, Noal C, Trevisini S, Fadel M, Damiani G, et al. Polypoid and fungating form of elephantiasic pretibial myxedema with involvement of the hands. Int J Dermatol. 2016; 55:e413–e415. PMID: 26873132.
Article8. Shirai K, Ito T, Mitsuhashi Y, Tsuboi R. Dramatic effect of low-dose oral steroid on elephantiasic pretibial myxedema. J Dermatol. 2014; 41:941–942. PMID: 25200964.
Article9. Yu H, Jiang X, Pan M, Huang R. Elephantiasic pretibial myxedema in a patient with graves disease that resolved after 131I treatment. Clin Nucl Med. 2014; 39:758–759. PMID: 24830877.
Article10. Heyes C, Nolan R, Leahy M, Gebauer K. Treatment-resistant elephantiasic thyroid dermopathy responding to rituximab and plasmapheresis. Australas J Dermatol. 2012; 53:e1–e4. PMID: 22309343.
Article11. Dhaille F, Dadban A, Meziane L, Fessier C, Colta L, Lok C, et al. Elephantiasic pretibial myxoedema with upper-limb involvement, treated with low-dose intravenous immunoglobulins. Clin Exp Dermatol. 2012; 37:307–308. PMID: 22007759.
Article12. Terheyden P, Kahaly GJ, Zillikens D, Bröcker EB. Lack of response of elephantiasic pretibia myxoedema to treatment with high-dose intravenous immunoglobulin. Clin Exp Dermatol. 2003; 28:224–226. PMID: 12653721.13. Susser WS, Heermans AG, Chapman MS, Baughman RD. Elephantiasic pretibial myxedema: a novel treatment for an uncommon disorder. J Am Acad Dermatol. 2002; 46:723–726. PMID: 12004314.
Article14. Lan C, Li C, Yang M, Mei X, He Z, Chen W, et al. Pretibial myxoedema with autoimmunity and hyperplasia treated with glucocorticoids and surgery. Br J Dermatol. 2012; 166:457–459. PMID: 21848686.
Article15. Felton J, Derrick EK, Price ML. Successful combined surgical and octreotide treatment of severe pretibial myxedema reviewed after 9 years. Br J Dermatol. 2003; 148:825–826. PMID: 12752151.