Clin Endosc.
2018 Jul;51(4):368-374. 10.5946/ce.2017.155.
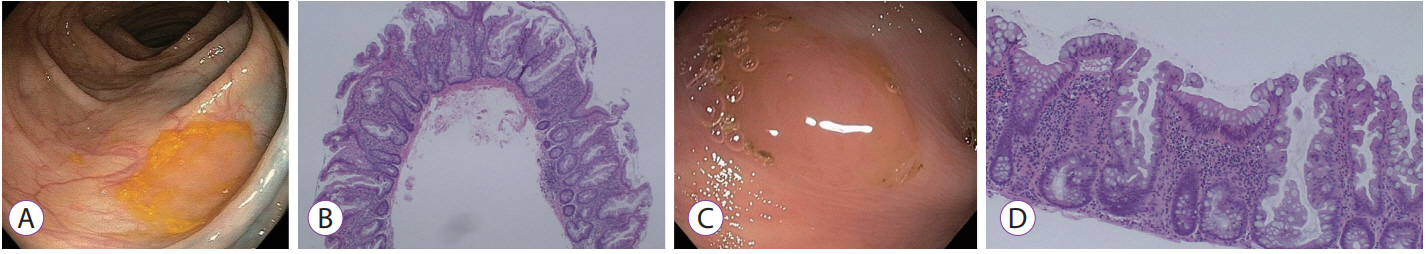
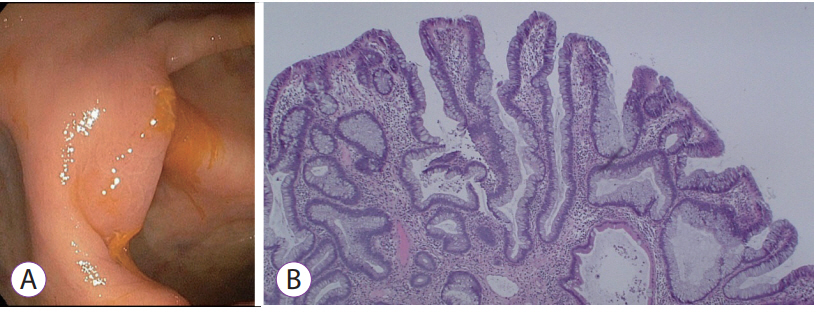
Endoscopic Features of Mucous Cap Polyps: A Way to Predict Serrated Polyps
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, UConn Health, Farmington, CT, USA. moy@uchc.edu
- 2Department of Pathology, UConn Health, Farmington, CT, USA.
- 3Connecticut Institute for Clinical & Translational Science, UConn Health, Farmington, CT, USA.
- KMID: 2419709
- DOI: http://doi.org/10.5946/ce.2017.155
Abstract
- BACKGROUND/AIMS
The aims of the study were to identify whether a mucous-cap predicts the presence of serrated polyps, and to determine whether additional endoscopic findings predict the presence of a sessile serrated adenomas/polyp (SSA/P).
METHODS
We analyzed 147 mucous-capped polyps with corresponding histology, during 2011-2014. Eight endoscopic features (presence of borders, elevation, rim of debris, location in the colon, size ≥10 mm, varicose vessels, nodularity, and alteration in mucosal folds) of mucous-capped polyps were examined to see if they can predict SSA/Ps.
RESULTS
A total of 86% (n=126) of mucous-capped polyps were from the right sided serrated pathway (right-sided hyperplastic [n=83], SSA/Ps [n=43], traditional serrated adenoma [n=1]), 10% (n=15) were left-sided hyperplastic polyps, and 3% (n=5) were from the adenoma-carcinoma sequence. The presence of a mucous cap combined with varicose vessels was the only significant predictor for SSA/Ps. The other seven characteristics were not found to be statistically significant for SSA/Ps, although location in the colon and the presence of nodularity trended towards significance.
CONCLUSIONS
Our study suggests that mucous-capped polyps have high predictability for being a part of the serrated pathway. Gastroenterologists should be alert for a mucous-capped polyp with varicose veins, as these lesions have a higher risk of SSA/P.
Figure
Cited by 1 articles
-
How to Detect Sessile Serrated Adenoma/Polyps
Eun Ran Kim, Dong Kyung Chang
Clin Endosc. 2018;51(4):313-314. doi: 10.5946/ce.2018.108.
Reference
-
1. Vogelstein B, Fearon ER, Hamilton SR, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988; 319:525–532.
Article2. Sillars-Hardebol AH, Carvalho B, van Engeland M, Fijneman RJ, Meijer GA. The adenoma hunt in colorectal cancer screening: defining the target. J Pathol. 2012; 226:1–6.
Article3. East JE, Saunders BP, Jass JR. Sporadic and syndromic hyperplastic polyps and serrated adenomas of the colon: classification, molecular genetics, natural history, and clinical management. Gastroenterol Clin North Am. 2008; 37:25–46, v.
Article4. Arnold CA, Montgomery E, Iacobuzio-Donahue CA. The serrated pathway of neoplasia: new insights into an evolving concept. Diagn Histopathol (Oxf). 2011; 17:367–375.
Article5. Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010; 138:2088–2100.
Article6. Torlakovic E, Skovlund E, Snover DC, Torlakovic G, Nesland JM. Morphologic reappraisal of serrated colorectal polyps. Am J Surg Pathol. 2003; 27:65–81.
Article7. Tadepalli US, Feihel D, Miller KM, et al. A morphologic analysis of sessile serrated polyps observed during routine colonoscopy (with video). Gastrointest Endosc. 2011; 74:1360–1368.
Article8. Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabeneck L. Rates of new or missed colorectal cancers after colonoscopy and their risk factors: a population-based analysis. Gastroenterology. 2007; 132:96–102.
Article9. Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009; 150:1–8.
Article10. Hetzel JT, Huang CS, Coukos JA, et al. Variation in the detection of serrated polyps in an average risk colorectal cancer screening cohort. Am J Gastroenterol. 2010; 105:2656–2664.
Article11. de Wijkerslooth TR, Stoop EM, Bossuyt PM, et al. Differences in proximal serrated polyp detection among endoscopists are associated with variability in withdrawal time. Gastrointest Endosc. 2013; 77:617–623.
Article12. Kahi CJ, Hewett DG, Norton DL, Eckert GJ, Rex DK. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy. Clin Gastroenterol Hepatol. 2011; 9:42–46.
Article13. Pohl H, Srivastava A, Bensen SP, et al. Incomplete polyp resection during colonoscopy-results of the complete adenoma resection (CARE) study. Gastroenterology. 2013; 144:74–80.e1.
Article14. Murakami T, Sakamoto N, Ritsuno H, et al. Distinct endoscopic characteristics of sessile serrated adenoma/polyp with and without dysplasia/carcinoma. Gastrointest Endosc. 2017; 85:590–600.
Article15. Parente F, Marino B, Crosta C. Bowel preparation before colonoscopy in the era of mass screening for colo-rectal cancer: a practical approach. Dig Liver Dis. 2009; 41:87–95.
Article16. Chiu HM, Lin JT, Lee YC, et al. Different bowel preparation schedule leads to different diagnostic yield of proximal and nonpolypoid colorectal neoplasm at screening colonoscopy in average-risk population. Dis Colon Rectum. 2011; 54:1570–1577.
Article17. Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003; 58:76–79.
Article18. Pereyra L, Gómez EJ, González R, et al. Finding sessile serrated adenomas: is it possible to identify them during conventional colonoscopy? Dig Dis Sci. 2014; 59:3021–3026.
Article19. Rustagi T, Rangasamy P, Myers M, et al. Sessile serrated adenomas in the proximal colon are likely to be flat, large and occur in smokers. World J Gastroenterol. 2013; 19:5271–5277.
Article20. Bauer VP, Papaconstantinou HT. Management of serrated adenomas and hyperplastic polyps. Clin Colon Rectal Surg. 2008; 21:273–279.
Article21. Zhu H, Zhang G, Yi X, et al. Histology subtypes and polyp size are associated with synchronous colorectal carcinoma of colorectal serrated polyps: a study of 499 serrated polyps. Am J Cancer Res. 2015; 5:363–374.22. Rex DK, Ahnen DJ, Baron JA, et al. Serrated lesions of the colorectum: review and recommendations from an expert panel. Am J Gastroenterol. 2012; 107:1315–1329. quiz 1314, 1330.
Article23. Saito S, Tajiri H, Ikegami M. Serrated polyps of the colon and rectum: endoscopic features including image enhanced endoscopy. World J Gastrointest Endosc. 2015; 7:860–871.
Article24. Mäkinen MJ. Colorectal serrated adenocarcinoma. Histopathology. 2007; 50:131–150.
Article25. Carr NJ, Mahajan H, Tan KL, Hawkins NJ, Ward RL. Serrated and non-serrated polyps of the colorectum: their prevalence in an unselected case series and correlation of BRAF mutation analysis with the diagnosis of sessile serrated adenoma. J Clin Pathol. 2009; 62:516–518.
Article26. Kim KM, Lee EJ, Ha S, et al. Molecular features of colorectal hyperplastic polyps and sessile serrated adenoma/polyps from Korea. Am J Surg Pathol. 2011; 35:1274–1286.
Article27. Spring KJ, Zhao ZZ, Karamatic R, et al. High prevalence of sessile serrated adenomas with BRAF mutations: a prospective study of patients undergoing colonoscopy. Gastroenterology. 2006; 131:1400–1407.
Article28. Gurudu SR, Heigh RI, De Petris G, et al. Sessile serrated adenomas: demographic, endoscopic and pathological characteristics. World J Gastroenterol. 2010; 16:3402–3405.
Article29. Hazewinkel Y, López-Cerón M, East JE, et al. Endoscopic features of sessile serrated adenomas: validation by international experts using high-resolution white-light endoscopy and narrow-band imaging. Gastrointest Endosc. 2013; 77:916–924.
Article30. Nakao Y, Saito S, Ohya T, et al. Endoscopic features of colorectal serrated lesions using image-enhanced endoscopy with pathological analysis. Eur J Gastroenterol Hepatol. 2013; 25:981–988.
Article31. Uraoka T, Higashi R, Horii J, et al. Prospective evaluation of endoscopic criteria characteristic of sessile serrated adenomas/polyps. J Gastroenterol. 2015; 50:555–563.
Article32. East JE, Suzuki N, Bassett P, et al. Narrow band imaging with magnification for the characterization of small and diminutive colonic polyps: pit pattern and vascular pattern intensity. Endoscopy. 2008; 40:811–817.
Article33. Yamashina T, Takeuchi Y, Uedo N, et al. Diagnostic features of sessile serrated adenoma/polyps on magnifying narrow band imaging: a prospective study of diagnostic accuracy. J Gastroenterol Hepatol. 2015; 30:117–123.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Diagnosis, Treatment, and Follow-up of Serrated Polyps
- Sessile Serrated Adenoma with High-grade Dysplasia
- External Validation of the Endoscopic Features of Sessile Serrated Adenomas in Expert and Trainee Colonoscopists
- Serrated Adenoma with Adenocarcinoma of Stomach Treated by Endoscopic Submucosal Dissection
- Optical diagnosis by near-focus versus normal-focus narrow band imaging colonoscopy in colorectal polyps based on combined NICE and WASP classification: a randomized controlled trial