Clin Endosc.
2018 Jul;51(4):362-367. 10.5946/ce.2017.177.
Accuracy of Endoscopic Diagnosis for Mild Atrophic Gastritis Infected with Helicobacter pylori
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Medicine, Shinshu University School of Medicine, Japan. tokamura@shinshu-u.ac.jp
- 2Endoscopic Examination Center, Shinshu University Hospital, Matsumoto, Japan.
- KMID: 2419708
- DOI: http://doi.org/10.5946/ce.2017.177
Abstract
- BACKGROUND/AIMS
This study examined the accuracy of endoscopic evaluation for determining the Helicobacter pylori infection status in patients with mild atrophy who might not exhibit characteristic endoscopic findings.
METHODS
Forty endoscopists determined the H. pylori infection status of 50 randomly presented H. pylori-positive and H. pylori-negative cases on the basis of a list of established findings.
RESULTS
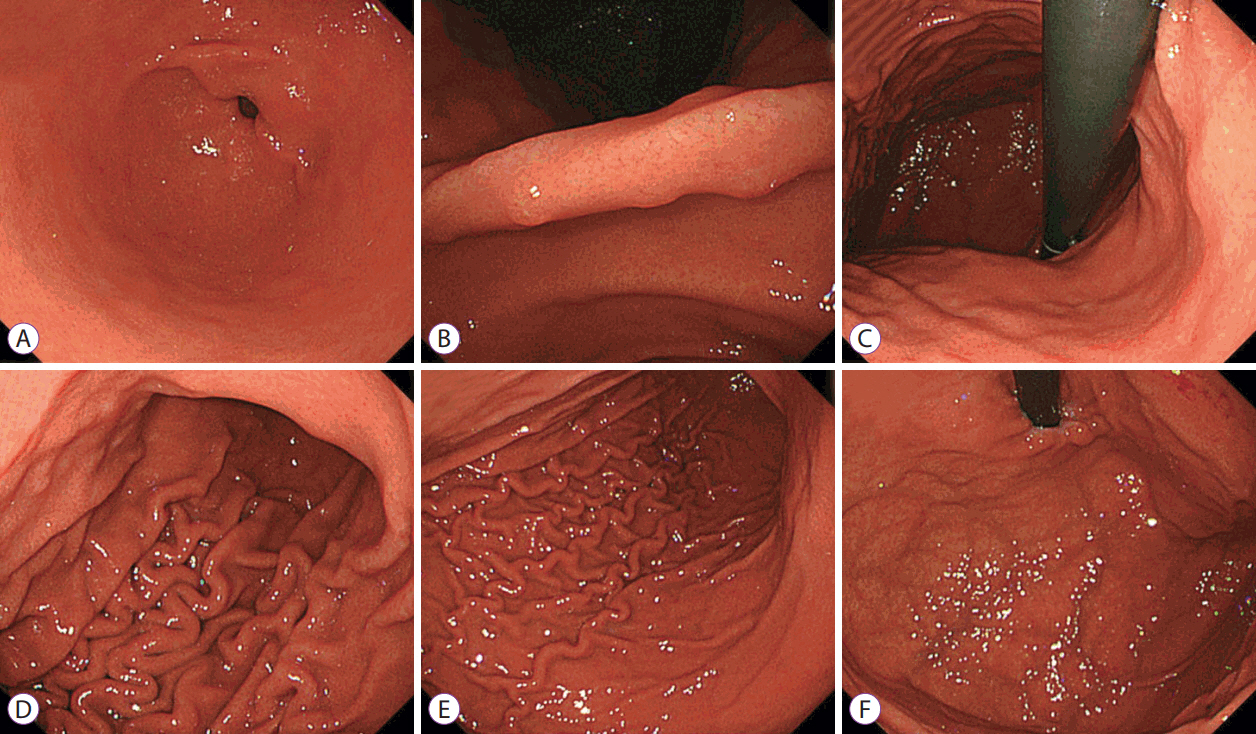
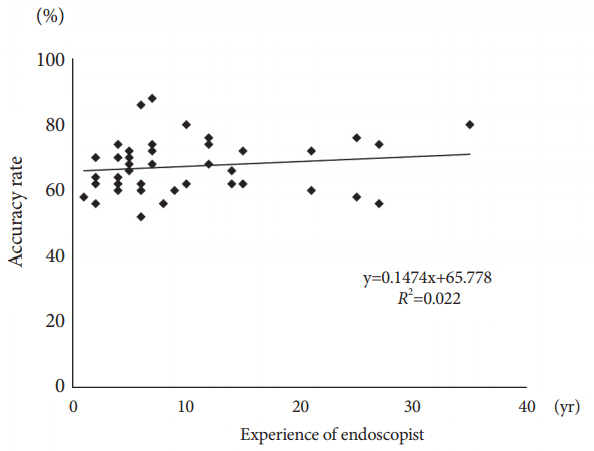
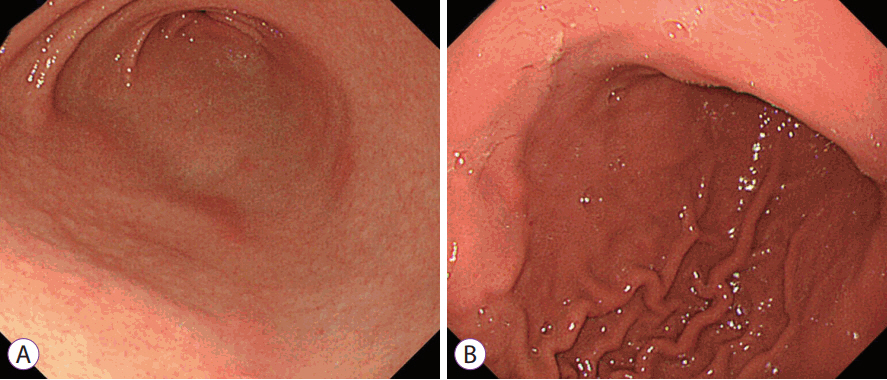
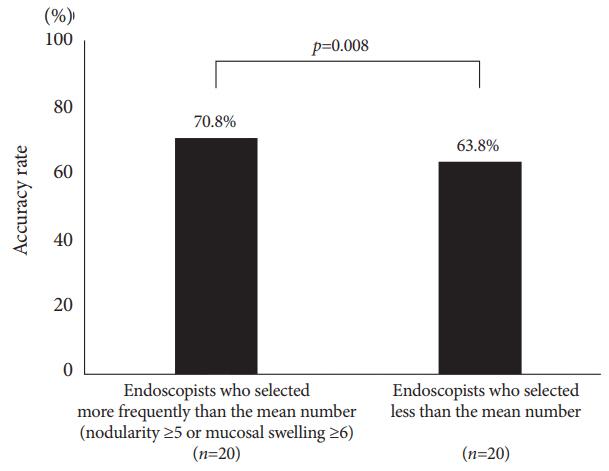
The median clinical endoscopy experience was 7 years (range, 1-35 years), including 22 board-certified endoscopists (55%) of the Japan Gastroenterological Endoscopy Society. The mean accuracy rate of endoscopic diagnosis was 67% and was unrelated to experience status (experienced vs. trainee: 69% vs. 65%, p=0.089) and total years of experience (R 2 =0.022). The most frequently selected endoscopic findings were regular arrangement of collecting venules (59%), atrophy (45%), and red streak (22%), which had fair accuracy rates of 67%, 65%, and 73%, respectively. By contrast, the accuracy rates of nodularity (89%) and mucosal swelling (77%) were highest. The 20 endoscopists who more frequently identified these findings diagnosed H. pylori infection significantly more accurately than did the other endoscopists (71% vs. 64%, p=0.008).
CONCLUSIONS
Careful attention to nodularity and mucosal swelling in patients with mild atrophy may enhance diagnosis, enable prompt treatment, and avoid possible long-term carcinogenesis.
MeSH Terms
Figure
Cited by 1 articles
-
Accuracy of Endoscopic Diagnosis of Mild Atrophic Gastritis with
Helicobacter pylori Infection
Dae Bum Kim, Woo Chul Chung
Clin Endosc. 2018;51(4):310-312. doi: 10.5946/ce.2018.085.
Reference
-
1. Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001; 345:784–789.2. Fukase K, Kato M, Kikuchi S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet. 2008; 372:392–397.
Article3. Asaka M. A new approach for elimination of gastric cancer deaths in Japan. Int J Cancer. 2013; 132:1272–1276.
Article4. Masuyama H, Yoshitake N, Sasai T, et al. Relationship between the degree of endoscopic atrophy of the gastric mucosa and carcinogenic risk. Digestion. 2015; 91:30–36.
Article5. Wong BC, Lam SK, Wong WM, et al. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA. 2004; 291:187–194.6. Kato T, Yagi N, Kamada T, Shimbo T, Watanabe H, Ida K. Diagnosis of Helicobacter pylori infection in gastric mucosa by endoscopic features: a multicenter prospective study. Dig Endosc. 2013; 25:508–518.7. Watanabe K, Nagata N, Nakashima R, et al. Predictive findings for Helicobacter pylori-uninfected, -infected and -eradicated gastric mucosa: validation study. World J Gastroenterol. 2013; 19:4374–4379.8. Yagi K, Nakamura A, Sekine A. Characteristic endoscopic and magnified endoscopic findings in the normal stomach without Helicobacter pylori infection. J Gastroenterol Hepatol. 2002; 17:39–45.
Article9. Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969; 1:87–97.
Article10. Kamada T, Haruma K, Inoue K, Shiotani A. [Helicobacter pylori infection and endoscopic gastritis -Kyoto classification of gastritis]. Nihon Shokakibyo Gakkai Zasshi. 2015; 112:982–993.11. Shiotani A, Kamada T, Kumamoto M, et al. Nodular gastritis in Japanese young adults: endoscopic and histological observations. J Gastroenterol. 2007; 42:610–615.
Article12. Kato S, Nishino Y, Ozawa K, et al. The prevalence of Helicobacter pylori in Japanese children with gastritis or peptic ulcer disease. J Gastroenterol. 2004; 39:734–738.
Article13. Ricuarte O, Gutierrez O, Cardona H, Kim JG, Graham DY, El-Zimaity HM. Atrophic gastritis in young children and adolescents. J Clin Pathol. 2005; 58:1189–1193.
Article14. Okamura T, Sakai Y, Hoshino H, Iwaya Y, Tanaka E, Kobayashi M. Superficially located enlarged lymphoid follicles characterise nodular gastritis. Pathology. 2015; 47:38–44.
Article15. Kitamura S, Yasuda M, Muguruma N, et al. Prevalence and characteristics of nodular gastritis in Japanese elderly. J Gastroenterol Hepatol. 2013; 28:1154–1160.
Article16. Nomura S, Terao S, Adachi K, et al. Endoscopic diagnosis of gastric mucosal activity and inflammation. Dig Endosc. 2013; 25:136–146.
Article17. Ohkuma K, Okada M, Murayama H, et al. Association of Helicobacter pylori infection with atrophic gastritis and intestinal metaplasia. J Gastroenterol Hepatol. 2000; 15:1105–1112.
Article18. Yagi K, Aruga Y, Nakamura A, Sekine A. Regular arrangement of collecting venules (RAC): a characteristic endoscopic feature of Helicobacter pylori-negative normal stomach and its relationship with esophago-gastric adenocarcinoma. J Gastroenterol. 2005; 40:443–452.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of Endoscopic Diagnosis of Mild Atrophic Gastritis with Helicobacter pylori Infection
- Changing Trends of Serum Pepsinogen I/II Ratio in Asymptomatic Subjects
- Endoscopic gastritis, serum pepsinogen assay, and Helicobacter pylori infection
- Successful Eradication of Helicobacter pylori Using Modified Quadruple Therapy in Patient with Long-lasting H. pylori-induced Active Gastritis
- Atrophic Gastritis: Pathophysiology and Etiology