Yonsei Med J.
2017 Sep;58(5):1066-1070. 10.3349/ymj.2017.58.5.1066.
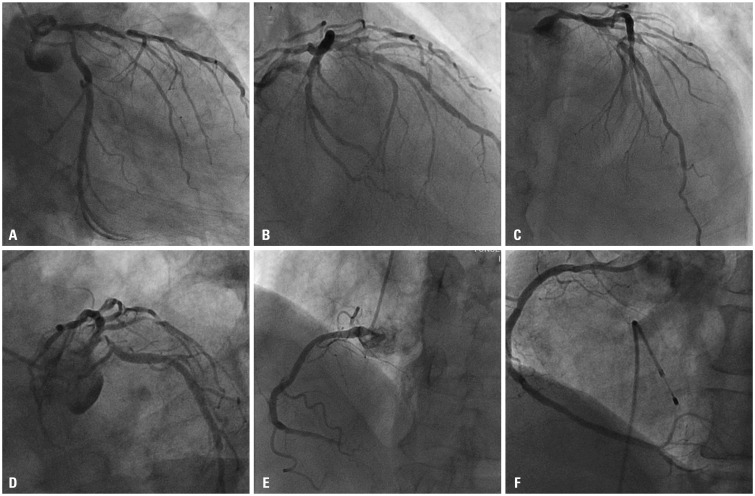
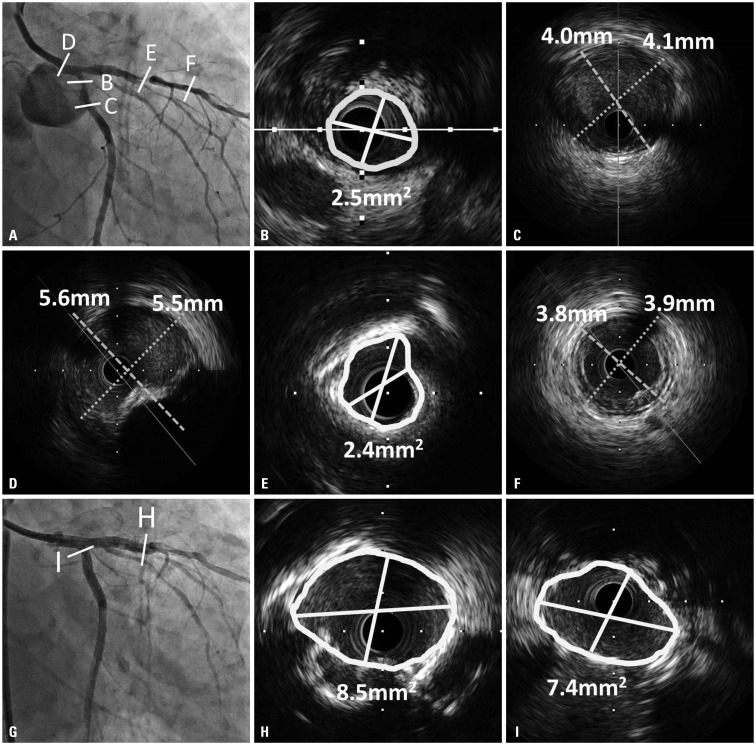
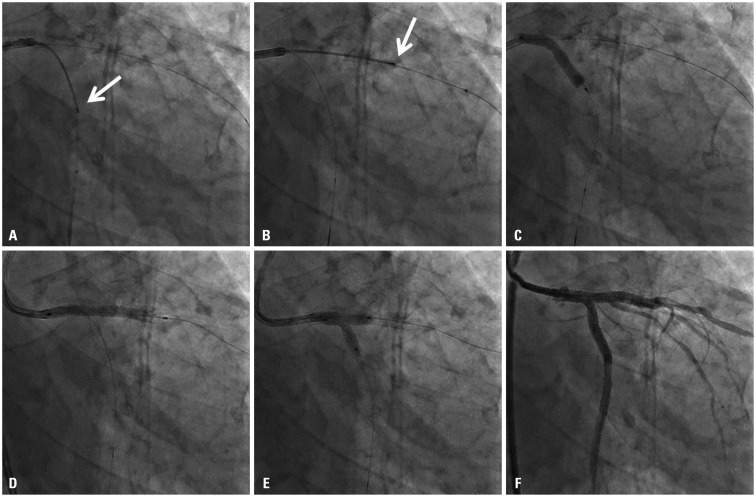
Successful Treatment of Unprotected Left Main Coronary Bifurcation Lesion Using Minimum Contrast Volume with Intravascular Ultrasound Guidance
- Affiliations
-
- 1Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University Health System, Seoul, Korea. mkhong61@yuhs.ac
- 2Cardiovascular Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- 3Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2418948
- DOI: http://doi.org/10.3349/ymj.2017.58.5.1066
Abstract
- Contrast-induced nephropathy (CIN) is a serious complication in patients undergoing percutaneous coronary intervention (PCI), and is associated with higher morbidity and mortality. The limiting volume of contrast medium is safest and most reliable strategy for CIN prevention. Intravascular ultrasound (IVUS) serves as an attractive alternative imaging tool to angiography in many steps during PCI, thereby reducing the use of contrast agents. Here, we reported a case of successfully treated unprotected left main bifurcation lesion with heavily calcified and diffuse lesion under the IVUS-guided PCI using low volumes of contrast dye of total 12 cc in an elderly patient.
MeSH Terms
Figure
Reference
-
1. Mehran R, Nikolsky E. Contrast-induced nephropathy: definition, epidemiology, and patients at risk. Kidney Int Suppl. 2006; (100):S11–S15. PMID: 16612394.
Article2. Lin YS, Fang HY, Hussein H, Fang CY, Chen YL, Hsueh SK, et al. Predictors of contrast-induced nephropathy in chronic total occlusion percutaneous coronary intervention. EuroIntervention. 2014; 9:1173–1180. PMID: 24561734.3. Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002; 105:2259–2264. PMID: 12010907.4. Azzalini L, Spagnoli V, Ly HQ. Contrast-induced nephropathy: from pathophysiology to preventive strategies. Can J Cardiol. 2016; 32:247–255. PMID: 26277092.
Article5. Nayak KR, Mehta HS, Price MJ, Russo RJ, Stinis CT, Moses JW, et al. A novel technique for ultra-low contrast administration during angiography or intervention. Catheter Cardiovasc Interv. 2010; 75:1076–1083. PMID: 20146209.
Article6. Ali ZA, Karimi Galougahi K, Nazif T, Maehara A, Hardy MA, Cohen DJ, et al. Imaging- and physiology-guided percutaneous coronary intervention without contrast administration in advanced renal failure: a feasibility, safety, and outcome study. Eur Heart J. 2016; 37:3090–3095. PMID: 26957421.
Article7. Mariani J Jr, Guedes C, Soares P, Zalc S, Campos CM, Lopes AC, et al. Intravascular ultrasound guidance to minimize the use of iodine contrast in percutaneous coronary intervention: the MOZART (minimizing contrast utilization with IVUS guidance in coronary angioplasty) randomized controlled trial. JACC Cardiovasc Interv. 2014; 7:1287–1293. PMID: 25326742.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Treatment of an Injured Coronary Stent Using the Looping Wire Technique
- Successful Drug-Eluting Stent Overexpansion with Intravascular Ultrasound Guidance for Left Main Bifurcation Lesion Via Left Snuffbox Approach
- Stenting of Unprotected Left Main Coronary Artery Stenosis without Anticogulation: Immediate and Late Outcomes
- A Case of Coronary Pseudostenosis, Diagnosed by Intravascular Ultrasound
- Past, Present, and Future of Left Main Coronary Artery PCI