Healthc Inform Res.
2018 Apr;24(2):125-138. 10.4258/hir.2018.24.2.125.
Development of the IMB Model and an Evidence-Based Diabetes Self-management Mobile Application
- Affiliations
-
- 1College of Nursing, Seoul National University, Seoul, Korea. hapark@snu.ac.kr
- 2Systems Biomedical Informatics Research Center, Seoul National University, Seoul, Korea.
- KMID: 2418181
- DOI: http://doi.org/10.4258/hir.2018.24.2.125
Abstract
OBJECTIVES
This study developed a diabetes self-management mobile application based on the information-motivation-behavioral skills (IMB) model, evidence extracted from clinical practice guidelines, and requirements identified through focus group interviews (FGIs) with diabetes patients.
METHODS
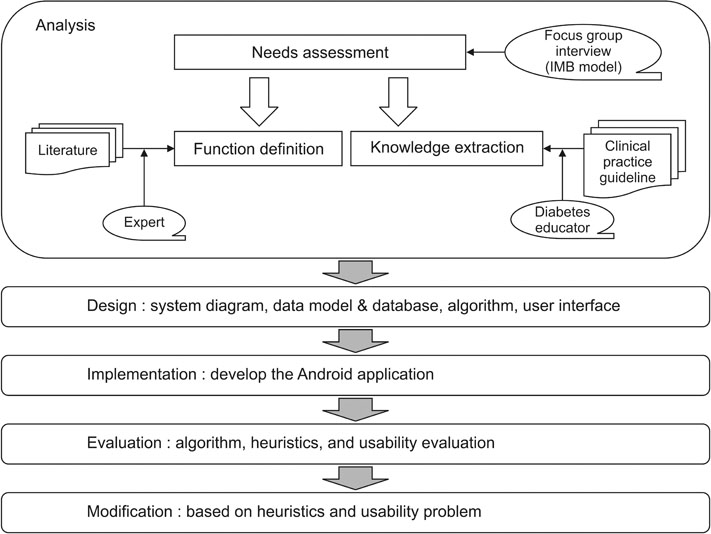
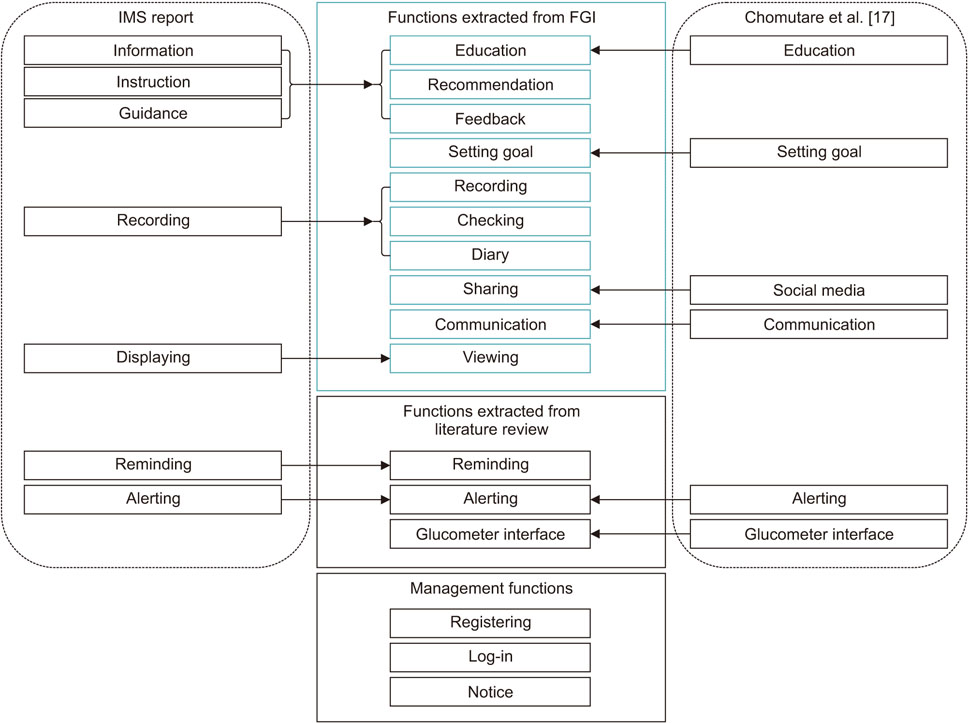
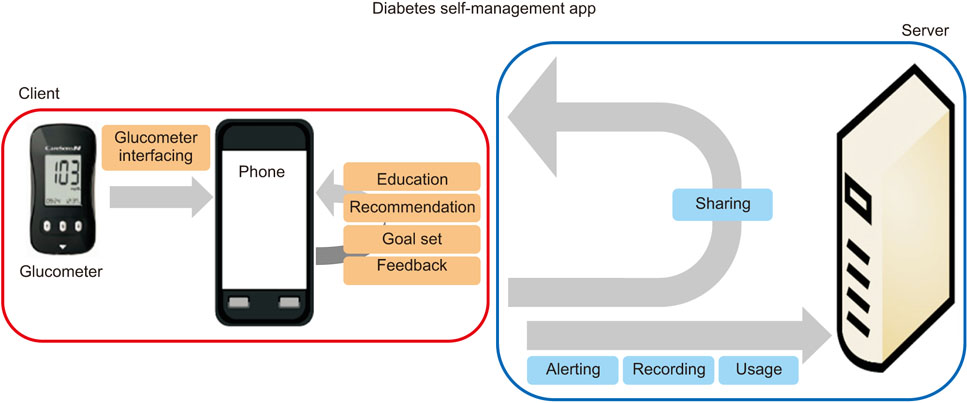
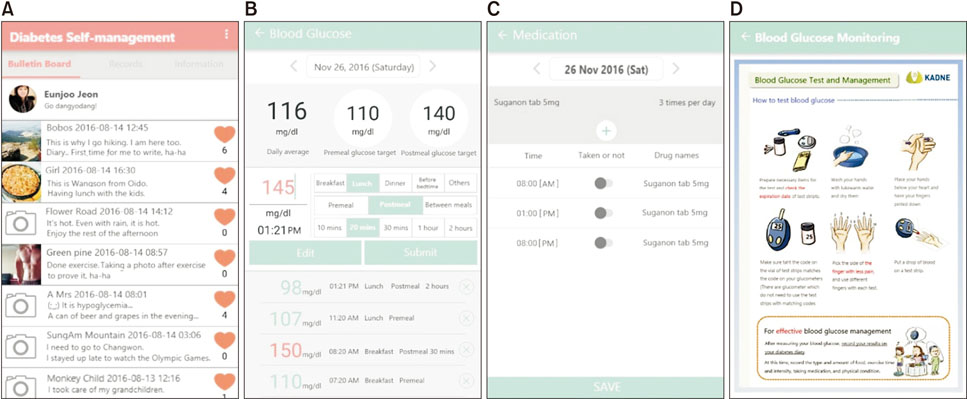
We developed a diabetes self-management (DSM) app in accordance with the following four stages of the system development life cycle. The functional and knowledge requirements of the users were extracted through FGIs with 19 diabetes patients. A system diagram, data models, a database, an algorithm, screens, and menus were designed. An Android app and server with an SSL protocol were developed. The DSM app algorithm and heuristics, as well as the usability of the DSM app were evaluated, and then the DSM app was modified based on heuristics and usability evaluation.
RESULTS
A total of 11 requirement themes were identified through the FGIs. Sixteen functions and 49 knowledge rules were extracted. The system diagram consisted of a client part and server part, 78 data models, a database with 10 tables, an algorithm, and a menu structure with 6 main menus, and 40 user screens were developed. The DSM app was Android version 4.4 or higher for Bluetooth connectivity. The proficiency and efficiency scores of the algorithm were 90.96% and 92.39%, respectively. Fifteen issues were revealed through the heuristic evaluation, and the app was modified to address three of these issues. It was also modified to address five comments received by the researchers through the usability evaluation.
CONCLUSIONS
The DSM app was developed based on behavioral change theory through IMB models. It was designed to be evidence-based, user-centered, and effective. It remains necessary to fully evaluate the effect of the DSM app on the DSM behavior changes of diabetes patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Torgan CE. The mHealth summit: local & global converge [Internet]. [place unknown]: caroltorgan.com;2009. cited 2018 Apr 1. Available from: http://caroltorgan.com/mhealth-summit/.2. Thirumurthy H, Lester RT. M-health for health behaviour change in resource-limited settings: applications to HIV care and beyond. Bull World Health Organ. 2012; 90(5):390–392.
Article3. Blake H. Mobile phone technology in chronic disease management. Nurs Stand. 2008; 23(12):43–46.
Article4. American Association of Diabetes Educators. AADE guidelines for the practice of diabetes self-management education and training (DSME/T). Diabetes Educ. 2009; 35:3_suppl. 85S–107S.5. Aitken M. Patient adoption of mHealth: use, evidence and remaining barriers to mainstream acceptance. Parsippany (NJ): IMS Institute for Healthcare Informatics;2015.6. Liang X, Wang Q, Yang X, Cao J, Chen J, Mo X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med. 2011; 28(4):455–463.
Article7. Hardeman W, Sutton S, Griffin S, Johnston M, White A, Wareham NJ, et al. A causal modelling approach to the development of theory-based behaviour change programmes for trial evaluation. Health Educ Res. 2005; 20(6):676–687.
Article8. Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med. 2011; 1(1):53–71.
Article9. Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006; 23(12):1332–1338.
Article10. Choi S, Song M. Behavior change theories in diabetes self-management: a conceptual review. Perspect Nurs Sci. 2010; 7(1):1–9.11. Fisher WA, Fisher JD, Harman J. The information-motivation-behavioral skills model: A general social psychological approach to understanding and promoting health behavior. In : Suls J, Wallston KA, editors. Social psychological foundations of health and illness. Malden (MA): Blackwell Publishing;2003. p. 82–106.12. Mulcahy K, Maryniuk M, Peeples M, Peyrot M, Tomky D, Weaver T, et al. Diabetes self-management education core outcomes measures. Diabetes Educ. 2003; 29(5):768–770. 773–784. 787–788. passim.
Article13. Osborn CY, Egede LE. Validation of an Information-Motivation-Behavioral Skills model of diabetes self-care (IMB-DSC). Patient Educ Couns. 2010; 79(1):49–54.
Article14. Gao J, Wang J, Zhu Y, Yu J. Validation of an information-motivation-behavioral skills model of self-care among Chinese adults with type 2 diabetes. BMC Public Health. 2013; 13:100.
Article15. Choi S, Song M, Chang SJ, Kim SA. Strategies for enhancing information, motivation, and skills for self-management behavior changes: a qualitative study of diabetes care for older adults in Korea. Patient Prefer Adherence. 2014; 8:219–226.
Article16. Wensing M, Huntink E, van Lieshout J, Godycki-Cwirko M, Kowalczyk A, Jager C, et al. Tailored implementation of evidence-based practice for patients with chronic diseases. PLoS One. 2014; 9(7):e101981.
Article17. Chomutare T, Fernandez-Luque L, Arsand E, Hartvigsen G. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res. 2011; 13(3):e65.
Article18. Chae YH, Son SG. Effects of individual nursing education on self-efficacy and sick-roll behavior in diabetes patients. J Korean Acad Soc Nurs Educ. 2000; 6(1):103–114.19. LeRouge C, Wickramasinghe N. A review of user-centered design for diabetes-related consumer health informatics technologies. J Diabetes Sci Technol. 2013; 7(4):1039–1056.
Article20. Mayring P. Qualitative content analysis: theoretical foundation, basic procedures and software solution. Klagenfurt, Austria: Philipp Mayring;2014.21. Choubey MK. IT infrastructure and management: for the GBTU and MMTU. Uttar Pradesh, India: Pearson Education India;2011.
Article22. Choi J, Bakken S. Creation of a gold standard for validation of a computer-interpretable depression screening guideline. Stud Health Technol Inform. 2006; 122:95–99.23. Bertini E, Gabrielli S, Kimani S. Appropriating and assessing heuristics for mobile computing. In : Proceedings of the Working Conference on Advanced Visual Interfaces; 2006 May 23–26; Venezia, Italy. p. 119–126.24. American Diabetes Association. Standards of medical care in diabetes: 2014. Diabetes Care. 2014; 37:Suppl 1. S14–S80.25. Korean Diabetes Association. Clinical practice guideline for diabetes management. Seoul, Korea: Committee of Clinical Practice Guideline of KDA;2013.26. Korea Association of Diabetes Nurse Educator. Smart diabetes management: standard management guidelines to win diabetes. Seoul, Korea: Simong;2012.27. Seoul National University Hospital. Bundang Seoul National University Hospital. Boramae Medical Center. Seoul National University Hospital Gangnam Center. Guidelines for managing diabetes: diabetes living guidelines for a healthy and abundant life. Seoul, Korea: Panmun Education;2012.28. Fitzgerald JT, Funnell MM, Hess GE, Barr PA, Anderson RM, Hiss RG, et al. The reliability and validity of a brief diabetes knowledge test. Diabetes Care. 1998; 21(5):706–710.
Article29. Peyrot M, Peeples M, Tomky D, Charron-Prochownik D, Weaver T. AADE Outcomes Project and AADE/UPMC Diabetes Education Outcomes Project. UPMC Diabetes Education Outcomes Project. Development of the American Association of Diabetes Educators' diabetes self-management assessment report tool. Diabetes Educ. 2007; 33(5):818–826.
Article30. Ministry of Food and Drug Safety. Food nutrition ingredient DB [Internet]. Cheongju, Korea: Ministry of Food and Drug Safety;c2018. cited at 218 Apr 1. Available from:https://www.foodsafetykorea.go.kr/portal/healthyfoodlife/foodnutrient/simpleSearch.do?menu_grp=MENU_NEW03&menu_no=2805.31. Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, et al. National standards for diabetes self-management education and support. Diabetes Care. 2013; 36:Suppl 1. S100–S108.
Article32. Peyrot M, Rubin RR. Behavioral and psychosocial interventions in diabetes: a conceptual review. Diabetes Care. 2007; 30(10):2433–2440.
Article33. Snoek FJ, Pouwer F, Welch GW, Polonsky WH. Diabetes-related emotional distress in Dutch and US diabetic patients: cross-cultural validity of the problem areas in diabetes scale. Diabetes Care. 2000; 23(9):1305–1309.
Article34. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care. 2009; 32:Suppl 1. S87–S94.
Article35. Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT, Assendelft WJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care. 2001; 24(10):1821–1833.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coronavirus disease vaccine linked menstrual changes: mobile application study
- HealthTWITTER Initiative: Design of a Social Networking Service Based Tailored Application for Diabetes Self-Management
- Diabetes Management via a Mobile Application: a Case Report
- Diabetes Management according to Blood Glucose Measurement Trend
- Using a Mobile-based Nutritional Intervention Application Improves Glycemic Control but Reduces the Intake of Some Nutrients in Patients with Gestational Diabetes Mellitus: A Case Series Study