Ann Rehabil Med.
2018 Jun;42(3):416-424. 10.5535/arm.2018.42.3.416.
Changes in Hyolaryngeal Movement During Swallowing in the Lateral Decubitus Posture
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Physical Medicine and Rehabilitation, Kosin University College of Medicine, Busan, Korea. oggum@hanmail.net
- 3Department of Biomedical Engineering, Seoul National University College of Medicine, Seoul, Korea.
- 4Department of Rehabilitation Medicine, Gangwon-Do Rehabilitation Hospital, Chuncheon, Korea.
- KMID: 2417833
- DOI: http://doi.org/10.5535/arm.2018.42.3.416
Abstract
OBJECTIVE
To investigate the differences in hyolaryngeal kinematics at rest and during swallowing in the upright sitting (UP) and the lateral decubitus (LD) postures in healthy adults, and delineating any potential advantages of swallowing while in the LD posture.
METHODS
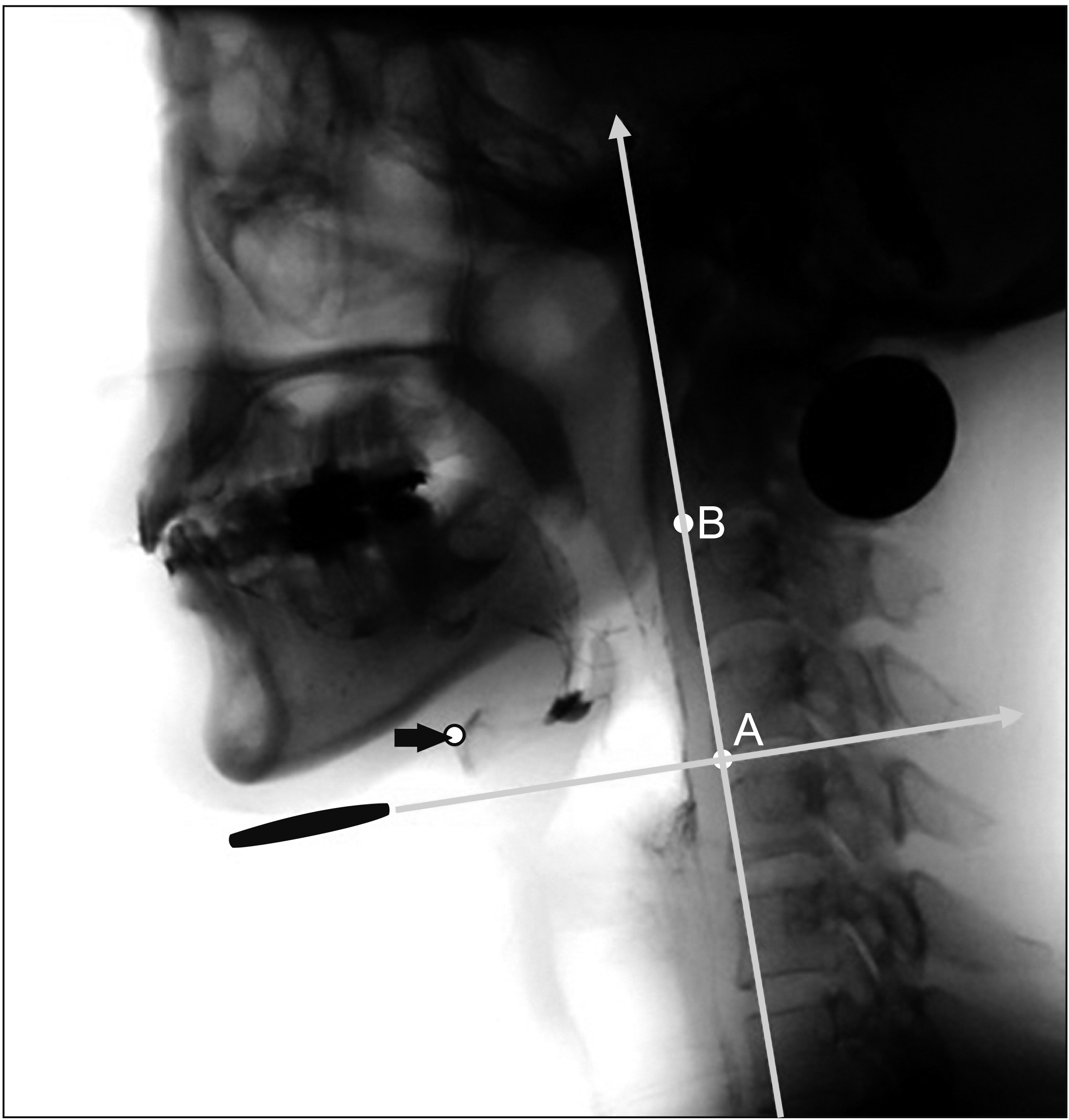
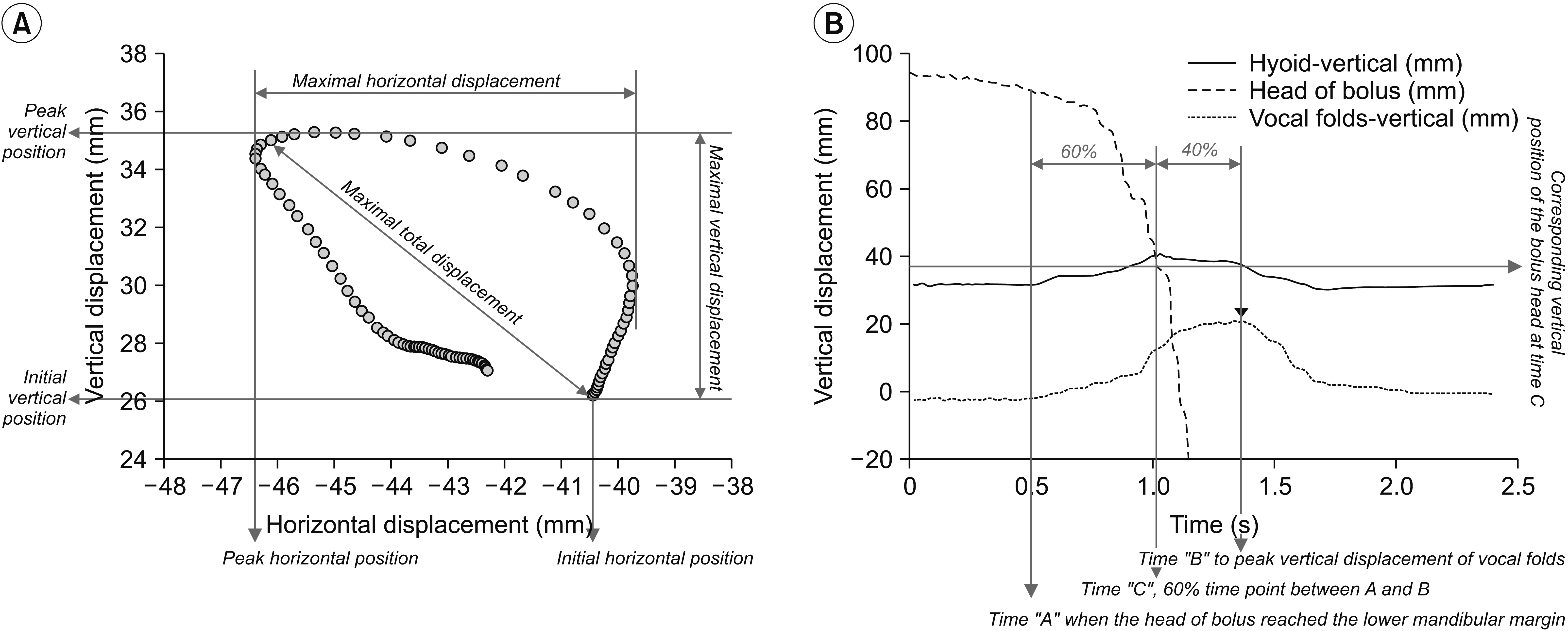
Swallowing was videofluoroscopically evaluated in 20 healthy volunteers in UP and LD postures, based on the movements of hyoid bone, vocal folds, and the bolus head. Parameters included the Penetration-Aspiration Scale (PAS), horizontal and vertical displacement, horizontal and vertical initial position, horizontal and vertical peak position, time to peak position of the hyoid bone and vocal folds, and pharyngeal transit time (PTT).
RESULTS
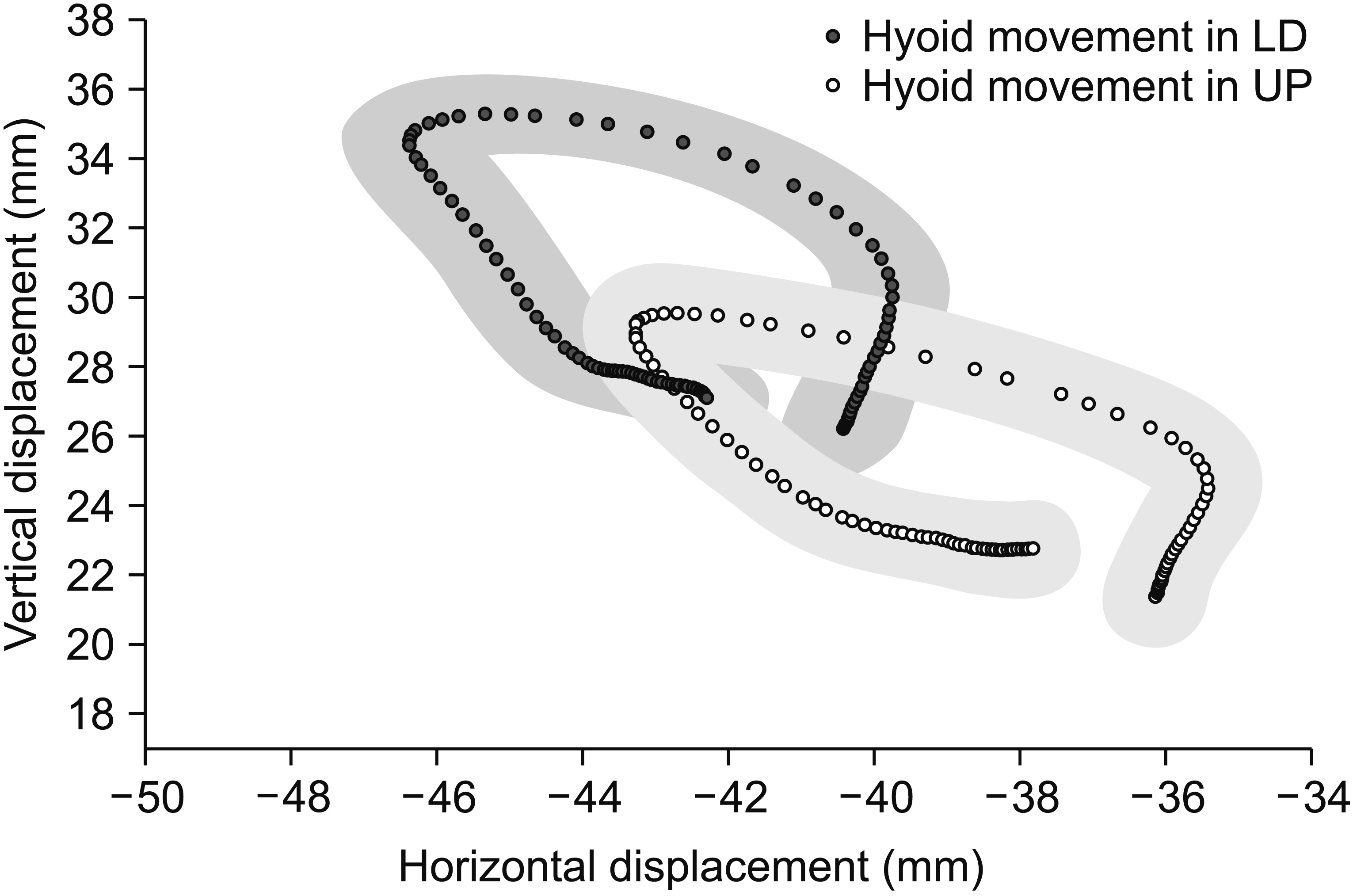
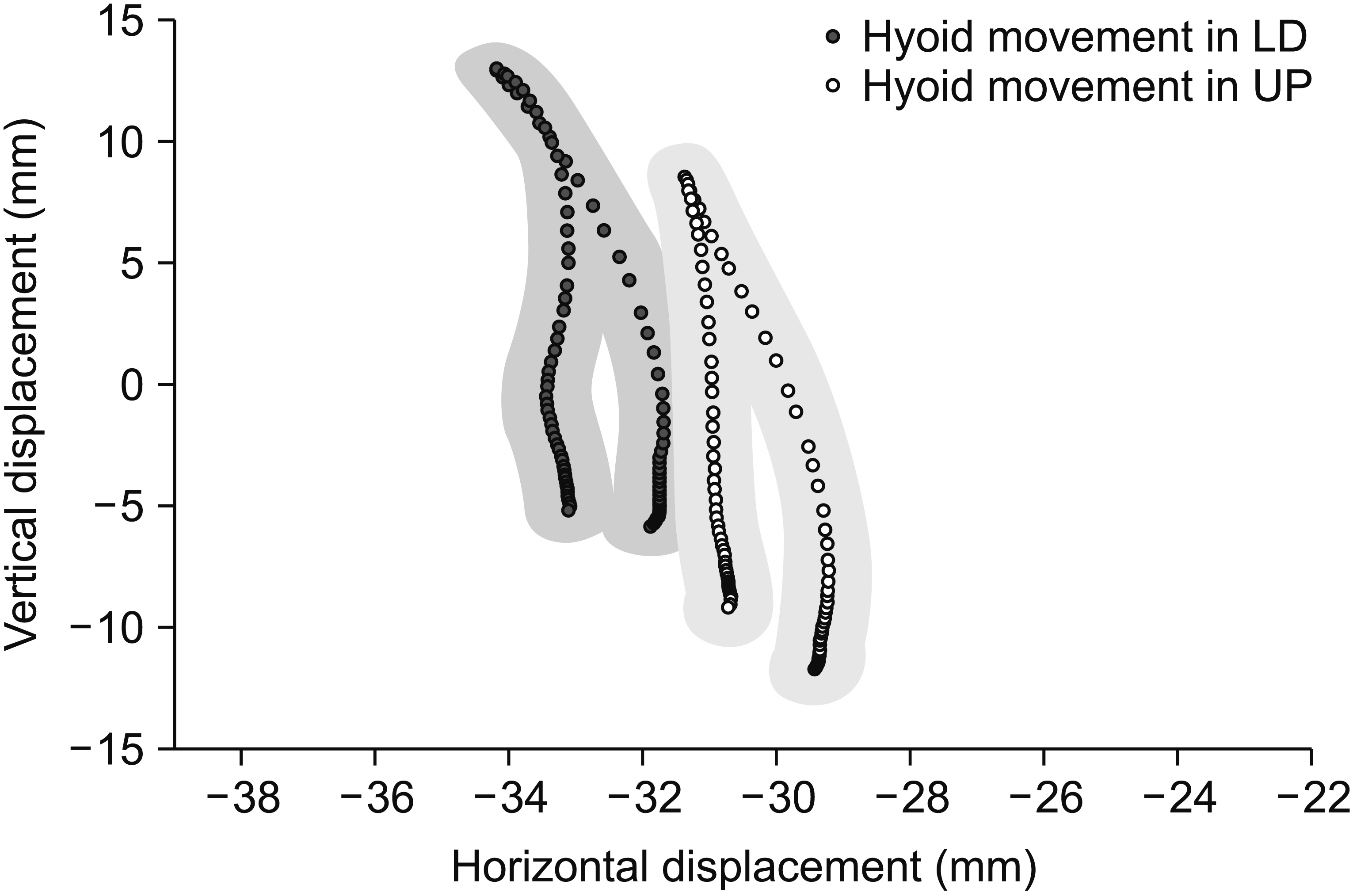
Nine participants were rated PAS 2 in the UP and 1 was rated PAS 2 in the LD (p=0.003) at least 1 out of 3 swallows each posture. The hyoid and vocal folds showed more anterior and superior peak and initial positions in the LD. In addition, swallowing resulted in greater vertical and smaller horizontal displacement of the hyoid in LD posture compared with UP. Time to peak position of the hyoid was shorter in LD. The maximal vertical and horizontal displacement of the vocal folds, and PTT were comparable between postures.
CONCLUSION
The results showed that the peak and initial positions of the hyoid and larynx and the pattern of hyoid movement varied significantly depending on the body postures. This study suggests that the LD posture was one of the safe feeding postures without any increased risk compared with UP posture.
MeSH Terms
Figure
Cited by 1 articles
-
Proportion of Aspiration Pneumonia Cases Among Patients With Community-Acquired Pneumonia: A Single-Center Study in Korea
Inpyo Jeon, Gwang Pyo Jung, Han Gil Seo, Ju Seok Ryu, Tai Ryoon Han, Byung-Mo Oh
Ann Rehabil Med. 2019;43(2):121-128. doi: 10.5535/arm.2019.43.2.121.
Reference
-
1. Ertekin C, Aydogdu I. Neurophysiology of swallowing. Clin Neurophysiol. 2003; 114:2226–44.
Article2. Oh TH, Brumfield KA, Hoskin TL, Stolp KA, Murray JA, Bassford JR. Dysphagia in inflammatory myopathy: clinical characteristics, treatment strategies, and outcome in 62 patients. Mayo Clin Proc. 2007; 82:441–7.
Article3. Seo HG, Oh BM, Han TR. Longitudinal changes of the swallowing process in subacute stroke patients with aspiration. Dysphagia. 2011; 26:41–8.
Article4. Park YH, Han HR, Oh BM, Lee J, Park JA, Yu SJ, et al. Prevalence and associated factors of dysphagia in nursing home residents. Geriatr Nurs. 2013; 34:212–7.
Article5. Achem SR, Devault KR. Dysphagia in aging. J Clin Gastroenterol. 2005; 39:357–71.
Article6. Kendall KA, Leonard RJ. Hyoid movement during swallowing in older patients with dysphagia. Arch Otolaryngol Head Neck Surg. 2001; 127:1224–9.
Article7. Tamura F, Shishikura J, Mukai Y, Kaneko Y. Arterial oxygen saturation in severely disabled people: effect of oral feeding in the sitting position. Dysphagia. 1999; 14:204–11.
Article8. Steele CM, Greenwood C, Ens I, Robertson C, Seidman-Carlson R. Mealtime difficulties in a home for the aged: not just dysphagia. Dysphagia. 1997; 12:43–51.
Article9. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2001; 24 Suppl 1:S40–101.10. Dejaeger E, Pelemans W, Ponette E, Vantrappen G. Effect of body position on deglutition. Dig Dis Sci. 1994; 39:762–5.
Article11. Barkmeier JM, Bielamowicz S, Takeda N, Ludlow CL. Laryngeal activity during upright vs. supine swallowing. J Appl Physiol (1985). 2002; 93:740–5.
Article12. Feng X, Cartwright MS, Walker FO, Bargoil JH, Hu Y, Butler SG. Ultrasonographic evaluation of geniohyoid muscle and hyoid bone during swallowing in young adults. Laryngoscope. 2015; 125:1886–91.
Article13. Perry JL, Bae Y, Kuehn DP. Effect of posture on deglutitive biomechanics in healthy individuals. Dysphagia. 2012; 27:70–80.
Article14. Su HK, Khorsandi A, Silberzweig J, Kobren AJ, Urken ML, Amin MR, et al. Temporal and physiologic measurements of deglutition in the upright and supine position with videofluoroscopy (VFS) in healthy subjects. Dysphagia. 2015; 30:438–44.
Article15. Inagaki D, Miyaoka Y, Ashida I, Yamada Y. Influence of food properties and body position on swallowingrelated muscle activity amplitude. J Oral Rehabil. 2009; 36:176–83.
Article16. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article17. Leigh JH, Oh BM, Seo HG, Lee GJ, Min Y, Kim K, et al. Influence of the chin-down and chin-tuck maneuver on the swallowing kinematics of healthy adults. Dysphagia. 2015; 30:89–98.
Article18. Bryant KN, Finnegan E, Berbaum K. VFS interjudge reliability using a free and directed search. Dysphagia. 2012; 27:53–63.
Article19. Torchiano M. effsize: Efficient Effect Size Computation [Internet]. [place unknown]: The R Foundation;2017. [cited 2018 May 1]. Available from: https://cran.r-project.org/web/packages/effsize/index.html.20. Standring S, Berkovitz BK, Ellis H, Gray H. Gray’s anatomy: the anatomical basis of clinical practice. 39th ed. Edinburgh: Churchill Livingstone;2005.21. Simental AA, Carrau RL. Assessment of swallowing function in patients with head and neck cancer. Curr Oncol Rep. 2004; 6:162–5.
Article22. Johnsson F, Shaw D, Gabb M, Dent J, Cook I. Influence of gravity and body position on normal oropharyngeal swallowing. Am J Physiol. 1995; 269(5 Pt 1):G653–8.
Article23. Robbins J, Coyle J, Rosenbek J, Roecker E, Wood J. Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia. 1999; 14:228–32.
Article24. Molfenter SM, Steele CM. Kinematic and temporal factors associated with penetration-aspiration in swallowing liquids. Dysphagia. 2014; 29:269–76.
Article25. Palermo P, Cattadori G, Bussotti M, Apostolo A, Contini M, Agostoni P. Lateral decubitus position generates discomfort and worsens lung function in chronic heart failure. Chest. 2005; 128:1511–6.
Article26. Teixeira AB, Mathias LA, Saad Junior R. The influence of posture on spirometric values in grade III obese patients. Rev Bras Anestesiol. 2011; 61:713–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in Hyolaryngeal Movement and Swallowing Function After Neuromuscular Electrical Stimulation in Patients With Dysphagia
- Influence of Supraglottic Swallow on Swallowing Kinematics: Comparison between the Young and the Elderly
- The Influence of Posture on Instability Evaluation Using Flexion–Extension X-Ray Imaging in Lumbar Spondylolisthesis
- Normative Temporal Data of Hyolaryngeal Movements during Swallowing
- Sonoanatomical Change of Phrenic Nerve According to Posture During Ultrasound-Guided Stellate Ganglion Block